Gastroparesis Treatment in Hyderabad, India
PACE Hospitals is renowned as the Best hospital for Gastroparesis treatment in Hyderabad, India, offering advanced care for patients with delayed gastric emptying and related digestive conditions. Our team of experienced gastroenterologists specializes in managing complex cases, including diabetic gastroparesis, with precision and care.
At PACE Hospitals, we provide personalized treatment plans focused on long-term relief, improved gastric health, and better quality of life.
Book an Appointment for Gastroparesis Treatment
Gastroparesis Treatment Online Appointment
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Why Choose PACE Hospitals for Gastroparesis Treatment?
Advanced Diagnostic Facilities: Endoscopy, Gastric Emptying Scintigraphy, Ultrasound & Blood Tests for accurate Gastroparesis evaluation
Gastroparesis specialists with vast experience in diagnosing and managing mild to severe Gastroparesis
Minimally Invasive & Advanced Treatment Approaches: Endoscopic therapies, pyloric injection, gastric electrical stimulation, laparoscopic pyloroplasty
Affordable & Transparent Gastroparesis Treatment at PACE Hospitals with Insurance & Cashless Options
Gastroparesis Diagnosis
Diagnosis of gastroparesis may depend on factors such as medical history and physical examination, which help the gastroenterologist accurately diagnose the condition. A gastroenterologist considers the following before selecting the appropriate tests to diagnose gastroparesis:
- Medical history
- Physical examination
Medical history
When assessing a patient for gastroparesis, it is important to gather a thorough medical history. Focusing on early signs of gastroparesis, like nausea, vomiting of undigested food, bloating, abdominal pain, early fullness, and unintentional weight loss, is important. It is vital to note when these symptoms started and how long they last after meals.
The gastroenterologist may ask questions about any history of diabetes mellitus, connective tissue or neurological disorders, prior abdominal surgeries, and use of medications known to delay gastric emptying, such as opioids, anticholinergics, or certain diabetes medications. Dietary habits, including meal size and frequency, as well as recent changes in diet, need to be reviewed.
In addition, family history of any gastrointestinal or motility disorders, and lifestyle factors like alcohol or smoking are relevant. It is also vital to identify any alarming signs, such as gastrointestinal bleeding, rapid weight loss, or signs of obstruction, which may suggest alternative diagnoses. This comprehensive history helps to guide further diagnostic evaluation and management of suspected gastroparesis.
Physical examination
The physical examination in the evaluation of gastroparesis is often nonspecific but plays a crucial role in supporting the diagnosis, ruling out other causes, and identifying complications. On examination, patients may appear thin or malnourished if symptoms are chronic and severe. The abdomen is usually soft, but mild upper abdominal distension or tenderness may be present, especially in the epigastric region. Visible peristalsis or a succussion splash may rarely be detected if there is significant gastric retention.
A gastroenterologist also checks for signs of dehydration, such as dry skin or mucous membranes. Importantly, the physical exam also focuses on excluding signs of acute abdomen, peritonitis, or palpable masses, which would suggest alternative diagnoses such as mechanical obstruction or malignancy. In general, while the physical findings in gastroparesis are often subtle, a careful examination helps assess the severity of illness, nutritional status, and the need for urgent intervention.
Diagnostic Tests of Gastroparesis
A gastroenterologist may suggest specific diagnostic tests to check stomach emptying and find possible underlying causes based on the information given. To identify gastroparesis, the following tests may be recommended:
- Laboratory tests
- Imaging studies
- Endoscopic evaluation
- Tests to measure stomach emptying
Laboratory tests
While gastric emptying studies are the primary procedure to diagnose gastroparesis, laboratory tests help identify underlying conditions such as diabetes, infections, or metabolic disorders that may cause or aggravate the condition.
The following laboratory tests are commonly performed in the evaluation of gastroparesis:
- Complete blood count (CBC)
- Metabolic panel
- Blood glucose
- Liver function test (LFT)
- Lipase
- Urine test
Complete blood count: This test measures the number of red blood cells, white blood cells, and platelets. It is indicated to evaluate for anaemia (which can occur in gastroparesis patients due to malnutrition or other underlying illnesses) and to detect signs of infection or inflammation (reflected by an elevated white blood cell count) that may occur with complications or help rule out other causes of symptoms.
Metabolic panel: This panel checks levels of electrolytes, kidney function, and blood glucose. It is used to detect electrolyte imbalances and dehydration (which can result from persistent vomiting seen in gastroparesis), as well as to assess for hyperglycaemia or hypoglycaemia important because diabetes is a major cause, and blood sugar fluctuations can impact gastric emptying.
Blood glucose: The blood glucose test is performed to identify diabetes mellitus, which is a common underlying cause of gastroparesis. Measuring fasting blood glucose or glycated haemoglobin (HbA1c) helps determine whether hyperglycaemia may be contributing to delayed gastric emptying. Good glycaemic control is important for both diagnosing and managing gastroparesis in patients with diabetes.
Liver function test: This group of tests measures liver enzymes and bilirubin. LFTs help to rule out liver disease as a potential cause of gastrointestinal symptoms similar to those seen in gastroparesis.
Lipase: A blood test measuring the pancreatic enzyme lipase is often recommended to help rule out pancreatitis as the cause of symptoms such as nausea, vomiting, and abdominal discomfort, since these symptoms can resemble those of gastroparesis. Elevated lipase levels are a key indicator of acute pancreatitis and can help distinguish it from other conditions with similar presentations.
Urine test: A urine test is not used to diagnose gastroparesis directly, but it plays an important supportive role in the diagnostic process. The urine test is performed to identify signs of dehydration, kidney problems, infection, or diabetes, which are potential complications of gastroparesis or alternative diagnoses that may resemble its symptoms.
Imaging studies
Imaging tests may reveal problems that could be causing symptoms, such as intestinal or stomach blockages. A gastroenterologist may perform the following tests:
- Upper gastrointestinal (GI) series
- Gastric ultrasonography (GUS)
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI)
Upper gastrointestinal series: This test involves the patient swallowing a barium-containing liquid, followed by a series of X-rays to visualise the oesophagus, stomach, and duodenum. In addition to helping identify anatomical abnormalities such as tumors, strictures, or ulcers that may produce symptoms like gastroparesis, the upper GI series can demonstrate delayed stomach emptying. Instead of making a direct diagnosis of gastroparesis, its main objective is to rule out mechanical obstruction.
Gastric ultrasonography (GUS): Gastric ultrasound is a non-invasive imaging can help detect structural abnormalities, such as tumors or thickening of the stomach wall, and, in some cases, estimate gastric emptying by measuring changes in gastric volume after a meal. However, it is not a standard diagnostic tool for gastroparesis and is mainly used to exclude other causes of symptoms.
Computed tomography (CT) scan: Abdominal CT scans give cross-sectional images of the organs. It assists in locating masses, blockages, or other intra-abdominal conditions that might resemble gastroparesis. Complications like bezoars or stomach distension can also be found using CT scans. Similar to the other imaging tests, CT is not used to confirm gastroparesis, but rather to rule out structural reasons.
Magnetic resonance imaging (MRI): MRI produces high-resolution images of the abdominal organs. It helps exclude structural abnormalities or masses that could cause delayed gastric emptying. In some specialised centres, MRI can also be used to assess gastric motility, but this is not widely available. The primary role of MRI in this context is to rule out other causes of symptoms, rather than to diagnose gastroparesis directly.
Endoscopic evaluation
Endoscopic evaluation can be used to assist in ruling out obstructive etiologies in patients with suspected gastroparesis.
Upper GI endoscopy: Upper GI endoscopy does not directly diagnose gastroparesis; its role is to rule out mechanical obstructions or other structural issues in the esophagus, stomach, and duodenum that could mimic gastroparesis symptoms. While retained food in the stomach after fasting might suggest delayed emptying, this finding is not specific enough for a definitive diagnosis.
Tests to measure stomach emptying
To diagnose gastroparesis, tests are performed to objectively measure the rate at which the stomach empties its contents, as the condition is characterised by delayed gastric emptying in the absence of mechanical obstruction.
- Scintigraphic gastric emptying scan (GES)
- Gastric emptying breath test (GEBT)
- Antroduodenal manometry
- Wireless motility capsule (WMC)
Scintigraphic gastric emptying scan (GES): GES is the gold standard for diagnosing gastroparesis. In this test, the patient consumes a solid or liquid meal containing a small amount of radioactive material, and a special camera is used to measure how quickly the stomach empties the meal. The amount of food remaining in the stomach after four hours is used to assess the severity of delayed gastric emptying: less than 15% retention indicates mild gastroparesis, 15–35% retention indicates moderate, and more than 35% retention indicates severe gastroparesis.
Although some centres measure gastric emptying after two hours, the four-hour measurement is considered more accurate. In certain cases, a liquid meal is added to the study to improve sensitivity in detecting gastroparesis when solid emptying appears normal.
Gastric emptying breath test (GEBT): The gastric emptying breath test diagnoses gastroparesis by assessing the rate of gastric emptying. A meal containing carbon-13 is given, and breath samples are analyzed over time to measure carbon-13 exhalation. Delayed release of carbon-13 indicates impaired gastric emptying, consistent with gastroparesis. In patients with lung or liver disease, GEBT use is limited.
Antroduodenal manometry: Antroduodenal manometry is used to diagnose gastroparesis by measuring the coordination and strength of muscle contractions in the stomach and duodenum. A catheter is inserted to record pressure patterns during fasting and after eating. This test helps identify abnormal motility patterns, such as antral hypomotility or uncoordinated contractions, which can cause delayed gastric emptying and symptoms of gastroparesis. It is useful in distinguishing gastroparesis from other motility disorders when the cause of symptoms is unclear.
Wireless motility capsule (WMC): The wireless motility capsule diagnoses gastroparesis by measuring the time it takes for the stomach to empty. The capsule is swallowed and records when it leaves the stomach. A delayed transit time indicates gastroparesis. This test is also known as SmartPill.
Gastroparesis Stages
Gastroparesis is commonly classified into three stages based on symptom severity, the degree of delayed gastric emptying, and complications:
- Mild Gastroparesis: The stomach empties slowly, but symptoms are mild or minimal, usually not significantly affecting daily life.
- Moderate Gastroparesis: The stomach empties more slowly, symptoms become more noticeable, affecting eating habits and causing discomfort.
- Severe Gastroparesis: There is marked impairment in stomach emptying, leading to severe symptoms such as dehydration, malnutrition, and significant weight loss, severely impacting quality of life.
Gastroparesis Differential Diagnosis
A gastroenterologist may consider a broad differential diagnosis in patients presenting with nausea and vomiting. The following conditions can present similarly to gastroparesis:
- Functional dyspepsia: It is a condition that presents chronic upper abdominal discomfort, bloating, early satiety, and nausea, similar to gastroparesis.
- Gastric outlet obstruction: This refers to a physical blockage at the distal stomach or proximal duodenum, often due to peptic ulcer disease, malignancy, or strictures. It causes symptoms like nausea, vomiting, and abdominal distension, but unlike gastroparesis, the obstruction is mechanical and can be identified on imaging or endoscopy.
- Cyclical vomiting syndrome: It is characterized by recurrent, stereotypical episodes of severe nausea and vomiting separated by symptom-free intervals. Unlike gastroparesis, gastric emptying is typically normal between episodes, and the pattern is more episodic rather than chronic.
- Psychiatric disorders: There are some conditions, such as anxiety, depression can manifest with gastrointestinal symptoms, including nausea and vomiting. These symptoms are not due to delayed gastric emptying but rather to psychological factors.
- Cannabinoid hyperemesis syndrome: This happens when prolonged cannabis use can cause episodic vomiting, accompanied by a tendency for hot showers to aid symptom relief; symptoms improve with the cessation of cannabis.
- Rumination syndrome: This is a behavioural disorder that consists of daily, effortless regurgitation of undigested food after ingestion of a meal. In contrast to gastroparesis, it is not preceded by nausea or vomiting.
Gastroparesis Treatment Goals
The main goals of treating gastroparesis are to
- Reduce symptoms like nausea and vomiting
- Improve nutritional and fluid deficiencies
- Identify and address any underlying causes, such as diabetes or specific medications
- Prevent complications such as Severe protein-calorie malnutrition, Bezoar formation requiring surgical resection, Mallory-Weiss tears, and frequent hospital visits.
A gastroenterologist may choose the treatment depending on the cause, the severity of the symptoms, and whether complications are present or not. In some cases, treating the cause can cure gastroparesis. And if the cause of gastroparesis is unknown, treatment is provided to help relieve symptoms and manage complications. Below are the treatment options for gastroparesis:
Non-pharmacological therapy
- Lifestyle and dietary modifications
- Controlling blood glucose levels
- Avoiding drugs that cause gastroparesis
- Nutritional support
- Patient education
Pharmacological therapy
- Antiemetics
- Prokinetic agents
- Dopamine-D2 antagonist
- Macrolide antibiotics
- Pain medicines
- Antidepressants
Endoscopic management
- Gastric peroral endoscopic myotomy (G-POEM)
- Pyloric botulinum toxin injection
- Pyloric balloon dilation
Surgical interventions
- Jejunostomy tube feeding
- Gastric electrical stimulation
- Venting gastrostomy
Non-pharmacological therapy
Non-drug therapies are usually the first choice for treating gastroparesis. They concentrate on changes in diet and lifestyle to ease symptoms and speed up gastric emptying without using medications.
- Lifestyle and dietary modification: Dietary modification is an initial step in managing gastroparesis. Patients are suggested to eat small, frequent meals that are low in fat and fibre because these macronutrients slow gastric emptying and can worsen symptoms. A “small particle” (soft or liquid) diet is often better tolerated and more likely to relieve symptoms and improve gastric emptying. Sitting upright after meals and maintaining adequate hydration are also recommended lifestyle adjustments. Quitting alcohol and smoking may improve delayed gastric emptying.
- Controlling blood glucose levels: For patients with diabetic gastroparesis, keeping blood glucose levels under control is crucial. High blood sugar can delay gastric emptying and make symptoms worse. Strict blood sugar management can help lessen the severity of gastroparesis and prevent complications. This is supported by both clinical guidelines and research, which show that improved glucose control can lead to better gastric motility and symptom management.
- Avoiding drugs that cause gastroparesis: The most important aspect of treating gastroparesis is avoiding drugs that may cause or worsen the illness, particularly when drug-induced gastroparesis is present. Drugs such as opioids, certain anticholinergics, some diabetes medications (like GLP-1 receptor agonists), and specific antidepressants are known to slow gastric emptying and may aggravate symptoms. Clinical guidelines recommend that healthcare experts carefully review a patient’s medication list and discontinue or substitute these drugs whenever possible to help improve gastric motility and reduce symptoms.
- Nutritional support: Nutritional support is important to prevent malnutrition and dehydration, especially in moderate to severe cases. If oral intake is inadequate, enteral nutrition (such as jejunal tube feeding) is considered; parenteral nutrition is reserved for the rarest, most severe cases. Ensuring sufficient calorie, protein, and micronutrient intake reduces morbidity and supports healing.
- Patient education: Patients need to receive thorough instruction regarding dietary and lifestyle changes, such as eating multiple small meals daily and abstaining from alcohol, tobacco, and carbonated beverages. The patient's quality of life is negatively impacted by gastroparesis because of the chronic nature of the symptoms and the absence of effective treatment alternatives.
Pharmacological therapy
Pharmacological therapy is considered when lifestyle changes and diet changes do not relieve symptoms of gastroparesis. Certain drugs are used to improve gastric motility, relieve symptoms, and speed up gastric emptying.
Pharmacological approaches for the treatment of gastroparesis include:
- Antiemetics: Antiemetics are commonly utilised to manage the chronic nausea and vomiting that often accompany gastroparesis. These drugs function by obstructing the brain signals that cause nausea and the urge to vomit. They can reduce these symptoms, assisting patients in maintaining improved nutrition and hydration, even if they do not treat the underlying root cause of delayed stomach emptying.
- Prokinetic agents: Prokinetic medications are important for treating gastroparesis because they increase the stomach's normal muscle contractions. These medications help the stomach empty its contents more efficiently into the small intestine. By improving gastric motility, prokinetic agents can reduce symptoms such as bloating, early satiety (feeling full quickly), and abdominal discomfort, and may also help with associated nausea.
- Dopamine-D2 antagonist: Dopamine-D2 antagonists are a specific type of prokinetic medication that work by blocking dopamine receptors in the digestive tract and the brain. This action not only stimulates the muscles of the stomach to contract and move food along, but also helps reduce nausea and vomiting. These medications are often chosen when both improved gastric emptying and symptom control are needed.
- Macrolide antibiotics: Macrolide antibiotics are sometimes used to treat gastroparesis because they can stimulate stomach muscle contractions by acting as motilin receptor agonists. This reliefs symptoms like bloating and nausea and speeds up stomach emptying. However, because of the possibility of adverse effects and their gradual decline in efficacy, their usage is typically restricted to short-term or intermittent therapy. Patients who are unable to take prokinetic medicines and dopamine-D2 antagonists are treated with macrolide antibiotics.
- Pain medicines: Pain medicines may be used in cases where abdominal pain is a significant symptom of gastroparesis. However, the choice of pain medication is important, as some types can further slow gastric emptying and worsen symptoms. Therefore, non-opioid pain relievers are generally preferred, and pain management is approached cautiously and individually.
- Antidepressants: Antidepressants, second-line therapy, particularly at low doses, are sometimes used in gastroparesis to help manage chronic pain and persistent nausea. These medications can influence how the nervous system processes pain and discomfort, and may also help with the psychological burden of living with a chronic digestive disorder. They are used carefully, as higher doses or certain types can have side effects that might negatively impact gastric motility.
Endoscopic management
Endoscopic therapy is an emerging option for patients with gastroparesis who have persistent, refractory symptoms despite medical and dietary treatment.
- Gastric peroral endoscopic myotomy (G-POEM): Gastric peroral endoscopic myotomy (G-POEM) is a minimally invasive endoscopic procedure that involves cutting the muscles of the pylorus (the valve at the stomach’s exit). By relaxing this muscle, G-POEM can improve gastric emptying and relieve symptoms in patients with severe gastroparesis who have not responded to other treatments.
- Pyloric botulinum toxin injection: Botulinum toxin injection involves endoscopically injecting botulinum toxin into the pyloric sphincter, the muscle at the outlet of the stomach. The toxin temporarily relaxes this muscle, which can help improve gastric emptying and relieve symptoms.
- Pyloric balloon dilation: Balloon dilatation of the pylorus is another endoscopic procedure where a balloon is inserted and inflated at the pyloric sphincter to stretch and widen the opening. This can help food pass more easily from the stomach into the small intestine, potentially improving symptoms in some patients with gastroparesis.
Surgical interventions
When medicinal and dietary treatments fail to manage severe, refractory symptoms in patients with gastroparesis, surgery may be considered.
Gastroparesis surgery includes:
- Jejunostomy tube feeding: A feeding tube is inserted straight into the jejunum, a section of the small intestine, during jejunostomy tube feeding. For individuals who are unable to accept oral intake because of severe gastroparesis, this enables nourishment to completely avoid the stomach. It reduces symptoms like bloating and vomiting while ensuring proper nutrition and hydration.
- Gastric electrical stimulation: Gastric electrical stimulation is a procedure where a small device is surgically implanted into the stomach wall. In certain patients with drug-induced gastroparesis, this device can help reduce symptoms like nausea and vomiting by providing slight electrical pulses to the stomach muscles. Although it may not work for everyone, some people may benefit from it.
- Venting gastrostomy: Venting gastrostomy involves placing a tube into the stomach to allow for the release of air and fluids. This procedure helps relieve symptoms of severe bloating, nausea, and vomiting by decompressing the stomach. It is often used for symptom management in patients with refractory gastroparesis.
Gastroparesis Prognosis
The prognosis of gastroparesis depends on its cause and severity. Many patients experience persistent symptoms and poor quality of life, but in some, especially those with diabetes, symptoms can remain stable over time and do not necessarily increase mortality.
However, more severe cases often seen in tertiary care centers may lead to serious complications, with some patients requiring long-term nutritional support and a small percentage facing increased risk of death. Post-viral gastroparesis generally has a better outlook, often improving within a year. Overall, more community-based studies are needed to understand long-term outcomes fully.
Gastroparesis Treatment Cost in Hyderabad, India
The cost of Gastroparesis Treatment in Hyderabad generally ranges from ₹3,000 to ₹38,000 (approx. US $36 – US $455).
The exact gastroparesis treatment cost varies depending on factors such as the severity of delayed gastric emptying, underlying cause (diabetes, nerve dysfunction, post-surgical issues), need for diagnostic tests (endoscopy, gastric emptying study, ultrasound), requirement for IV medications, hospital admission, diet therapy, and hospital facilities — including cashless treatment options, TPA corporate tie-ups, and assistance with medical insurance wherever applicable.
Cost Breakdown According to Type of Gastroparesis Treatment
- Outpatient Consultation + Basic Medication – ₹3,000 – ₹6,000 (US $36 – US $72)
- Diagnostic Evaluation (CBC, Electrolytes, Ultrasound Abdomen) – ₹2,000 – ₹6,000 (US $24 – US $72)
- Upper GI Endoscopy for Evaluation – ₹8,000 – ₹15,000 (US $96 – US $180)
- Gastric Emptying Study (Scintigraphy Test) – ₹12,000 – ₹22,000 (US $145 – US $265)
- Day-Care IV Fluids + Prokinetic Therapy – ₹5,000 – ₹12,000 (US $60 – US $145)
- Hospital Admission for Moderate to Severe Gastroparesis – ₹18,000 – ₹38,000 (US $215 – US $455)
Frequently Asked Questions (FAQs) on Gastroparesis Treatment
How is gastroparesis treated?
Gastroparesis is a disorder described by slowed stomach emptying when there isn't a mechanical barrier. This may lead to symptoms such as nausea, vomiting, early satiety, bloating, and abdominal pain. Treatment typically involves dietary modifications (such as small, low-fat, low-fibre meals), blood glucose control in diabetic patients, prokinetic and antiemetic medications, and, in severe cases, nutritional support or surgical interventions.
Which Is the best hospital for Gastroparesis Treatment in Hyderabad, India?
PACE Hospitals, Hyderabad, is one of the leading centres for gastroparesis diagnosis and treatment, offering comprehensive care for delayed gastric emptying and severe digestive motility disorders.
We render best service under the guidance of reputed gastroenterologists and digestive motility specialists as they evaluate underlying causes, provide targeted medical therapy, endoscopic assessment, customised diet planning, and long-term management for diabetic, idiopathic, and post-surgical gastroparesis in a proper manner.
We have dedicated team and provide advanced endoscopy suites, nuclear medicine support for gastric emptying studies, modern day-care units, personalised diet counselling, and round-the-clock emergency support, PACE Hospitals ensures safe, effective, and patient-focused gastroparesis management — supported by cashless treatment options, TPA corporate tie-ups, and assistance with medical insurance documentation.
What causes gastroparesis?
Gastroparesis can be caused by a variety of factors, including diabetes (the most common cause), post-viral syndromes, certain medications that slow gastric motility, surgeries that affect the stomach or vagus nerve, and idiopathic (unknown) reasons.
Is gastroparesis fatal?
Gastroparesis is generally not considered a fatal condition. But severe cases can lead to serious complications such as malnutrition, dehydration, and electrolyte imbalances, which may be life-threatening if not properly managed. Mortality rates are higher in patients with severe, refractory gastroparesis, particularly those requiring long-term nutritional support, but overall, gastroparesis itself is not typically fatal.
What is the difference between diabetic gastropathy and gastroparesis?
Diabetic gastropathy is a broad term for various stomach nerve and muscle problems in diabetes, including abnormal contractions. Gastroparesis is a specific condition defined by objectively delayed stomach emptying without a blockage.
What Is the cost of Gastroparesis Treatment at PACE Hospitals, Hyderabad?
At PACE Hospitals, Hyderabad, the cost of gastroparesis treatment typically ranges from ₹2,800 to ₹32,000 and above (approx. US $34 – US $385), making it an affordable and comprehensive option for gastrointestinal motility care. However, the final cost depends on:
- Severity of symptoms (vomiting, bloating, fullness, weight loss)
- Underlying cause (diabetes, idiopathic, post-surgical)
- Type of treatment required (oral medications / IV therapy / endoscopy)
- Need for gastric emptying study or ultrasound scan
- Diet counselling and nutrition correction
- Duration of hospital stay (if required)
- Follow-up consultations and long-term management
For mild cases requiring outpatient care and diet management, costs remain at the lower end; moderate to severe cases requiring diagnostic tests, IV therapy, or hospitalisation fall toward the higher range.
After a detailed gastroenterology evaluation, imaging review, gastric motility assessment, and treatment planning, our specialists will provide a personalised treatment plan and transparent cost estimate tailored to your medical needs.
What is the survival rate for people with gastroparesis?
Studies show that people with gastroparesis have a lower 5-year survival rate (67%) compared to the general population (81%). Mortality is higher among older patients and those with comorbidities, with an overall rate of about 3.19 per 1000 patients. Delayed gastric emptying is an independent predictor of increased mortality, highlighting the significant health burden of gastroparesis and the need for careful management.
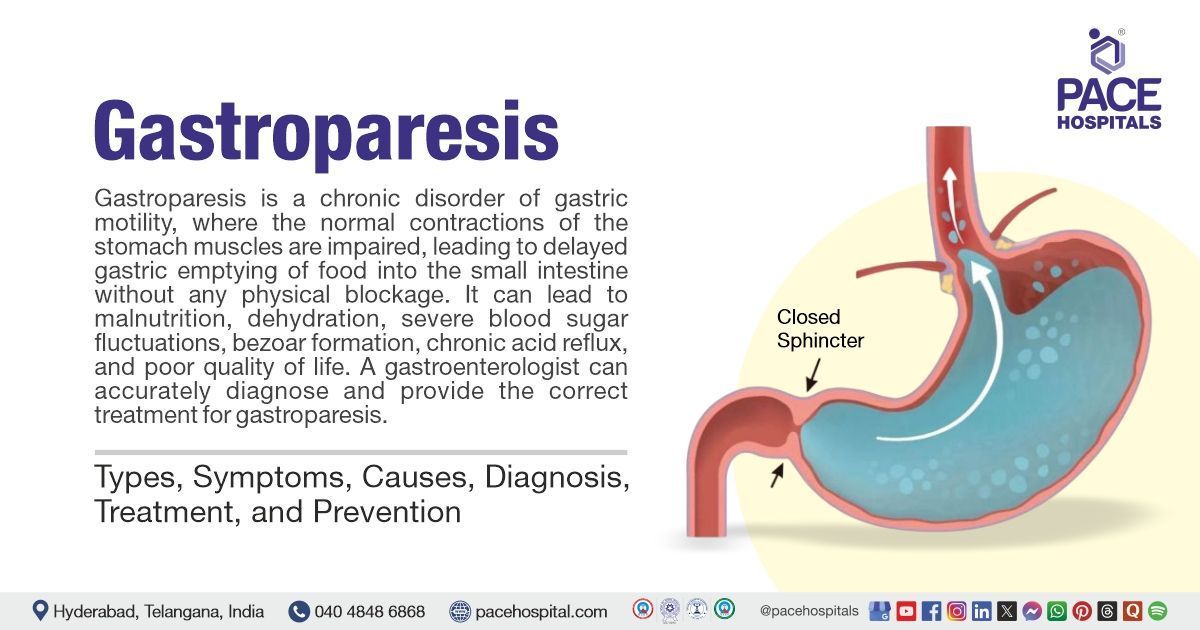
What is gastroparesis?
Gastroparesis means "partially paralysed stomach." It refers to a condition where the stomach muscles do not function properly, resulting in delayed movement of food from the stomach to the small intestine without any physical blockage.
How does gastroparesis affect blood sugar?
Gastroparesis can result in delayed and inconsistent nutrient absorption, which can cause blood glucose levels to fluctuate. People with diabetes are especially affected by this since it can make controlling blood sugar more challenging and raise the risk of both hyperglycaemia and hypoglycaemia.
How does alcohol affect gastroparesis?
Alcohol can worsen gastroparesis by impairing gastric motility and damaging the nerves that control stomach muscles. Chronic alcohol use may exacerbate symptoms and contribute to the development or progression of gastroparesis.
What is diabetic gastroparesis?
Diabetic gastroparesis is a form of gastroparesis that occurs as a complication of diabetes, most often due to long-term high blood sugar levels damaging the vagus nerve, which controls stomach muscles. It is characterized by delayed gastric emptying and the typical symptoms of gastroparesis, and it can make blood glucose management more challenging.
Can someone get disability for gastroparesis?
Yes, Gastroparesis is considered a disabling condition. If symptoms are severe enough to significantly limit daily activities and the ability to work. The severity of symptoms, the effect on nutritional status, and the responsiveness to treatment all affect eligibility for disability benefits. Disability claims usually involve evidence of functional limitations and documentation from healthcare experts.
Do digestive enzymes help with gastroparesis?
There is no strong evidence that the use of digestive enzymes is beneficial in the treatment of gastroparesis. Gastroparesis is primarily a disorder of gastric motility, not enzyme deficiency, so enzyme supplements are not generally recommended.
Does exercise help gastroparesis?
Light to moderate physical activity, such as walking after meals, may help stimulate gastric motility and improve symptoms in some individuals with gastroparesis. However, there is limited high-quality evidence, and exercise needs to be tailored to individual tolerance and overall health status.
What to eat with gastroparesis?
The gastroparesis diet focuses on eating small, frequent meals that are low in fat and fiber, as these are easier to digest and less likely to delay gastric emptying. Pureed or liquid foods are often better tolerated. High-fat and high-fibre foods, carbonated beverages, and tough meats need to be avoided.
Can gastroparesis turn into cancer?
There is no evidence to suggest that gastroparesis leads to or increases the risk of cancer. Gastroparesis is a disorder of stomach motility and is not considered a precancerous condition.
Can gastroparesis cause bad breath?
Yes, delayed gastric emptying may lead to the retention of food in the stomach, which can ferment and produce unpleasant odours that may be expelled as bad breath. This association is noted in clinical observations, although it is not unique to gastroparesis and can be seen in other gastrointestinal disorders as well.