Colon Cancer - Symptoms, Causes, Diagnosis and Treatment
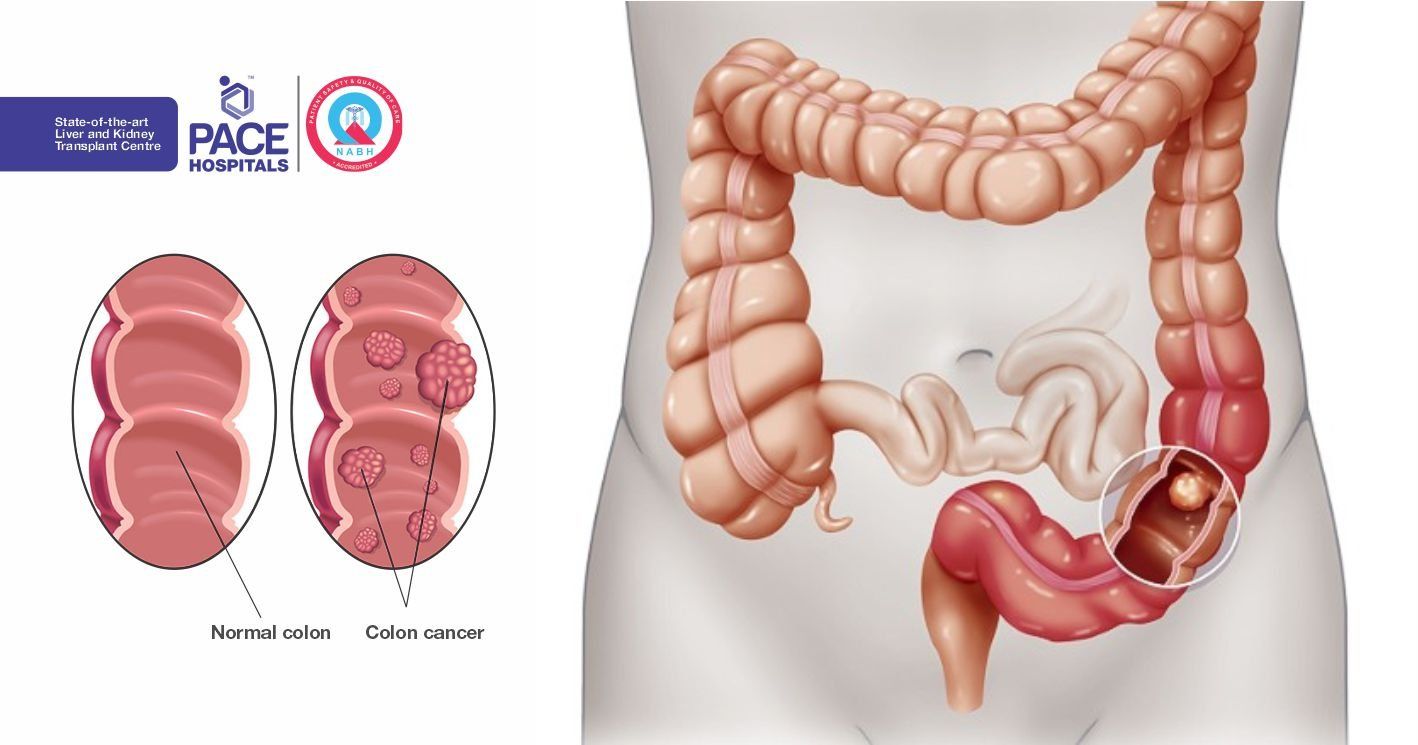
Colon Cancer or Colorectal Cancer (CRC) is a disease of the large bowel, it is a type of cancer that originates from the rectum or colon, also known as colon cancer. Your colon, cecum, rectum and anus make up the large intestine Figure 1. The ileocecal valve, located at the opening between the ileum and the large intestine, controls the flow of chyme from the small intestine to the large intestine.
Colon cancer occurs mainly in the large intestine where waste materials from digestion begin to build up, the colon absorbs vitamins and nutrients from the digested food that passes through. It usually starts when abnormal cells form out of control, invade the wall of the rectum and neighboring tissue. CRC is one of the most common types of cancer among adults. It is also one of the deadliest, with the vast majority of cases occurring in men. Although CRC is usually found in men, it is also possible for women to develop this disease.
Prevalence
Colon Cancer or Colorectal cancer (CRC) is an alarming health problem worldwide. It is the second most common in women (5,71,000 cases, 9.4% of all cancer cases) and the third most common cancer in men (6,63,000 cases, 10.0% of all cancer cases).
Almost 60% of cases are encountered in developed countries. The number of CRC related deaths is estimated to be approximately 6,08,000 worldwide, accounting for 8% of all cancer deaths and making CRC the fourth most common cause of death due to cancer.
In India, the annual incidence rates (AARs) for colon cancer in men are 4.4 and 4.1 per 1,00,000, respectively. The AARs for colon cancer in women is 3.9 per 1,00,000. Colon cancer ranks 8th and rectal cancer ranks 9th among men. For women, this does not figure in the top 10 cancers, whereas CRC ranks 9th.
Signs and Symptoms of Colon Cancer
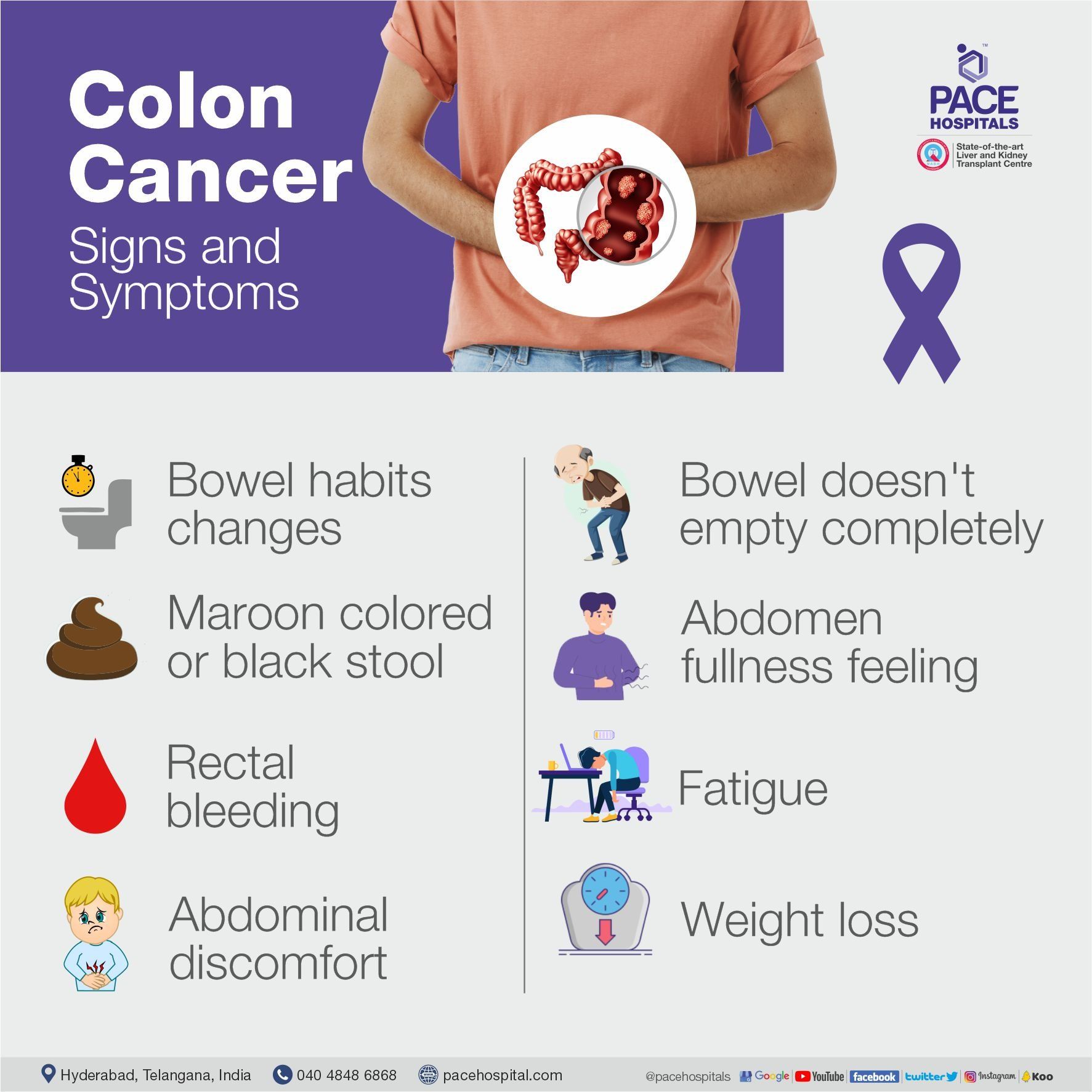
Colon Cancer or Colorectal cancer may not present with any symptoms, especially in the early stages. If you do experience signs and symptoms during the early stages, they may include:
- A persistent bowel habits changes, such as constipation, diarrhea, changes in stool color, changes in stool shape, such as narrowed stool
- Bright red blood in the stool as well as maroon colored or black stool
- Rectal bleeding or blood coming from the rectum
- Persistent abdominal discomfort such as cramps
- Excessive gas and abdominal pain
- A feeling that your bowel doesn't empty completely
- Abdomen fullness feeling, even after not eating for a sometime
- Fatigue or tiredness or weakness
- Unexplained weight loss
Most of these symptoms may also indicate other possible conditions. Many people with colon cancer experience no symptoms in the early stages of the disease. When symptoms appear, they'll likely vary, depending on the cancer's size and location in your large intestine. If you notice any of these symptoms, make an appointment with your gastroenterologist to discuss getting a rectal cancer screening.
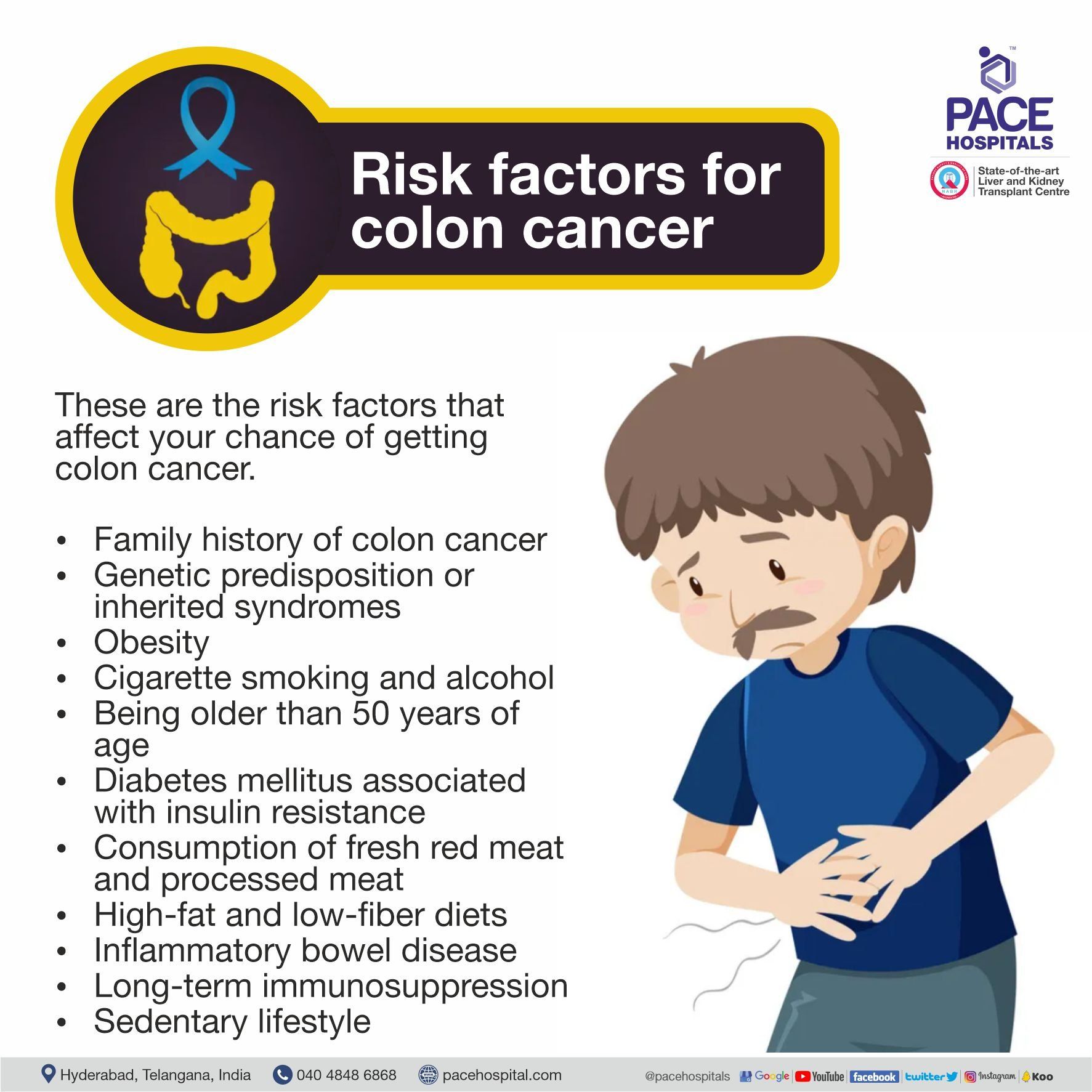
Risk Factors for Colon Cancer
There are several risk factors that directly affect your chance of getting colon cancer.
- Family history: One of the risk factors for colo rectal cancer is a family history, those individuals who have a family history of colorectal cancer are at a higher risk of developing this disease. It is also possible for women to develop this disease after they reach menopause. Research has shown that when comparing children who grew up with no family history of cancer of any kind with those who grew up with a family history of cancer, the risk of developing cancer was much smaller.
- Genetic predisposition or inherited syndromes. If your DNA contains abnormalities that correspond to a higher risk for the illness, you are more likely to develop it as well. For example, people with a genetic predisposition (sometimes also called genetic susceptibility) for polyps in their colon can be at a higher risk for developing the disease. The most common inherited syndromes that increase colon cancer risk are familial adenomatous polyposis (FAP) and Lynch syndrome, which is also known as hereditary nonpolyposis colo rectal cancer (HNPCC).
Environmental Factors
There are certain risk factors for developing colo rectal cancer that are not related to genetics. These include:
- Obesity - People who are obese are slightly (about 30%) more likely to develop colo-rectal cancer than normal-weight people. Researcher found that women ages 20 to 49 who were considered overweight or obese based on BMI had up to twice the risk of developing early onset colo-rectal cancer before age 50, compared with women who reported the lowest BMIs. A higher BMI is associated with increased risks of colon and rectal cancers in both men and in women, but the increases are higher in men than in women.
- Diabetes mellitus associated with insulin resistance - Diabetes mellitus is a disorder in which the body does not produce enough or respond normally to insulin, causing blood sugar (glucose) levels to be abnormally high. Urination and thirst are increased, and people may lose weight even if they are not trying to. Obesity (being significantly overweight and belly fat), an inactive lifestyle, and a diet high in carbohydrates are the primary causes of insulin resistance.
- High-fat and low-fiber diets - Research showed that levels of F nucleatum increase if an individual switches from a low-fat, high fiber diet to a high-fat, low-fiber diet can increase risk of colon cancer. Fusobacterium nucleatum (F. nucleatum) – positive indicates colo-rectal cancer.
- Cigarette smoking - People who have been smokers for many years are at a greater risk of developing colon polyps because nicotine decreases the production of natural lubricants in the colon. Long periods of cigarette smoking decreases the amount of lubrication in the colon and can increase the risk of developing inflammation, which can cause polyps.
- Sedentary lifestyle - lifestyle involving little or no physical activity. A person living a sedentary lifestyle is often sitting or lying down while engaged in an activity like reading, socializing, watching television, playing video games, reading or using a mobile phone / computer for much of the day.
- Age and gender - Older men are at a high risk (25% higher in men than in women)
- Inflammatory bowel disease (IBD) is a chronic inflammation of digestive or GI (gastrointestinal) tract. The digestive tract includes mouth, esophagus, stomach, small intestine and large intestine. Chronic inflammatory diseases of the colon, such as Crohn's disease, Ulcerative colitis (UC) and Indeterminate Colitis (IC) can increase your risk of colon cancer.
- Alcohol consumption - Moderate to heavy alcohol consumption is associated with 1.2- to 1.5-fold increased risks of cancers of the colon and rectum compared with no alcohol consumption.
- Consumption of fresh red meat and processed meat - There is strong evidence that consumption of either red meat, such as beef, pork and lamb or processed meat are both causes of colo-rectal cancer. People who eat a lot of fruits and vegetables are less likely to develop cancer.
- Cholecystectomy History - Cholecystectomy is the surgical removal of the gallbladder. It is a common treatment of symptomatic gallstones and other gallbladder conditions. Researcher found that a history of cholecystectomy was positively associated with the risk of colo-rectal cancer.
- Uretero-Colic Anastomosis
- Cancer Radiation therapy. Radiation therapy through the abdomen to treat previous cancers increases the risk of colon cancer.
- Long-term immunosuppression (Suppression of the immune system and its ability to fight infection) following organ transplantation, especially renal transplantation - The relative risk is the same as that of the normal population, but aged 20–30 years older.
Causes
Researchers aren't certain what causes most colon cancers. It is not clear exactly why CRC develops in some people and not in others. In general, CRC begins when healthy cells in the colon develop changes (mutations) in their DNA. A cell's DNA contains a set of instructions that tell a cell what to do.
Cancer may be caused by genetic mutations, either inherited or acquired. These mutations don’t guarantee you’ll develop colon cancer, but they do increase your chances. With time, the cancer cells can grow to invade and destroy normal tissue nearby. And cancerous cells can travel to other parts of the body to form deposits there (metastasis).
Prevention
Many lifestyle measures may reduce the risk of developing colorectal cancer -
- Regular screening: People who have had colon cancer before, who are over 50 years of age, who have a family history of this type of cancer, or who have Lynch syndrome, Crohn’s disease or adenomatous polyposis should have regular screenings.
- Maintaining a healthy bodyweight: Being overweight or obese raises the risk of many cancers, including colorectal cancer. You can limit portion size to control calorie intake, add healthy snacks during the day if you want to gain weight, be as physically active as you can be.
- Regular exercise: Moderate, regular exercise has been shown to have a significant impact on lowering a person’s risk of developing colorectal cancer.
- Healthy diet: Follow a diet with plenty of fiber, fruit, vegetables, and good quality carbohydrates and a minimum of red and processed meats
Screening
Screening tests for colo-rectal cancer can be done in many ways. A physical exam may be used in order to detect abnormalities in the large intestine. You may also be asked to undergo several tests such as a fecal test, blood test, Fecal Occult Blood Test (FOBT), CEA Test (Carcinoembryonic Antigen), X-ray, CT scan, colonoscopy, sigmoidoscopy or enteroscopy.
If the tests for colo-rectal cancer indicate that you have this disease, you will then get a consultation with a gastroenterologist. During your first visit, the gastroenterologist will ask you questions about your medical history, lifestyle, and any concerns you may have regarding your gastrointestinal tract.
After the initial check-up, your gastroenterologist will likely recommend that you undergo one or more clinical trials, which are usually outpatient procedures. These clinical trials allow the physician to get a better view of how your body responds to treatment, without having to do any invasive testing. The type of clinical trial that your doctor might recommend depends on your individual case, but all clinical trials will include some combination of blood tests, scans, and gastrointestinal tract tests.
Diagnosis
Early detection and treatment dramatically improve the odds of beating this disease. A tumor is not the reason for this condition. Instead, it is caused by a tumor that has formed within the colon wall. Screening can detect polyps before they become cancerous, as well as detecting colon cancer during its early stages when the chances of a cure are much higher. These are the commonly used screening and diagnostic procedures for colorectal cancer-
- Fecal Occult Blood Test (FOBT)
- If you have a positive result, which means that it showed blood in the stool. A blood in stool test is not 100-percent accurate, because not all cancers cause a loss of blood, or they may not bleed all the time. Blood may also be present because of other illnesses or conditions like piles, hemorrhoids.
- Fecal calprotectin (Faecal calprotectin) - It is a biochemical measurement of the protein calprotectin in the stool. Elevated faecal calprotectin indicates the migration of neutrophils to the intestinal mucosa. It is a simple and sensitive non-invasive marker of CRC and adenomatous polyps. It is more sensitive than fecal occult blood tests (FOBT) for detection of colorectal neoplasia at the cost of a somewhat lower specificity.
- Narrow-band imaging (NBI) - Recent progress in endoscopic techniques, including the development of chromoendoscopy and magnifying endoscopy with narrow-band imaging (NBI), have tried to overcome the limitations of conventional colonoscopy and thus produce an increase in diagnosis, detection and resection of colorectal lesions.
- Endoscopic Ultrasound (EUS) - It is essential to have accurate staging of CRC for selecting patients who can undergo surgery. Usually clinical staging is accomplished by performing a physical examination through an imaging evaluation (eg, transrectal endoscopic ultrasound, computed tomography scanning (CT scan), or magnetic resonance imaging (MRI scan)).
- Barium enema X-ray - It is also called a colon X-ray and can detect changes or abnormalities in the large intestine (colon).
- Stool DNA test – It is also called a stool DNA-fecal immunochemical test, is a combination test that detects specific changes (mutations) in several genes associated with colon cancer within the cells shed in stool, as well as trace amounts of blood in stool.
- Sigmoidoscopy - It is also called a flexible sigmoidoscopy, is a procedure that lets your doctor look inside your sigmoid colon by using a flexible tube with a light on it. It helps your doctor check for abnormal cells, polyps, ulcers.
- Colonoscopy - A colonoscopy is a process in which a thin tube with a camera is inserted into your anus. This camera will show images of your large intestine, the walls, and some of the lining of your intestines. Some of the symptoms that may be seen during this procedure include an abnormal color or appearance of your feces, bowel movements, blood in the stool, and an odd odor.
- Enteroscopy - It is a procedure that helps your doctor find and treat problems in the digestive system. It is commonly used to detect problems in the small intestine or stomach such as abnormal gastrointestinal bleeding, a high white blood cell count, intestinal damage from radiation treatment, tumors in the small intestine, unexplained severe diarrhea, blocked bowel passages, abnormal X-ray results and unexplained malnutrition.
- Virtual colonoscopy - It is also known as a CT colonography. Virtual colonoscopy is most often used to designate the search for precancerous colonic lesions, by CT, in asymptomatic patients. The main reason for doing CT colonography is to screen polyps or cancers in the large intestine. Polyps are growth that emerged from the inner Layer. A small number of polyps can grow and turn into cancer.
The symptoms can be difficult to recognize and often go undetected for years. If detected, colorectal cancer is a potentially deadly disease that has a 5 years survival rate of approximately 60 to 65%. Unfortunately, the 5 year survival rate for people diagnosed with advanced cancer is only about 10 to 14% percent.
Treatment
Treatment will depend on many factors, including the location, size and stage of the cancer, whether or not it is recurrent and the current state overall state of health of the patient. Treatment options include:
- Surgery - is another common form of colorectal cancer treatment. Surgical techniques is used when a tumor in the colon or pelvic area is malignant or cancerous and cannot be treated using chemotherapy. When a tumor in this area is malignant, surgery is usually the only option. However, in some instances a tumor may not be cancerous and surgery may be an option if it is not possible to remove the tumor using chemotherapy.
For early-stage colon cancer, gastroenterologist may recommend a minimally invasive such as
- Minimally invasive surgery (laparoscopic surgery)
- Laparoscopic surgery for colon cancer has been proven feasible and safe when compared with open surgery. This type of surgery may benefit patients by reducing postoperative pain, allowing fast recovery of bowel function and normal dietary intake and shorter hospitalization. Therefore, minimally invasive surgeries such as laparoscopic or robot surgery have become the predominant treatment option for colon cancer.
- Removing polyps during a colonoscopy (polypectomy) - As per the research colonoscopic removal of adenomatous polyps observed 53% reduction in mortality. The goal of this procedures is to remove the polyps in one piece to avoid colectomy.
For advanced-stage colon cancer, gastroenterologist may recommend:
- Partial colectomy - It is a procedure to remove the diseased portion of your colon and a small portion of surrounding healthy tissue,
Figure 2
- Colostomy - it is a surgical procedure that brings one end of the large intestine out through the abdominal wall. During this procedure, one end of the colon is diverted through an incision in the abdominal wall to create a stoma. A stoma is the opening in the skin where a pouch for collecting feces is attached.
- Lymph node removal. Nearby lymph nodes are usually also removed during CRC surgery and tested for cancer.
In addition to surgery, chemotherapy can also be administered in a variety of different ways. In a typical procedure, doctors will administer medication through a vein in the arm or into a catheter inserted under the skin. The medication is then spread throughout the entire body via these instruments. In some procedures, surgery is combined with chemotherapy to maximize the chances of stopping or reducing the size of the cancer cells. In some cases, radiation is used alongside surgery to kill as many cancer cells as possible while the patient is undergoing the procedure.
- Colonic Metal Stenting or colonic stenting - It is the preferred treatment for palliation of malignant colonic obstruction or considered as a bridge to surgery to be discussed, within a shared decision-making process, as a treatment option in patients with potentially curable left-sided obstructing colon cancer as an alternative to emergency resection or should be performed or directly supervised by an operator who can demonstrate competence in both colonoscopy and fluoroscopic techniques and who performs colonic stenting on a regular basis. Figure 3
- Chemotherapy - One of the most common types of colorectal cancer treatment is chemotherapy. Chemotherapy involves the use of medication or combination of medications to fight cancer cells in the colon and its various components. Although chemotherapy is successful in killing cancer cells, it is not without side effects and sometimes worsens existing conditions. Chemotherapy treatments can take several forms and can be administered in a variety of ways. It is important, when considering colorectal cancer treatment, discuss all options with your doctor.
- Radiofrequency ablation (RFA) - It is one of the most common methods to treat cancer that has spread to the liver. It uses high-energy radio waves to kill cancer cells. A CT scan or ultrasound is used to guide a thin, needle-like probe through the skin and into the tumor.
- Immunotherapy is a type of biological therapy for cancer treatment that helps your immune system fight cancer. The immune system helps your body fight infections and other diseases. It is made up of white blood cells and organs and tissues of the lymph system.
- Radiation therapy - Another option for treating colorectal cancer is to use radiation therapy. This form of colorectal cancer treatment uses x-rays to damage cancerous cells in the stomach, duodenum, or pelvis. Although this can be successful in removing large tumors, it is often accompanied by nausea and vomiting, bone loss and other negative side effects. Chemotherapy is usually recommended as the first line of defense against colorectal cancer.
Unfortunately, this treatment can have some serious side effects. Some patients experience incontinence, fluid retention, and gastrointestinal problems after chemotherapy. It can also lead to fatigue, nausea, vomiting, weight loss, and hair loss. The effectiveness of this form of treatment depends on how well the cancer cells are treated. Sometimes, it may not even be able to remove all of the cancer cells. For this reason, it is often used along with surgery.
Frequently asked questions (FAQs)
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868