Insulin Blood Test - Fasting Insulin Test in Hyderabad, India
PACE Hospitals offers advanced Fasting Insulin Test in Hyderabad, Telangana, India through our NABL - accredited laboratory. Our expert team ensures accurate detection of insulin levels, enabling timely diagnosis of diabetes and metabolic health concerns. With cutting-edge diagnostics and professional care, we help you achieve better health outcomes.
Book an appointment for
Fasting Insulin Test
Fasting Insulin Test Online Appointment
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Insulin Blood Test Preparation
No special preparation is required. However, follow any specific instructions given by your doctor.
What is a Insulin Blood Test?
An Insulin Blood Test measures the amount of insulin, an important hormone made by the pancreas and released into the bloodstream. Insulin helps move glucose (sugar) from the blood into cells, so the body can use it for energy. When insulin is working properly, blood sugar levels remain stable. If insulin levels are too high or too low, it can be a sign of underlying health issues like insulin resistance, diabetes, metabolic disorders or pancreatic disorders.
What is a fasting insulin test?
A fasting insulin test measures the concentration of insulin level in the blood after an overnight fast (typically 8 to 12 hours) when no food has been consumed. This gives a baseline (“steady state”) level of insulin secretion.
Insulin plays a key role primarily in carbohydrate metabolism and helps promote glucose storage in the liver, muscles, and fat tissue, which can contribute to overall weight gain. Because insulin influences a wide range of physiological processes, its production and balance are crucial in the development and progression of many chronic diseases.
Importance of an Insulin Blood Test
- When insulin doesn’t work properly, or the human body doesn’t make enough of it, blood sugar levels rise - leading to diabetes and other health problems.
- Measuring insulin in the blood provides critical insight into how the body regulates blood sugar. When insulin is either insufficient or ineffective, blood glucose levels rise, contributing to the development of different types of diabetes and related health issues.
- By understanding insulin levels, physicians and endocrinologists can identify and manage different forms of diabetes earlier and more effectively.
Different Types of Diabetes & the Role of Insulin
- Type 1 Diabetes (Juvenile Diabetes): The body’s immune system attacks the pancreas, destroying the cells that make insulin. People with type 1 diabetes always need insulin injections to survive.
- Type 2 Diabetes: The most common type of diabetes (90-95% of cases) and usually occurs after the age of 45 years. The body’s cells become resistant to insulin, so glucose can’t easily enter them. Over time, the pancreas gets tired of producing extra insulin, and blood sugar levels stay high. This involves insulin resistance, where cells become less responsive to insulin. Over time, β-cells wear out, reducing insulin output. Many patients eventually require insulin treatment. In the later stages, many people need insulin treatment.
- Maturity-Onset Diabetes of the Young (MODY): A rare, inherited form of diabetes caused by a gene problem that affects insulin production. People are usually young, of a healthy weight, and have family members with the same condition.
- Gestational Diabetes: It occurs during pregnancy and can affect the mother and baby if not managed. If diet and exercise don’t control blood sugar, insulin may be needed.
Benefits of a Fasting Insulin Test
The Fasting Blood Insulin Test measures how much insulin is present in blood after not eating for 8–12 hours.
- High fasting insulin may mean an individual's body is producing extra insulin to overcome insulin resistance - an early warning sign for type 2 diabetes, metabolic syndrome, or Polycystic Ovary Syndrome (PCOS).
- Low fasting insulin can indicate type 1 diabetes, late-stage type 2 diabetes, or other conditions where insulin production is impaired.
A fasting insulin test is an important way to check how well the body is producing insulin and controlling blood sugar. Endocrinologists recommend this test for several reasons:
Diagnosis: An insulin blood test can help identify the cause of symptoms related to low blood sugar (hypoglycemia), such as shaking, sweating, confusion, rapid heartbeat, or intense hunger. It can also assist in diagnosing conditions like insulin resistance, insulinoma (insulin-producing tumors), and pancreatic disorders.
Monitoring: The test can help monitor how well the pancreas is functioning, especially after procedures like islet cell transplants or the removal of an insulinoma. It also aids in tracking how the body responds to insulin and blood sugar levels in people with diabetes, guiding decisions about insulin therapy.
Screening: An Endocrinologist may use an insulin blood test to screen for blood sugar disorders such as prediabetes, type 2 diabetes, or gestational diabetes, even before symptoms appear.
General Health: Evaluating insulin levels can provide insights into overall metabolic and pancreatic health. It helps detect early signs of insulin resistance and assess the risk of developing Type 2 diabetes or other related complications.
Preparing for the Fasting Insulin Blood Test
While preparing for an insulin test is generally simple, following specific guidelines is crucial to ensure accurate and reliable results.
Fasting Rules followed for Insulin Blood Test Sample Collection
Fasting clears the effect of recent meals, giving a true baseline for blood sugar and insulin levels.
- 8–12 hours of fasting is usually required before blood sample collection.
- Only plain water is allowed during this time.
Morning appointments are best, as they use the body’s natural overnight fasting period.
Foods, Drinks, and Habits to Avoid Before the Test
- Individuals need to avoid all foods, sugary drinks, tea, coffee, alcohol, and juices.
- Other habits to avoid: Physical exercises, chewing gum and smoking, as both can interfere with fasting accuracy.
Talking to the Endocrinologist/Physician About Medications and Supplements
- Individuals need to write down all medications, vitamins, and supplements taken, including the drugs (like steroids, insulin, or oral diabetes medications), as they can alter the interpretation of the results.
- Patients need to discuss with the healthcare provider before the test about whether to pause, adjust, or continue them. They are advised not to make any changes self-way and always need to follow the Endocrinologist/Physician’s advice exactly.
What Happens During the Test
Step-by-Step Experience at the Clinic or Lab
- A healthcare professional will draw a blood sample from a vein (usually in the arm).
- If an oral glucose tolerance test (OGTT) is advised, drinking of a glucose solution, and additional samples will be collected at an interval of 30 minutes, 1 hour, 2 hours, and sometimes 3 hours are taken into consideration.
How Long Does It Take and What Individuals Might Feel
- A single fasting test takes just a few minutes.
- A glucose tolerance test may take 2–3 hours with multiple blood draws.
- During the test, a quick feeling of sting from the needle, and sometimes mild dizziness, may be noticed.
Fasting Insulin Test Results Interpretation
The ranges of healthy insulin and blood sugar help to evaluate how well the body manages blood sugar and how efficiently insulin is functioning. Fasting glucose and fasting insulin are two key indicators that, when interpreted together, provide a powerful snapshot of your overall metabolic health.
Insulin blood test normal range and blood sugar (glucose) normal range
Fasting Glucose Level
| Category | Range | What It Means |
|---|---|---|
| Normal | Less than 5.56 mmol/L (100 mg/dL) | Healthy blood sugar control: insulin is working effectively. |
| Prediabetes | 5.56 - 6.94 mmol/L (100-125 mg/dL) | “Warning zone” (impaired fasting glucose). Higher risk of developing Type 2 diabetes. |
| Diabetes | ≥ 7.0 mmol/L (126 mg/dL or higher on two separate tests) | Blood sugar is not controlled; diabetes is diagnosed. Medical treatment and lifestyle changes are needed. |
For healthy individuals, fasting blood sugar should be below 5.56 mmol/L. Levels between 5.56-6.94 mmol/L may suggest prediabetes, while 7.0 mmol/L or higher could indicate diabetes.
Fasting Insulin Level
| Category | Range | What It Means |
|---|---|---|
| Normal | Less than 25 mIU/L (varies slightly by lab) | Shows appropriate insulin production; cells are responding well. |
| Elevated | Greater than 25 mIU/L | Suggests insulin resistance. The pancreas is overworking to keep sugar in control, raising the risk of prediabetes or Type 2 diabetes. |
| Very Low | Significantly below normal | May indicate low or no insulin production (seen in Type 1 diabetes or late-stage Type 2 diabetes). |
In a simple way:
Glucose tells us how much sugar is in the blood.
Insulin tells us how hard the body is working to control that sugar.
When both are measured together, they provide a much clearer picture of metabolic health.
What High Levels May Indicate
- Insulin resistance
- Prediabetes or Type 2 diabetes
- Metabolic syndrome or weight-related issues
What Low Levels May Indicate
- Type 1 diabetes (low or no insulin production)
- Pancreatic dysfunction
- Hormonal imbalances
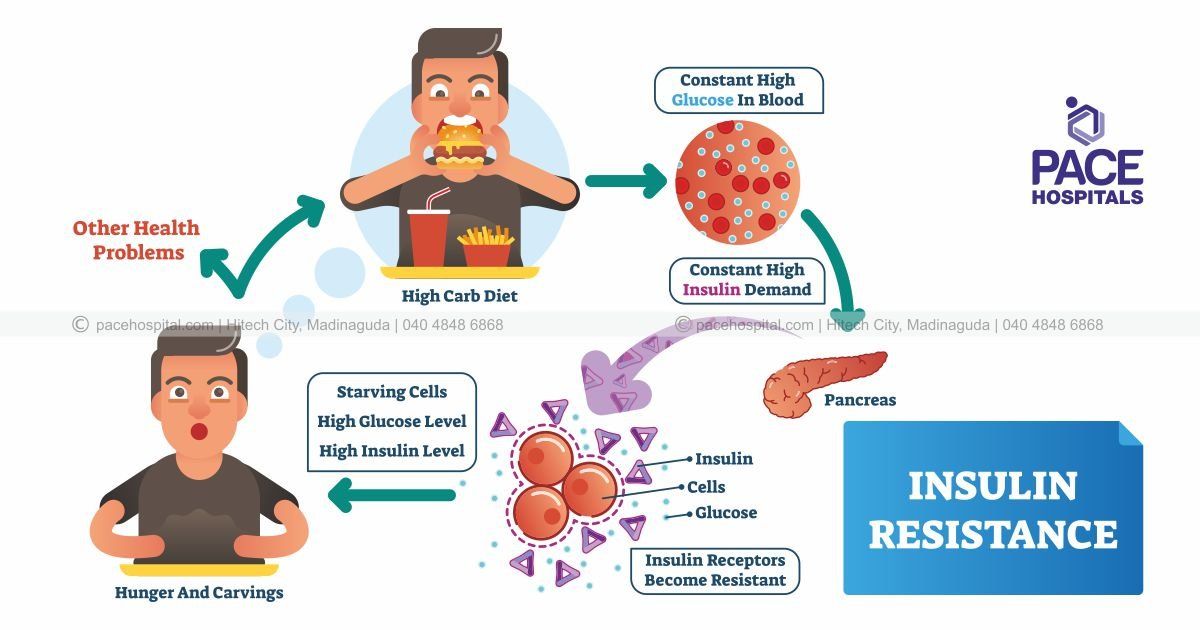
In some cases, the problem isn’t with producing insulin but with how the body uses it. This is known as insulin resistance. Here, cells stop responding effectively to insulin, causing blood sugar levels to remain high. In response, the pancreas keeps releasing more insulin to try to control glucose.
This ongoing battle - high blood sugar pushing for more insulin, and cells resisting its action - creates a vicious cycle. Over time, the pancreas becomes overworked and may lose its ability to produce insulin, setting the stage for Type 2 diabetes.
Too little insulin production leads to Type 1 diabetes or other hormonal/pancreatic disorders. Excess insulin due to resistance leads to Type 2 diabetes and metabolic complications.
Difference between Hypoglycemia and Hyperglycemia
Hypoglycemia vs Hyperglycemia
The body needs a careful balance of insulin to keep blood sugar within a healthy range. Too much or too little insulin - or the body’s inability to use it properly - can cause blood sugar to swing in either direction:
Hypoglycemia (Low Blood Glucose Levels)
Cause: Occurs when insulin (or diabetes medication) lowers blood sugar too much, or when the body produces too little glucose. More common in people taking insulin or certain diabetes drugs.
Symptoms:
- Shakiness, sweating, trembling
- Rapid heartbeat (palpitations)
- Hunger or nausea
- Irritability, confusion, or dizziness
- Blurred vision or headache
- In severe cases: seizures, unconsciousness may be observed
Complications if untreated:
Can lead to loss of consciousness, seizures, or coma.
Hyperglycemia (High Blood Glucose Levels)
Cause: Usually happens when there isn’t enough insulin, or when the body’s cells don’t respond to insulin (insulin resistance). This is commonly linked to Type 2 diabetes.
Symptoms:
- Increased thirst (polydipsia)
- Frequent urination (polyuria)
- Blurred vision
- Fatigue or weakness
- Slow-healing cuts or infections
- Headaches
Complications if untreated:
Nerve damage, kidney problems, eye disease, and risk of heart disease.
Symptoms of Low Insulin Production
When the pancreas fails to make enough insulin (common in Type 1 diabetes):
- Persistently high blood sugar (hyperglycemia)
- Unexplained weight loss
- Excessive thirst and urination
- Fatigue despite eating normally
- Increased hunger but low energy
Symptoms of Insulin Resistance
When the body makes insulin, but the cells do not respond properly (common in Type 2 diabetes and prediabetes):
- High fasting insulin levels but normal or slightly elevated glucose initially
- Cravings for sugar and carbs
- Fatigue, especially after meals
- Weight gain, especially around the belly
- Dark, velvety patches of skin (acanthosis nigricans)
- Gradual rise in blood sugar leading to prediabetes/diabetes
Insulin Blood Test Types
The fasting blood insulin test can be performed in different ways, depending on what the endocrinologist is trying to check. Here are the main types:
| Type of Test | Purpose | How It’s Done |
|---|---|---|
| Simple Fasting Insulin Test/ Basic Fasting Insulin Test/ Fasting Serum Insulin Test | Measures baseline insulin levels after 8-12 hours of fasting | A single blood sample is taken after overnight fasting. |
| Fasting Insulin with Glucose - Homeostatic Model Assessment of Insulin Resistance (HOMA-IR Test) | Evaluates insulin resistance (how well the body responds to insulin) | Both fasting insulin and fasting glucose are measured, and a formula (HOMA-IR) is used to calculate insulin resistance. |
| Glucose Tolerance Test with Insulin (GTT with Insulin) | Checks how insulin responds after glucose intake | Blood samples are taken at fasting, then at 30 min, 1 hr, 2 hrs, and 3 hrs after drinking a glucose solution. |
| Fasting Insulin with HbA1c (glycated hemoglobin) | Provides a long-term picture of blood sugar control along with insulin function | Both fasting insulin and HbA1c (3-month average blood sugar) are measured. |
| Fasting Insulin with C-Peptide Test | Helps determine if the pancreas is producing insulin properly | Measures both insulin and C-peptide (a marker of natural insulin production). Useful in differentiating Type 1 vs. Type 2 diabetes. |
In brief:
- A basic fasting insulin test or fasting serum insulin test gives you a snapshot of insulin at rest.
- Insulin random blood test measures insulin levels at any time of the day, without requiring fasting. It is often paired with a glucose test to assess how well the body is producing and releasing insulin.
- More advanced versions (like HOMA-IR or GTT with insulin) tell how the body handles sugar and whether an individual may have insulin resistance, prediabetes, or diabetes.
Fasting Blood Insulin Tests Explained for Different Symptoms Observed
Doctors or Endocrinologists may recommend different types of fasting insulin tests depending on symptoms, risk factors, or existing health conditions. Here’s what patients need to know:
| Type of Tests Recommended | Symptoms Observed by Individuals | What It Means for |
|---|---|---|
| Basic Fasting Blood Insulin Test or Fasting Serum Insulin Test - Measures serum insulin concentration after 8-12 hours of fasting using immunoassay methods (e.g., ELISA, RIA, or chemiluminescence). | If noticing tiredness, weight gain, frequent urination, or a family history of diabetes | Detects hyperinsulinemia, early insulin resistance, or pancreatic beta-cell dysfunction. |
| Fasting Insulin with Glucose - Homeostatic Model Assessment for Insulin Resistance Test (HOMA-IR Test) Formula: HOMA-IR = (Fasting Glucose × Fasting Insulin) ÷ 405. | If being overweight, have PCOS, or early signs of metabolic syndrome | High HOMA-IR indicates reduced insulin sensitivity and a higher risk of Type 2 diabetes, metabolic syndrome, and cardiovascular disease. |
| Glucose Tolerance Test with Insulin (GTT with Insulin) | If having unexplained fatigue, sugar cravings, or borderline diabetes. Serial measurement of plasma insulin and glucose levels at 0, 30, 60, 120, and 180 minutes after ingestion of a 75 g oral glucose load. | Identifies impaired glucose tolerance, prediabetes, Type 2 diabetes, and gestational diabetes. |
| Fasting Insulin with HbA1c Measures fasting serum insulin alongside glycated hemoglobin (HbA1c) | If already having diabetes or prediabetes | Combines current insulin levels with 3-month average blood sugar. Helps Endocrinologists/ Physicians to fine-tune treatment plan. |
| Fasting Insulin with C-Peptide (a cleavage product of proinsulin secreted in equimolar amounts with insulin) | Differentiates endogenous insulin production from exogenous insulin therapy. | Helps distinguish between Type 1 diabetes (low or no insulin production) and Type 2 diabetes (insulin resistance). |
Simple Takeaway for Patients
- If the physician or endocrinologist advises a fasting insulin test, it’s to check how the body is handling sugar.
- Different versions of the test give different insights - from early warning signs (insulin resistance) to managing existing diabetes more effectively.
Factors That Can Influence the Insulin Blood Test - Fasting Insulin Test
Factors like diet, stress, sleep quality, hormonal changes, and medications can all significantly impact fasting insulin and glucose results - so proper preparation and physician guidance are essential. Below are some of the factors that can influence blood insulin test results:
- Recent diet & lifestyle: Heavy meals or excess sugar before fasting can alter baseline insulin and glucose levels, reducing test accuracy.
- Stress & sleep: Stress and poor sleep increase cortisol and catecholamine release, which can temporarily raise blood glucose and insulin levels.
- Hormonal changes: Pregnancy and hormonal fluctuations (e.g., PCOS, thyroid dysfunction) can affect insulin sensitivity and fasting test results.
- Medications: Certain drugs, including corticosteroids, diuretics, and hormonal therapies, can raise blood glucose and interfere with accurate insulin assessment.
Precautions Required for Insulin Blood Test - Fasting Insulin Test
When to Seek Medical Advice
- Abnormal test results (either high or low values) should be reviewed by a healthcare provider.
- Early intervention is critical in preventing long-term complications.
Lifestyle Changes That Can Improve Insulin Levels
- Regular exercise and daily physical activity
- Balanced diet with controlled carbohydrates
- Weight management
- Good quality sleep and stress control
Follow-Up Tests and Monitoring
- Endocrinologists may recommend repeat fasting tests, HbA1c, oral glucose tolerance test, or HOMA-IR calculation to track long-term health.
Fasting insulin and blood sugar tests are powerful tools for early detection of diabetes and insulin resistance. Following proper preparation steps ensures accurate results. With early awareness, lifestyle adjustments, and medical support, long-term health risks can be significantly reduced.
Frequently Asked Questions (FAQs) on Insulin Blood Test - Fasting Insulin Test
Does an Insulin Blood Test Require Fasting?
Yes. Most insulin blood tests, especially the fasting insulin test, require fasting for 8-12 hours. Only plain water is allowed. Fasting ensures that food or drinks don’t affect blood sugar and insulin levels, giving an accurate baseline result.
How to Test Blood Sugar for Insulin Resistance?
Insulin resistance cannot be detected with a simple blood sugar test alone. Endocrinologists often rely on specialized tests that measure both insulin and glucose levels to get a clearer picture. One common method is the HOMA-IR test, which combines fasting insulin and fasting glucose to assess how well the body is responding to insulin. Another approach is the Oral Glucose Tolerance Test with Insulin (OGTT + Insulin), where insulin and glucose levels are measured at set intervals after drinking a glucose solution. These tests help reveal how insulin and glucose interact in the body, making it possible to detect early stages of insulin resistance even before blood sugar levels become abnormal.
What to Avoid During Fasting Blood Test?
To ensure accurate results from a fasting insulin blood test, avoid eating or drinking anything - this includes water with additives, tea, coffee, juice, alcohol, and sugary beverages - for at least 8 to 12 hours before the test. Even small amounts of food or drink can alter blood sugar and insulin levels, potentially leading to misleading results. In addition to dietary restrictions, it's also important to avoid smoking, chewing gum, and engaging in physical activity during the fasting period, as these habits can interfere with the accuracy of the test.
How Often Should a Person Get a Fasting Insulin Test?
The need for fasting insulin tests depends on your individual health circumstances. If having conditions such as diabetes, prediabetes, PCOS, metabolic syndrome, or are at risk for insulin resistance, healthcare provider may recommend regular testing to monitor changes and guide treatment decisions. For individuals without known risk factors, a fasting insulin test might be done periodically as part of a comprehensive metabolic assessment.
What Conditions Other Than Diabetes Can an Insulin Test Detect?
The test may also help detect:
- Insulinoma (a rare insulin-producing tumor in the pancreas)
- Pancreatic disorders affecting insulin production
- Hormonal or metabolic imbalances
Can an Individual Take Insulin Before a Fasting Blood Test?
No. If a person on insulin therapy, should not take insulin injection before the test unless the physician or endocrinologist specifically advises it. Taking insulin beforehand may alter test results. Always follow the specialist instructions regarding medications before testing.
Is There a Blood Test for Insulin Levels?
Yes. The Insulin Blood Test measures the amount of insulin in the blood. It can be done after fasting (to check baseline levels), during an Oral Glucose Tolerance Test (OGTT) to see how the body responds to sugar, or along with HbA1c to assess long-term blood sugar control. This test helps detect insulin resistance, prediabetes, or diabetes earlier than glucose tests alone.
Is there any Insulin Resistance blood test?
Yes. The most used is the HOMA-IR Test, which uses both fasting glucose and fasting insulin to calculate insulin resistance. Another option is the Glucose Tolerance Test with Insulin (measuring insulin response after a glucose drink).
Can a Person Test Insulin Levels Through a Blood Test?
Yes, insulin levels can be measured directly from a blood sample taken from a vein. In the lab, techniques such as ELISA, RIA, or chemiluminescence are commonly used to estimate insulin levels. This test helps doctors evaluate insulin production and detect conditions like insulin resistance or diabetes.
How to Measure Insulin Content in Blood Without doing Blood Test?
Currently, there is no non-invasive test to measure insulin levels directly. Insulin can only be measured through a blood test. However, blood sugar monitoring devices (glucometers or CGMs) help track glucose, which indirectly reflects insulin function.
How To Test Blood Insulin Level?
A blood sample is taken, usually after fasting, and analyzed in a lab.
Options include:
- Fasting Insulin Test
- HOMA-IR Test (with glucose)
- Glucose Tolerance Test with Insulin
- Insulin with C-Peptide Test
Is There a Blood Test to Check for Insulin Resistance?
Yes. The most widely used is the HOMA-IR Test. It combines fasting glucose and insulin to assess how well the body responds to insulin. OGTT with Insulin is another method to check how the body reacts after glucose intake.
What is Insulin Random Blood Test?
Unlike the fasting test, the Random Insulin Test measures insulin levels at any time of the day, regardless of when what consumed. It’s less commonly used but may help in certain cases, such as checking insulinoma or unusual glucose fluctuations.
Why is the Insulin Blood Test Important if Blood Sugar is Normal?
Even if blood sugar is normal, high insulin levels may indicate insulin resistance - an early warning sign for Type 2 diabetes, PCOS, or metabolic syndrome. Detecting this early helps prevent future complications.