Diverticulosis Disease Treatment | Diagnosis & Cost
PACE Hospitals is renowned as the best hospital for diverticulosis disease treatment in Hyderabad, India, providing advanced care for conditions such as colonic diverticulosis, sigmoid diverticulosis, and spastic diverticulosis. Our team of the best gastroenterologists specializes in accurate diagnosis using techniques like colonoscopy, CT scan, and imaging studies. Treatment options include personalized dietary guidance, medications to manage symptoms, and minimally invasive procedures when required, ensuring effective relief and long-term digestive health.
Book an Appointment for Diverticulosis Disease Treatment
Diverticulosis Treatment Online Appointment
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Why Choose PACE Hospitals for Diverticulosis Diagnosis and Treatment?

Advanced Diagnostic Facilities: Endoscopy, High-Resolution Manometry, pH Monitoring & Biopsy for accurate Esophagitis detection
Expert Gastroenterologist in Hyderabad dedicated to comprehensive Esophagitis care
Minimally invasive approaches for severe Esophagitis treatment, including endoscopic therapy, laparoscopic surgery, balloon dilation, radiofrequency ablation
Affordable & Transparent Esophagitis Treatment at PACE Hospitals with Insurance & Cashless Options
Diverticulosis Diagnosis
Diagnosing diverticulosis involves a structured evaluation by gastroenterologists to detect the presence of diverticula, small pouches in the colon wall, because abdominal pain from diverticulosis may be asymptomatic or mimic other gastrointestinal conditions. Gastroenterologists follow a methodical approach to confirm the diagnosis. The aim is to visualize the diverticula, assess for any complications, and differentiate between diverticulosis and diverticulitis.
A comprehensive clinical evaluation supports the diagnosis of diverticulosis by identifying potential symptoms and evaluating for complications. However, since most cases of diverticulosis are asymptomatic, it is often diagnosed incidentally during colonoscopy or imaging studies.
The gastroenterologist considers the following before selecting the appropriate tests to diagnose diverticulosis:
- Medical history
- Physical examination
Medical history
A thorough medical history is taken at the start of the evaluation. Most patients are asymptomatic, but some may report vague, intermittent left lower quadrant abdominal discomfort, bloating, changes in bowel habits (constipation or diarrhoea), or episodes of painless rectal bleeding. Risk factors include older age, low-fibre diet, obesity, sedentary lifestyle, smoking, and family history of diverticular disease. In the presence of complications such as diverticulitis or diverticular bleeding, history may reveal acute, persistent pain, fever, or significant rectal bleeding.
Physical examination
On physical examination, uncomplicated diverticulosis usually presents with normal findings and no specific abnormalities. Localized abdominal discomfort, usually in the left lower quadrant, may be discovered during the examination if complications are present. In extreme situations, symptoms of peritoneal irritation, such as rebound discomfort, rigidity, or guarding, may be observed. When there is severe rectal bleeding, the patient may show symptoms of pallor or hypovolemia. Physical findings are generally more pronounced when complications arise, and the examination helps guide the need for further diagnostic testing, such as colonoscopy or diverticulosis radiology (e.g., CT Scan), to confirm the diagnosis and assess for complications.
Diagnostic Tests of Diverticulosis
Based on the above, a gastroenterologist may suggest a series of diagnostic tests to identify diverticulosis-related issues, malignancies, or infections. They include the following:
Laboratory tests
Laboratory testing plays an essential role in the diagnosis and proper treatment of diverticulosis symptoms. Diverticulosis can also be diagnosed using endoscopy or imaging; however, laboratory tests can be performed to detect complications, such as bleeding, inflammation, or infection. When diverticulitis or other problems are suspected, these tests are especially helpful. Patients with complex diverticulosis or those suspected of having it frequently undergo the following laboratory tests:
- Complete blood count (CBC)
- C-Reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
- Faecal calprotectin (FC)
- Blood Urea Nitrogen (BUN) and Creatinine
- Blood Cultures
- Faecal occult blood test (FOBT)
Complete blood count (CBC): A CBC analysis includes various blood components, like platelets, white blood cells (WBCs), and red blood cells. In uncomplicated diverticulosis, the CBC is usually normal. But in patients with diverticulitis (inflammation or infection of the diverticula), an increased WBC count may be seen, indicating an inflammatory or infectious disease. In cases of significant diverticular bleeding, haemoglobin and haematocrit may be decreased, indicating blood loss.
C-Reactive protein (CRP): C-Reactive Protein (CRP) is an inflammatory marker that increases in response to inflammation or infection. In uncomplicated diverticulosis, CRP levels are generally normal. An elevated CRP strongly suggests acute diverticulitis or another inflammatory process. It is a useful tool for identifying any difficulties and directing additional research, even though it is not unique to diverticulitis.
Erythrocyte sedimentation rate (ESR): The Erythrocyte Sedimentation Rate (ESR) is another non-specific blood test that indicates inflammation. It may be elevated in diverticulitis (inflammation of diverticula).
Faecal calprotectin (FC) : This is a non-invasive marker of intestinal mucosal inflammation, primarily used to distinguish inflammatory bowel diseases (IBD) from functional disorders, such as irritable bowel syndrome.
Blood Urea Nitrogen (BUN) and Creatinine: These tests evaluate kidney function. In patients with diverticulosis, significant diverticular bleeding can lead to blood loss and dehydration, resulting in reduced blood flow (perfusion) to the kidneys. This can cause elevations in creatinine and BUN levels, indicating impaired renal function. Monitoring these values is important for assessing the severity of bleeding and guiding fluid replacement therapy.
Blood Cultures: Blood cultures are obtained if a patient with suspected diverticulitis presents with signs of systemic infection or sepsis, such as high fever, hypotension, or altered mental status. This test helps detect bacteria in the bloodstream and assists in selecting appropriate antibiotic therapy if bacteraemia is present.
Faecal occult blood test: The FOBT detects hidden (occult) blood in the stool. While diverticulosis can cause painless rectal bleeding, a positive FOBT is not specific to diverticulosis and may also indicate colorectal cancer, polyps, or other gastrointestinal disorders. Although primarily used for colorectal cancer screening, it may incidentally detect bleeding related to diverticula.
Imaging studies
The primary approaches for identifying distal colonic diverticulosis are imaging studies, which are also critical in assessing its complications. Imaging can directly visualise the diverticula and check for indications of inflammation, infection, or other problems, unlike clinical evaluation or laboratory testing.
Computed tomography (CT): A CT scan of the abdomen and pelvis is considered the gold standard for assessing complications of diverticulosis, especially acute diverticulitis. CT imaging provides direct visualization of segmental colitis associated with diverticulosis, revealing small colonic outpourings. CT imaging is highly sensitive for detecting inflammation, such as peri colonic fat stranding, perforation, bowel wall thickening, or abscesses. CT is also effective in identifying other complications, which may include fistulas and bowel obstruction.
Ultrasound scan: Ultrasound can sometimes detect moderate diverticulosis, but it is less sensitive than CT for diagnosing uncomplicated diverticulosis. Its main role is in evaluating suspected diverticulitis, particularly in patients where radiation exposure needs to be avoided, such as pregnant women or young adults. Ultrasound can reveal bowel wall thickening, inflamed pericolic fat, and fluid collections, which are suggestive of diverticulitis. However, its accuracy depends on the operator’s skill and can be limited by patient body habitus or bowel gas.
Magnetic resonance imaging (MRI): MRI is not routinely used for the initial diagnosis of diverticulosis but serves as an excellent alternative in complicated cases, particularly when radiation exposure is a concern (such as in pregnant women or patients with recurrent disease). MRI offers high soft tissue resolution, enabling detailed visualisation of diverticula, bowel wall thickening, peri colonic fat stranding, and abscesses. However, it is less widely available, more expensive, and takes longer to perform compared to CT.
Abdominal X-ray: Abdominal X-ray is not a reliable method for diagnosing diverticulosis. Plain abdominal X-rays generally provide limited information and are nonspecific for identifying diverticulosis or diverticulitis. The primary role of abdominal X-ray is to look for complications such as perforation (evidenced by free air under the diaphragm) or bowel obstruction.
Endoscopic evaluation
Colonoscopy: Diverticula are sac-like protrusions in the colon that can be directly seen during a colonoscopy. It is recommended for the evaluation of unexplained gastrointestinal bleeding to confirm diverticulosis and to rule out cancer. Colonoscopy needs to be avoided during acute diverticulitis due to the risk of colonic perforation. In some cases, colonoscopy may also be used to treat diverticular bleeding through endoscopic interventions.
Additionally, mild papan coloniciverticulosis is often first suspected or diagnosed during colonoscopy or imaging performed for other indications, such as colorectal cancer screening or evaluation of rectal bleeding. Imaging and endoscopy are not required in asymptomatic individuals, unless indicated for other diagnostic or therapeutic reasons.
Stages of Diverticulosis
Diverticulosis is categorised according to whether it is currently asymptomatic or has progressed to diverticulitis, as well as whether complications are present.
The stages are as follows:
Type 0: Asymptomatic diverticulosis
Small pouches (diverticula) form in the colon wall, frequently in the sigmoid colon. Most people remain asymptomatic, and the condition is often found incidentally during a colonoscopy or imaging performed for other reasons. No specific treatment is needed in the absence of symptoms or complications. However, a high-fibre diet may be recommended to support overall colonic health and potentially reduce the risk of progression or complications.
Type I: Acute uncomplicated diverticulitis
This stage involves inflammation of the diverticula, but without complications such as perforation, abscess or obstruction. Symptoms may include left lower quadrant abdominal pain, low-grade fever, and changes in bowel habits. Management usually includes a clear liquid diet, oral antibiotics, and dietary modification, such as increasing fibre once acute symptoms resolve. Low-fibre or processed foods need to be avoided to reduce the recurrence risk.
Type II: Acute complicated diverticulitis
This stage occurs when diverticula become inflamed, leading to complications such as abscesses, perforations, fistulas, or bowel obstructions. Patients who are present with severe sigmoidal diverticulosis, accompanied by symptoms such as fever, marked left lower abdominal pain, nausea, and sometimes signs of peritonitis. This stage may require intravenous antibiotics, hospitalisation, and surgical intervention in severe cases.
Type III: Chronic diverticular disease
Some patients develop recurrent or severe diverticulitis, leading to prolonged inflammation. Complications may include bowel obstruction, fistulas, colonic wall scarring and strictures. In severe or treatment-resistant cases, surgical resection of the affected colon segment may be needed.
Diverticulosis Differential Diagnosis
Diagnosing diverticulosis can be complex because its symptoms, such as rectal bleeding or abdominal pain, overlap with several other gastrointestinal conditions. A gastroenterologist usually distinguishes diverticulosis from disorders like hemorrhoids, colonic polyps, colorectal cancer, and inflammatory bowel disease, as these can present similarly on imaging or colonoscopy. Other potential causes, including infections, ischemic colitis, and various sources of gastrointestinal bleeding or inflammation, also need to be considered.
A gastroenterologist usually combines clinical data and diverticulosis radiology to determine the exact reason behind symptoms. Which includes:
- Hemorrhoids: These are swollen veins in the anus or rectum that commonly cause painless rectal bleeding, itching, or discomfort, especially during bowel movements. Unlike diverticulosis, haemorrhoids do not cause abdominal pain or systemic symptoms and are usually diagnosed by physical examination or anoscopy.
- Ulcers in the gut wall (gastrointestinal ulcers): Colonic or gastric ulcers can cause abdominal pain and gastrointestinal bleeding similar to diverticulosis. However, ulcers are often associated with risk factors like NSAID use, Helicobacter pylori infection, or stress, and may present with more persistent pain or signs of perforation.
- Inflammatory bowel disease (IBD): Diseases such as ulcerative colitis and Crohn’s disease can be confused with diverticulosis, with symptoms like diarrhea, abdominal pain, and rectal bleeding. IBD may also present with chronic symptoms, extraintestinal manifestations, and specific endoscopic and histological findings that differentiate it from diverticulosis.
- Anal fissure: These are small tears in the lining of the anus, causing bleeding and sharp pain during defecation. Unlike diverticulosis, the bleeding is usually minimal and associated with defecation, and there are no systemic symptoms or abdominal pain.
- Anal abscess or fistula: These are infections or abnormal tracts near the anus, often presenting with localized pain, swelling, and sometimes discharge. While they can cause perianal discomfort and bleeding, they are distinguished from diverticulosis by their localized symptoms and physical examination findings.
- Colonic polyps: These are growths on the inner lining of the colon that may cause intermittent rectal bleeding, but are usually asymptomatic. They are usually found accidentally during a colonoscopy and do not typically cause abdominal pain or inflammation, unlike diverticulosis.
- Colon cancer: Colon cancer and diverticulosis can present with rectal bleeding and changes in bowel habits. However, colon cancer may also cause unexplained weight loss, persistent abdominal pain, and iron deficiency anaemia, and is diagnosed by colonoscopy and biopsy.
- Chronic constipation: This causes abdominal discomfort and straining, which may also contribute to the development of diverticulosis. However, constipation itself does not cause the formation of diverticula or the associated complications and is diagnosed based on clinical history.
- Angiodysplasias: This is an abnormal, fragile blood vessel in the gastrointestinal tract, most commonly found in the colon and small intestine. They are a frequent cause of unexplained gastrointestinal bleeding and anaemia, especially in older adults.
- Colitis: This is inflammation of the colon, which can result from infections, inflammatory bowel disease, ischemia, or as a side effect of radiation therapy. Symptoms commonly include diarrhoea, abdominal pain, rectal bleeding, and urgency.
- Proctitis: This is the inflammation of the rectal lining, which frequently manifests as urgency, bleeding, rectal pain, and occasionally discharge. It may be brought on by radiation therapy (radiation proctitis), inflammatory bowel disease, or viruses. Radiation-induced proctitis occurs when pelvic radiation damages the rectal mucosa, leading to acute or chronic symptoms, including ulceration and bleeding.
Considerations of a Gastroenterologist Before Treatment
A gastroenterologist manages patients with diverticulosis or diverticular disease by taking into account the patient's symptoms, risk of complications, food preferences, and general health. In general, recommendations emphasise increasing dietary fibre, encouraging regular physical activity, and supporting proper hydration. Along with providing personalised guidance based on the patient's medical history and comorbidities, the gastroenterologist also looks out for any indications of problems, such as diverticulitis or bleeding.
Diverticulosis Treatment Goals
The overall treatment goal for diverticulosis is to prevent complications, minimize symptoms, and promote long-term colon health. Diverticulosis management focuses on prevention and risk reduction, as the condition is often asymptomatic and discovered incidentally.
The main goals of diverticulosis treatment are:
- Relieve symptoms (if present): The majority of diverticulosis patients have no symptoms and do not need special care. The goal is to reduce mild symptoms, such as changes in bowel habits or abdominal pain, usually by increasing dietary fibre and drinking enough water.
- Prevention of complications: The primary aim is to reduce the risk of developing diverticulitis (inflammation or infection of diverticula), bleeding, or perforation. This is achieved through lifestyle and dietary modifications that support colon health and decrease colonic pressure.
- Promote bowel health: Encouraging a high-fibre diet, regular physical activity, and proper hydration helps maintain normal bowel function, reduces constipation, and may help prevent the formation of new diverticula or slow the worsening of existing ones.
- Prevent recurrence of complications: For patients who have experienced diverticulitis or diverticular bleeding, the goal is to prevent recurrence. This may involve ongoing dietary management, reviewing medication use (such as avoiding unnecessary NSAIDs), and, in select cases, considering surgical intervention for recurrent or severe disease.
- Avoid unnecessary interventions: Since uncomplicated diverticulosis is often harmless, the goal is to avoid unnecessary medications or procedures unless symptoms or complications arise. Surveillance and intervention are reserved for those with persistent symptoms or complications.
- Reserve surgery for complications: Surgery is considered only in cases of recurrent diverticulitis, persistent symptoms despite medical management, or in emergencies such as perforation or abscess formation.
The treatment of diverticulosis depends on the patient's symptoms, the level of inflammation or infection, and any present complications. Several options are available for managing symptomatic diverticulosis and its complications:
The approach generally includes:
- Non-pharmacological treatment
- Pharmacological treatment
- Surgical interventions (if needed)
Non-pharmacological treatment
Lifestyle and dietary management are the first and most important steps in treating diverticulosis. A high-fibre diet (25–35 grams per day) from fruits, grains, vegetables, and legumes helps soften stool, reduce pressure in the colon, and prevent complications. Patients are advised to avoid foods, particularly those with low fibre, high fat, or high red meat content. Adequate hydration supports fibre function and prevents constipation. Regular physical activity, like walking, jogging or yoga, improves bowel motility.
Establishing a routine bowel habit, especially after meals, can aid in natural digestion. Other helpful changes include quitting smoking, maintaining a healthy weight, and avoiding NSAIDs, which may increase the risk of bleeding or inflammation. These measures promote long-term colon health and reduce symptoms.
- Managing symptoms: Increased fibre consumption and proper hydration are typically used to alleviate moderate symptoms, such as bloating, mild abdominal discomfort, or irregular bowel movements. Since NSAIDs may raise the risk of bleeding or diverticulitis, analgesics, which are preferable over NSAIDs, can be taken to relieve pain if symptoms continue.
- Avoiding NSAIDs: People with diverticulosis are advised to avoid non-steroidal anti-inflammatory drugs (NSAIDs), as well as opioid painkillers, because these medications can increase the risk of serious complications. NSAIDs can irritate the lining of the colon and may lead to diverticular bleeding or even perforation (a tear in the colon wall). Opioids, on the other hand, slow down bowel movements and can cause constipation, which raises pressure in the colon and may trigger inflammation or perforation. Safer alternatives are generally recommended for pain relief in patients with diverticulosis.
- Patient education: Patients must fully understand their condition, including what diverticulosis is, how it affects their digestive health, and what lifestyle and dietary changes are most essential to prevent complications. Patients must be made aware of their treatment options, including the advantages of a high-fiber diet and drinking enough water, as well as the possible negative effects of some drugs, particularly NSAIDs, which might raise the risk of problems. Additionally, patients need to be aware of warning indications that point to the need for immediate to seek medical attention immediately, such as fever, acute or ongoing abdominal pain, or notable changes in bowel habits. For patients to identify early warning signals and seek prompt treatment, education may also address the spectrum of diverticulosis and diverticulitis symptoms, from minor pain to severe problems.
Pharmacological Treatment
Medications are used selectively, mainly for symptom relief or when dietary measures are insufficient.
- Fibre supplements: These drugs, which include bulk-forming laxatives, function by making stool more substantial and containing more water. This promotes regular bowel movements and reduces straining by softening the stool and making it easier to pass. By preventing constipation and reducing pressure within the colon, fibre supplements help manage symptoms such as bloating and discomfort, and are thought to reduce the risk of diverticula becoming inflamed.
- Pain management: For mild abdominal pain or discomfort associated with diverticulosis, analgesics are used. They provide symptomatic relief by reducing pain signals. Importantly, NSAIDs are generally avoided because they can increase the risk of diverticular bleeding or trigger diverticulitis.
- Antispasmodics: Antispasmodics are sometimes used in the management of diverticulosis to help relieve symptoms such as abdominal cramps, bloating, and discomfort. These medications reduce colon spasms by relaxing the smooth muscles of the gastrointestinal tract. Antispasmodics can lessen the cramping and pain that certain diverticulosis patients feel by reducing these muscle spasms, particularly when symptoms are brought on by irregular bowel movements or elevated colonic pressure. It's important to note that antispasmodics do not treat the underlying diverticula or prevent complications; their role is limited to providing symptomatic relief in selected patients.
- Antibiotics: Antibiotics are not indicated for uncomplicated diverticulosis and are used selectively in cases of uncomplicated diverticulitis, primarily for higher-risk patients such as those who are immunocompromised, have significant comorbidities, or show clear signs of infection. Recent clinical evidence suggests that many patients with mild, uncomplicated diverticulitis who are otherwise healthy do not benefit from routine antibiotic therapy, as antibiotics do not significantly speed recovery or prevent complications in these cases. Supportive care and close monitoring are enough. However, antibiotics are essential for complicated diverticulitis with abscesses, perforation or systemic infections, where the risk of serious complications is high. This approach helps to reduce unnecessary antibiotic use, reduces the risk of side effects and antibiotic resistance, while ensuring appropriate treatment for those who need it.
- Probiotics: Probiotics have been studied for symptom relief in diverticular disease because they may help restore gut microbial balance and reduce low-grade inflammation. Some small studies suggest probiotics may decrease abdominal pain or bloating in patients with symptomatic diverticular disease, but evidence is inconsistent and not strong enough for routine recommendation.
- Anti-inflammatory drugs: Anti-inflammatory drugs have been assessed for reducing symptoms and preventing complications in symptomatic, uncomplicated diverticular disease. NSAIDS are generally avoided during diverticulosis.
Surgical Interventions
Surgical intervention for diverticulosis is indicated in cases of complications, such as recurrent or severe diverticulitis that is unresponsive to medical therapy, perforation, abscesses that are not amenable to percutaneous drainage, fistula formation, obstruction, or significant diverticular bleeding that cannot be controlled endoscopically or radiologically. The standard surgical procedures are elective surgery, partial colectomy, and sigmoid colectomy.
Prognosis of Diverticulosis
The prognosis for diverticulosis varies based on factors such as the presence of symptoms, the development of complications, and adherence to preventive measures. Most cases remain uncomplicated, but prognosis may be affected by recurrent diverticulitis, bleeding, or other associated conditions. Early detection and lifestyle modifications can improve long-term outcomes.
- Diverticulosis is usually asymptomatic. Most individuals never experience symptoms or complications from the condition.
- Diverticular bleeding occurs in approximately 15% of cases. This is one of the most common complications, but the majority of patients do not experience significant bleeding.
- If inflammation (diverticulitis) develops, approximately 85% of patients respond well to medical treatment. In the majority of cases, conservative care is effective, and in uncomplicated diseases, mortality is low.
- A minority of patients may require surgery. Usually, surgical intervention is reserved for patients who do not improve with treatments or who experience complications, including fistula, perforation, or abscess.
- Overall, the prognosis is excellent for most patients. With appropriate lifestyle modifications such as increasing physical activity, consuming a high-fibre diet, and avoiding constipation, long-term outcomes are favourable, and the risk of recurrence or complications can be reduced.
- The risk of life-threatening complications is low. Serious outcomes are rare and usually associated with untreated infection or severe bleeding.
Diverticulosis Disease Treatment Cost in Hyderabad, India
The cost of Diverticulosis Disease Treatment in Hyderabad generally ranges from ₹18,000 to ₹55,000 (approximately US $215 – US $660).
The exact diverticulosis treatment cost varies depending on factors such as the severity of the disease, whether diverticulitis (infection or inflammation) is present, the need for imaging tests (CT scan, ultrasound), requirement for IV antibiotics, hospitalization duration, need for colonoscopy, surgeon or gastroenterologist expertise, and the hospital facilities chosen — including cashless treatment options, TPA corporate tie-ups, and assistance with medical insurance approvals wherever applicable.
Cost Breakdown According to Type of Diverticulosis Disease Treatment / Evaluation
- Basic Medical Management (diet modification, oral antibiotics, medications) – ₹18,000 – ₹25,000 (US $215 – US $300)
- Diagnostic Evaluation (colonoscopy, CT scan, blood tests) – ₹20,000 – ₹30,000 (US $240 – US $360)
- Hospital-Based Treatment for Diverticulitis (IV antibiotics, monitoring) – ₹25,000 – ₹40,000 (US $300 – US $480)
- Minimally Invasive Procedures for Complications (abscess drainage) – ₹35,000 – ₹50,000 (US $425 – US $600)
- Surgical Management (for complicated diverticulitis / perforation) – ₹40,000 – ₹55,000 (US $480 – US $660)
Frequently Asked Questions (FAQs) on Diverticulosis Disease Treatment
Is diverticulosis painful?
In most cases, diverticulosis is regarded as an asymptomatic disorder and does not contribute to any pain. However, moderate, nonspecific symptoms, such as bloating or changes in bowel habits, may be experienced by some individuals. Complications like diverticulitis, in which the diverticula become inflamed or infected and cause localised stomach discomfort, are more frequently linked to pain.
Which Is the best hospital for Diverticulosis Treatment in Hyderabad, India?
PACE Hospitals, Hyderabad is regarded as one of the most trusted centres for the diagnosis and treatment of diverticulosis and diverticulitis.
Our team of expert gastroenterologists, general surgeons, dietitians, and infection-control specialists offers accurate diagnosis, modern medical therapy, and minimally invasive treatment options to ensure fast relief and long-term digestive health.
With advanced gastrointestinal diagnostic facilities, 24/7 emergency care, high-precision imaging, and dedicated follow-up programs, PACE Hospitals ensures safe, effective, and complication-free treatment — supported by cashless facility options, TPA corporate tie-ups, and assistance with medical insurance processing for eligible patients.
What is diverticulosis and diverticulitis?
Diverticulosis refers to the presence of asymptomatic diverticula in the colon wall, whereas diverticulitis denotes inflammation or infection of one or more diverticula. Diverticulitis presents with acute symptoms such as localised abdominal pain, fever, and elevated inflammatory markers. Though related, one can have diverticulosis without diverticulitis.
Can diverticulosis cause low haemoglobin?
Diverticulosis may lead to gastrointestinal bleeding from diverticular vessels, which can cause iron-deficiency anaemia and reduced haemoglobin over time. Although most bleeding episodes are self-limited, persistent or recurrent bleeding from diverticula can result in significant blood loss and anaemia.
What is calcified diverticulosis?
The term "calcified diverticulosis" refers to colonic diverticula that contain calcifications, which are often discovered by chance during imaging for gastrointestinal bleeding or other reasons. Chronic diverticular walls or associated fecaliths might develop calcification, which is indicative of long-standing local disease.
What Is the cost of Diverticulosis Disease Treatment at PACE Hospitals, Hyderabad?
At PACE Hospitals, Hyderabad, the cost of diverticulosis treatment typically ranges from ₹17,000 to ₹50,000 and above (approximately US $200 – US $600). However, the final cost depends on:
- Type and severity of diverticulosis / diverticulitis
- Whether hospitalization and IV antibiotics are required
- Need for colonoscopy, CT scan, or additional diagnostic tests
- •Surgical intervention for complications
- Duration of hospital stay and monitoring
- Post-treatment diet and follow-up care
- Surgeon or gastroenterologist expertise
For mild diverticulosis requiring medical therapy, costs fall at the lower end, whereas cases needing hospitalization or minimally invasive procedures fall toward the higher end.
After a complete gastrointestinal evaluation and imaging review, our specialists will provide a personalised treatment plan and a transparent cost estimate based on your condition.
What causes diverticulosis?
Diverticulosis arises from increased intraluminal pressure within weakened spots of the colon wall. Contributing factors include low dietary fibre intake, age-related degeneration of connective tissue, abnormal colonic motility, and genetic predisposition. This combination promotes mucosal herniation through the muscular layer, resulting in the formation of diverticula.
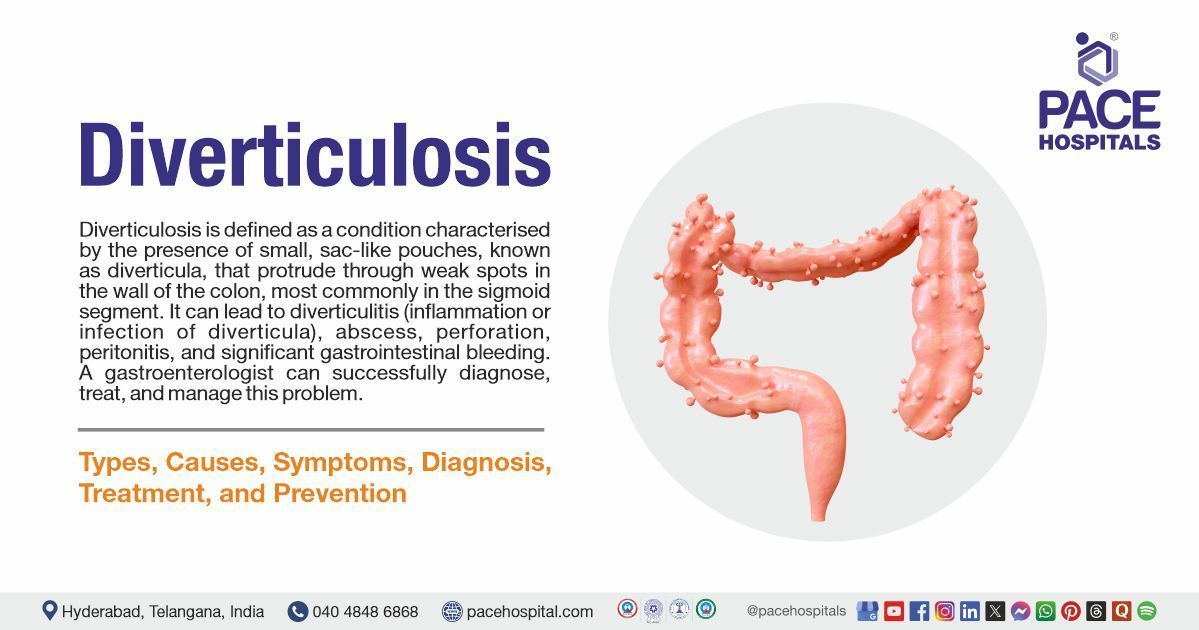
What is the definition of diverticulosis?
Diverticulosis is a condition characterised by the presence of one or more diverticula, which are small sac-like pouches that bulge outward through weak spots in the wall of the colon. These pouches are most commonly found in the lower part of the colon and are generally asymptomatic. The presence of diverticula, alone or without associated symptoms or complications, is referred to as diverticulosis.
What causes colonic diverticulosis?
Colonic diverticulosis develops when weak spots in the muscular wall of the colon allow the inner lining to protrude outward, forming pouches. Factors such as increased intraluminal pressure from low-fibre diets, ageing-related changes in the colon wall, and genetic predisposition contribute to the development of these diverticula. Lifestyle habits and certain medications may further increase the risk.
What is the prevalence of diverticulosis?
Diverticulosis is highly prevalent, especially in older adults. It affects approximately 10% of individuals under 40 years of age, with prevalence rising to more than 70% in those over 80 years. The condition occurs equally in men and women and is more common in Western countries, likely due to dietary and lifestyle differences.
What is pancolonic diverticulosis?
Pancolonic diverticulosis refers to the presence of diverticula distributed throughout the entire colon, rather than being confined to a specific segment such as the sigmoid colon. This pattern is less common than segmental diverticulosis and may be associated with a higher risk of developing complications, including bleeding. Pancolonic involvement is more frequently observed in certain populations and may reflect underlying differences in genetic or environmental risk factors.
How to keep diverticulosis under control?
Lifestyle changes, such as eating a high-fibre diet (20–35 g/day), staying adequately hydrated, and engaging in regular exercise, are key to managing diverticulosis. These steps help reduce colon pressure and restore regular bowel movements. In addition, abstaining from smoking and NSAIDs promotes colonic integrity and lowers the chance of problems.
Can a CT scan detect diverticulosis?
A CT scan is a highly helpful imaging technique for identifying diverticulosis and associated complications. It is capable of visualising diverticula, evaluating for inflammation, and detecting complications like fistulas, perforations, or abscesses. Due to its precision and speed, CT is frequently the imaging method of choice in acute situations.
What are some high-fibre foods recommended for individuals with diverticulosis?
For patients with diverticulosis, a high-fibre diet can help promote regular bowel movements and decrease the risk of complications. Vegetables like broccoli, carrots, and spinach; legumes like beans, lentils, and chickpeas; a range of fruits, particularly those with digestible skins like apples, pears, and berries; and whole grains like bran, whole wheat, barley, oats, quinoa, and brown rice are foods high in fibre.
Can a patient with diverticulosis eat nuts and seeds?
Patients with diverticulosis do not need to avoid nuts, seeds, or popcorn. Earlier dietary advice recommended restricting these foods, but recent studies have shown no increased risk of diverticulitis or bleeding from consuming them. Nuts and seeds can be included as part of a high-fibre diet, which supports colon health and helps prevent complications of diverticulosis.
Which one of these is more life-threatening diverticulosis or IBS?
Diverticulosis is potentially more life-threatening than irritable bowel syndrome (IBS), primarily due to the risk of serious complications such as diverticular bleeding, perforation, or peritonitis. IBS, while often causing significant discomfort and reduced quality of life, is a functional disorder and does not lead to life-threatening complications or structural damage to the colon.