Diverticulosis - Symptoms, Causes, Diagnosis, Treatment & Prevention
PACE Hospitals
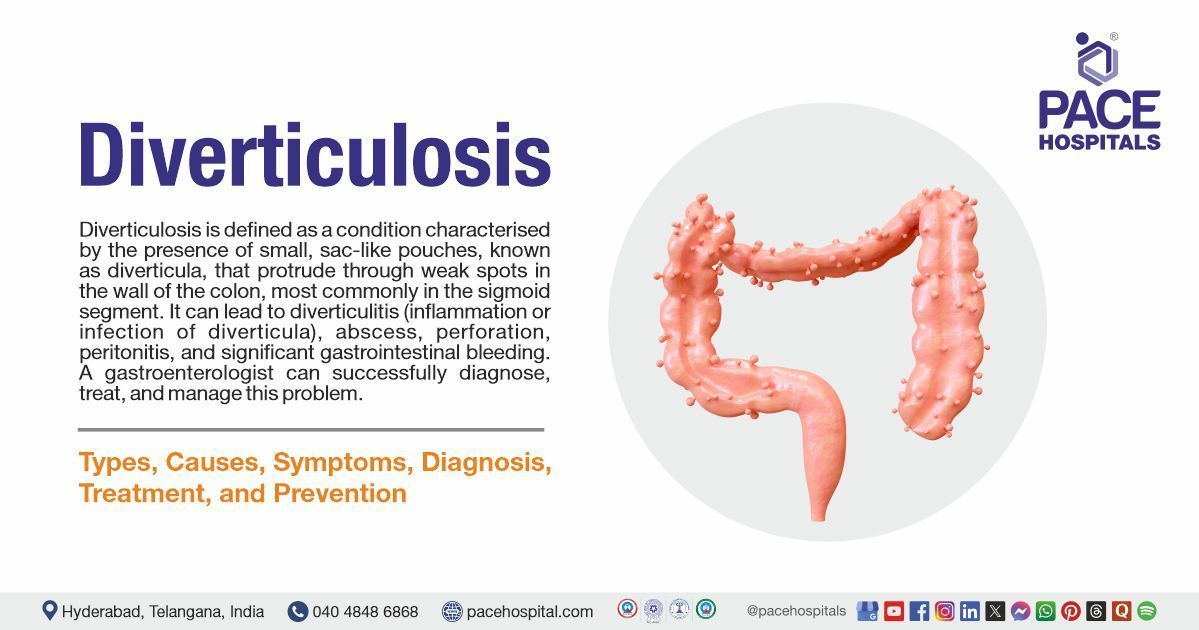
Diverticulosis definition
Diverticulosis is defined as a condition characterised by the presence of small, sac-like pouches, known as diverticula, that protrude through weak spots in the wall of the colon, most commonly in the sigmoid segment. The main cause of diverticulosis is unclear, but risk factors include a low-fibre diet, sedentary lifestyle,
obesity, smoking, and use of certain medications such as NSAIDs. Most people with diverticulosis are asymptomatic, but some may experience abdominal pain, bloating, changes in bowel habits, or rectal bleeding. Complications can include diverticulitis (inflammation or infection of diverticula), abscess, perforation, peritonitis, and significant gastrointestinal bleeding.
A gastroenterologist (a specialist in digestive system disorders) can successfully diagnose, treat, and manage the problem, ensuring proper healing and avoiding complications.
Diverticulosis meaning
The term "diverticulosis" is derived from mixed Latin and Greek words
- Diverticulum: From Latin, meaning "a bypath" or "a small turning aside," based on divertere ("to turn aside").
- -osis: A Greek suffix used in medical terminology to denote a condition, usually abnormal.
Thus, "diverticulosis" literally refers to the condition of having diverticula.
Prevalence of Diverticulosis
Prevalence of diverticulosis Worldwide
Diverticulosis is a common condition, especially in developed countries, and its prevalence increases with age. In Western countries, it affects 5–45% of the population. About 20% of people under 40 have the condition, while 60% of those over 60 are affected. In the U.S., nearly one-third of people aged 50–59 have diverticulosis. Age is the strongest risk factor. The condition is often found incidentally during imaging or colonoscopy.
In Asian countries, diverticulosis has historically been less common, but recent studies show a rising trend. Prevalence now ranges from 13–25% in some populations. Unlike Western countries, where left-sided disease is common, right-sided diverticulosis is more common in Asia, particularly in Japan, Hong Kong, and Singapore.
Prevalence of diverticulosis in India
In India, the true incidence of colonic diverticulosis is unclear due to limited community studies. Hospital-based data shows prevalence rates of 3.2% in northern India and up to 9.9% in southern India, increasing with age, from 0.3% under 30 years to about 32% over 60 years. Less than 25% of cases become symptomatic, and only 10–25% develop diverticulitis. The incidence is rising gradually, likely due to aging populations and lifestyle changes.
Types of Diverticulosis
Diverticulosis can be categorised according to its location, clinical manifestation, and anatomical structural characteristics. The different types of diverticulosis include:
By anatomical location
- Colonic diverticulosis
- Right-sided diverticulosis
- Left-sided diverticulosis
- Pancolonic diverticulosis
- Small bowel diverticulosis
By structural features
- Acquired (False) diverticulosis
- Congenital (true) diverticulosis
- Giant colonic diverticulosis
By clinical presentation
- Symptomatic uncomplicated diverticulosis disease
- Segmental colitis associated with diverticulosis
By anatomical location
- Colonic diverticulosis: Colonic diverticulosis, the most prevalent type, mostly affects the left sigmoid colon. It usually comes on by elevated intraluminal pressure, which is frequently brought on by a low-fibre diet and persistent constipation. Diverticula, which are tiny mucosal pouches, form in weak spots in the colon wall as a result of this pressure over time. The prevalence is higher in Western populations and rises with age.
- Right-sided diverticulosis: Right-sided diverticulosis mainly involves the ascending colon and is more common in Asian populations and younger individuals. It may have a different pathophysiology than left-sided disease, and can sometimes mimic appendicitis. Diverticula may be solitary or multiple.
- Left-sided diverticulosis: Predominant in Western countries, left-sided diverticulosis involves the descending and sigmoid colon. This type is more likely to be associated with complications, such as diverticulitis, than right-sided disease.
- Pancolonic Diverticulosis: Pancolonic diverticulosis refers to diverticula distributed throughout the colon, including the sigmoid, descending, transverse, and ascending segments. This pattern is often seen in more severe or chronic cases and is associated with extensive anatomical changes in the colon.
- Small bowel diverticulosis: Rarely, diverticula can form in the small intestine (e.g., jejunal diverticulosis, Meckel’s diverticulum). These are not generally included in standard colonic diverticulosis classifications.
By structural features
- Acquired (False) Diverticulosis: This is the most common form of diverticulosis, which involves only the mucosa and pushing through a weak area in the muscular layer with the submucosa.
- Congenital (true) diverticulosis: Congenital diverticulosis is rare and characterized by true diverticula containing all layers of the bowel wall (mucosa, submucosa, muscularis, and serosa). It usually affects the right colon and is present from birth due to developmental wall defects.
- Giant colonic diverticulosis: Giant colonic diverticulosis is an uncommon and severe form of diverticulosis characterised by diverticula greater than 4 cm in diameter, which often occur in the sigmoid colon. These big pouches usually require surgical care due to their increased risk of consequences, including rupture, abscess, or blockage.
By clinical presentation
Clinical subtypes of diverticulosis are:
Symptomatic uncomplicated diverticulosis disease: SUDD is characterized by chronic, often recurrent left lower quadrant abdominal pain in the absence of overt inflammation or infection. It represents a functional manifestation of diverticulosis and is thought to involve low-grade inflammation or altered motility.
Segmental colitis associated with diverticulosis: SCAD is a localized, non-specific colitis affecting colonic segments with diverticulosis, most commonly in the sigmoid colon. It presents with mild symptoms such as rectal bleeding or diarrhea and can mimic inflammatory bowel disease (IBD), although it usually follows a benign course.
Diverticulosis Causes
Understanding the root causes that contribute to the development of diverticulosis is important for effective prevention and appropriate management of the condition. A variety of intrinsic and extrinsic factors have influenced its onset.
Diverticulosis causes may include:
- Increased pressure within the colon (intraluminal pressure)
- Structural weakness in the colonic wall
- Low-fibre diet
- Genetic factors
Increased pressure within the colon (intraluminal pressure): The main contributing factor of diverticulosis is elevated pressure within the colon. Abnormal colonic motility, particularly exaggerated segmental contractions (segmentation), leads to the formation of isolated high-pressure compartments within the colon. These localised high pressures can force the mucosa and submucosa to herniate through weak points in the muscular layer, forming diverticula.
Structural weakness in the colonic wall: Diverticula most commonly form at sites where blood vessels (vasa recta) penetrate the circular muscle layer of the colon, creating natural weak spots. Age-related changes, such as degeneration of collagen and elastin, further reduce the compliance and strength of the colonic wall, making it more susceptible to herniation under pressure.
Low-fibre diet: A diet deficient in fibre results in smaller, harder stools that require increased colonic pressure to move through the bowel. This chronic elevation in pressure contributes to the formation of diverticula.
Genetic factors: Family history and certain genetic predispositions can increase the risk of developing diverticulosis. Some people may have inherited connective tissue weaknesses or other factors that make their colon walls more prone to forming diverticula.
Diverticulosis Symptoms
Diverticulosis often develops without symptoms and may go unnoticed for years.
While many individuals remain unaware that they have the condition, some may begin to experience signs that lead to further evaluation.
The symptoms of diverticulosis are generally classified into three categories: asymptomatic, symptomatic, and complicated diverticulosis.
- Asymptomatic diverticulosis
- Symptomatic (uncomplicated) diverticular disease
- Complicated diverticulosis
Asymptomatic diverticulosis
Diverticulosis is commonly found by chance during imaging or colonoscopy done for other purposes, and most patients with the disorder have no symptoms.
Symptomatic (Uncomplicated) Diverticulosis
Some people may develop mild, non-specific symptoms, including:
- Intermittent abdominal pain
- Bloating or abdominal distension
- Flatulence
- Changes in bowel habits
Intermittent abdominal pain: Abdominal pain, usually in the lower left side, is the most common symptom when diverticulosis is symptomatic. This pain results from increased pressure or mild inflammation around the diverticula. The discomfort is often intermittent and may worsen after eating or during periods of constipation.
Bloating or abdominal distension: Bloating is common due to altered bowel motility and gas production. The presence of diverticula can affect the normal movement of the colon, leading to a sensation of fullness or swelling.
Flatulence: The diverticula may interfere with the normal function of the bowel and result in increased gas production and frequent passage of wind.
Changes in bowel habits: Symptoms include an alternating pattern of bowel (i.e., constipation or diarrhoea). Some people could experience more frequent bowel movements. Diverticulosis-related altered intestinal motility is the cause of these alterations.
Complicated diverticulosis
Complications can include:
- Diverticulitis: Persistent lower abdominal pain (usually left-sided), fever, chills, nausea, and abdominal tenderness, indicating inflammation or infection of diverticula.
- Diverticular bleeding: Sudden, painless, bright red rectal bleeding, resulting from rupture of blood vessels near the diverticula. This can sometimes be significant and may require medical attention.
- Other complications: Other complications include abscess formation (localized pain, fever), fistulas (which can cause recurrent urinary tract infections if involving the bladder), bowel obstruction, strictures, and perforation (causing intense abdominal pain and signs of peritonitis, a medical emergency).
These classifications could be helpful in prompt diagnosis and treatment by assisting gastroenterologists in identifying the range of diverticulosis, from asymptomatic to symptomatic and complex types.
Diverticulosis Risk Factors
Several factors can increase the likelihood of developing diverticulosis. Understanding these risk factors is important for identifying individuals who may be more prone to this condition and for guiding preventive measures. The factors are as follows:
Non- controllable risk factors
- Age
- Gender
- Genetic predisposition
Controllable risk factors
- Low-fibre diet
- Lack of physical activity
- A diet high in red meat
- Body weight
- Smoking
- Alcohol consumption
- Use of NSAIDs and certain medications
- Comorbidities
Non-Controllable Risk Factors
Age: Advancing age is a primary risk factor. The incidence of diverticulosis rises significantly after age 60, likely due to degenerative changes in the colonic wall, including neural degeneration and weakening of connective tissue over time.
Gender: Males are at increased risk of diverticulosis in early adulthood, while female becomes a more significant factor in the elderly population. Reasons such as the protective effect of estrogen in premenopausal women, as well as differences in diet, body fat distribution, and lifestyle.
Genetic predisposition: Studies have indicated that diverticula tend to occur more frequently in specific families, suggesting that genetic predisposition plays a role in the development of diverticulosis. This implies that some people are more prone to developing diverticula due to inherited characteristics that may affect the strength and structure of the colon wall. The condition's biological mechanisms, including colonic motility and connective tissue integrity, can be influenced by genetic factors
Controllable Risk Factors
Low-fibre diet: Low-fibre diets result in smaller, harder stools that need more colonic pressure to pass. Diverticula are formed when the mucosa and submucosa herniate through weak areas in the colon wall as a result of this pressure over time.
Lack of physical activity: Lack of regular physical activity is associated with slower bowel movements and increased risk of constipation. This can raise intraluminal pressure, contributing to the development of diverticula over time.
A diet high in red meat: A high red meat diet raises the risk of diverticulosis and its complications, with studies indicating up to a 58% higher risk for those consuming red meat compared to the least.
Body weight: Diverticulosis is more common in obese people, perhaps as a result of elevated intra-abdominal pressure and related metabolic alterations. According to studies, people who are overweight are more likely to develop diverticulosis and its complications.
Smoking: Smoking weakens the colon wall through increased inflammation and poor blood flow, which raises the risk of diverticulosis. Additionally, it interferes with regular colon contractions, which raises pressure and causes diverticula to form. Smoking can also change the gut microbiota, which exacerbates inflammation and weakens the colon. When considered collectively, these factors increase the risk of diverticulosis in smokers.
Alcohol consumption: Alcohol consumption is an independent risk factor. It can inhibit colonic motility and increase intracolonic pressure, possibly through inflammatory pathways, thus contributing to diverticulosis development.
Use of NSAIDs and other medications: Regular use of NSAIDs, steroids, opioids, and aspirin can irritate and damage the colon lining, weaken the colon wall, and promote inflammation, all of which increase the risk of diverticulosis and its complications.
Comorbidities: Diverticulosis is associated with metabolic disorders such as hypertension, hyperuricemia, and elevated triglycerides. These elements may weaken the colon wall and increase its susceptibility to diverticula by causing vascular alterations, endothelial damage, and decreased blood flow.
Complications of Diverticulosis
While diverticulosis remains asymptomatic, it may lead to several complications, especially when the diverticula get inflamed or infected. It is important for to detect diverticulosis early, to prevent any type of complications.
The most common complications of diverticulosis are:
- Diverticulitis
- Perforation and peritonitis
- Abscess formation
- Fistula formation
- Bowel obstruction
- Diverticular bleeding
Diverticulitis: This is the most common complication, affecting approximately 4-15% of patients with diverticulosis. It can develop when a diverticulum becomes inflamed or infected, often due to blockage by stool (faecolith), which causes mucosal damage, bacterial overgrowth, and localized inflammation. If the inflammation spreads or becomes severe, it can lead to serious complications, such as perforation or abscess formation.
Perforation and peritonitis: Severe inflammation or infection can cause the wall of a diverticulum to rupture (perforate), resulting in leakage of intestinal contents into the abdominal cavity. This can lead to peritonitis, a potentially life-threatening infection of the abdominal lining.
Abscess formation: An abscess arises when a diverticulum becomes inflamed (diverticulitis), and the body’s immune response is unable to contain the infection. Instead of spreading throughout the abdomen, the infection can become localised, resulting in a collection of pus known as an abscess. This abscess can cause persistent abdominal pain, fever, and sometimes a palpable mass. If diverticulosis is left untreated, an abscess can enlarge, rupture, or lead to further complications, such as a fistula or sepsis. Treatment often involves antibiotics and, in some cases, drainage of the abscess.
Fistula formation: Chronic inflammation and infection can lead to the erosion of a diverticulum's wall into surrounding structures, such as the skin or the vagina (colo-vaginal fistula). Still, most frequently, the erosion occurs in the bladder (Colovesical fistula). Recurrent UTIs, unusual vaginal discharge, or the passage of air or stool in the urine are some symptoms that may result from this. To cure the underlying diverticular disease and repair the abnormal connection, fistulas often require surgical intervention.
Bowel obstruction: Recurrent episodes of diverticulitis can induce chronic inflammation and scarring, which can narrow the colon (strictures) and result in partial or total intestinal obstruction. This can require surgical intervention and cause constipation, bloating, and stomach pain.
Diverticular bleeding: Rectal bleeding that is mild but occasionally severe might result from diverticula eroding into nearby blood vessels. This is a known complication that may be severe enough to necessitate intervention or hospitalisation.
Diverticulosis Diagnosis
Diagnosing diverticulosis involves detecting small pouches (diverticula) in the walls of the colon, often found incidentally during tests for other digestive issues. Initial evaluation is usually done by a primary care physician. If needed, the patient may be referred to a gastroenterologist for further assessment. The goal of diagnosis is to confirm the presence of diverticula and determine whether the condition is symptom-free or associated with discomfort or complications.
The diagnostic process usually includes the following steps:
- Medical history
- Physical examination
- Laboratory tests
- Blood test
- Stool test
- Imaging tests
- Computed tomography (CT)
- Ultrasound
- Magnetic resonance imaging (MRI)
- Abdominal X-ray
- Endoscopic evaluation
- Colonoscopy
Diverticulosis Disease Treatment
Diverticulosis is managed with a patient-centred, stepwise approach, beginning with lifestyle and dietary changes initiated by a general physician. Treatment depends on symptoms, digestive health, and risk of complications. Most cases are managed by the general physician without medication, but persistent or severe symptoms prompt referral to a gastroenterologist for advanced medical or surgical management.
- Non-pharmacological therapy
- Pharmacological therapy
- Surgical interventions
Non-pharmacological therapy
- Dietary and lifestyle modification
- Patient education
- Regular physical exercise
Pharmacological therapy
- Fibre supplements
- Pain management
- Antispasmodics
- Antibiotics: Antibiotics are not indicated for uncomplicated diverticulosis.
- Probiotics and anti-inflammatory drugs
Surgical interventions
Surgical interventions for diverticulosis are reserved for specific situations, primarily when complications arise or conservative treatments fail.
- Elective surgery
- Partial colectomy
- Sigmoid colectomy
Treatment is thus individualized, with the primary goals of relieving symptoms, preventing complications, and improving quality of life.
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
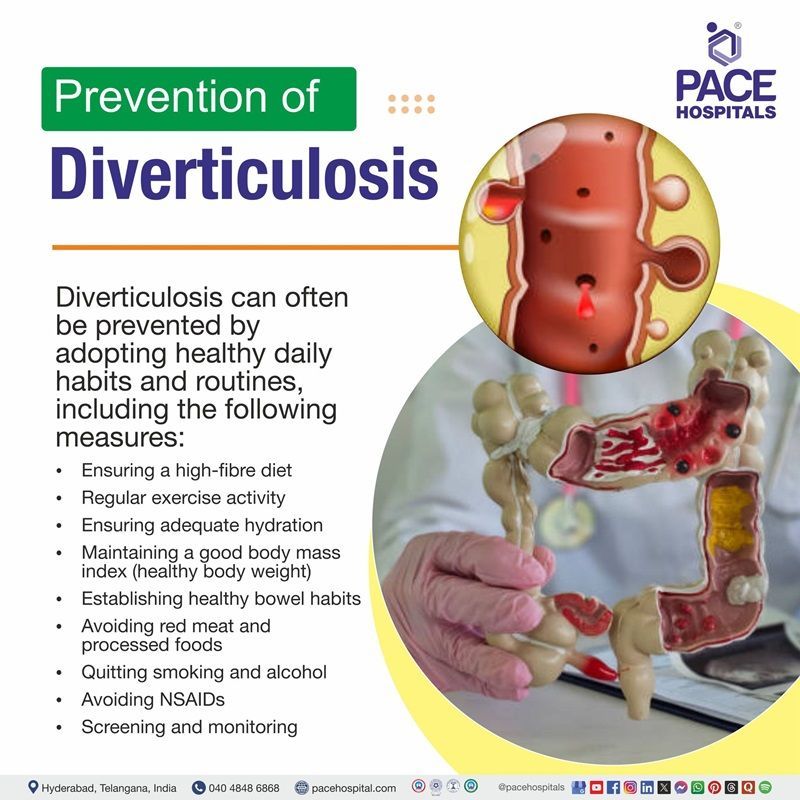
Diverticulosis Prevention
Preventing diverticulosis is more effective than managing its complications later. Since the condition develops gradually over time, early and consistent care of digestive health is key. Maintaining colon strength and motility, lowering intestinal pressure, and promoting general gut health are the key goals of prevention. Diverticulosis risk can be considerably reduced by forming long-term, healthy behaviours.
Diverticulosis can be prevented by managing healthy daily habits and routines, including the following measures:
- Ensuring a high-fibre diet
- Regular exercise activity
- Ensuring adequate hydration
- Maintaining a good body mass index (BMI) (healthy body weight)
- Establishing healthy bowel habits
- Avoiding red meat and processed foods
- Quitting smoking and alcohol
- Avoiding NSAIDs
- Screening and monitoring
Ensuring a high-fibre intake: A diet rich in fibre, especially from fruits and vegetables, has been shown to decrease the risk of diverticulosis and its complications, including diverticulitis. Higher fibre intake promotes regular bowel movements, reduces intracolonic pressure, and supports overall colon health.
Regular physical activity: Engaging in regular physical activity, especially moderate to vigorous exercises like brisk walking, jogging, or swimming, stimulates normal bowel function and reduces intestinal transit time. Physical activity decreases the risk of chronic constipation and reduces inflammation, both of which are implicated in diverticulitis. Studies have shown that physically active people have a significantly lower risk of developing symptomatic diverticular disease.
Ensuring adequate hydration: Drinking enough water helps fibre work effectively, softening stool and promoting regular bowel movements, which may reduce the risk of developing diverticula.
Maintaining a good body mass index (BMI): Obesity is a risk factor for diverticulosis and its complications. Diet management through diet and exercise supports overall colon health.
Establishing healthy bowel habits: Maintain regular, relaxed bathroom habits by responding promptly to the urge to go, especially after meals. Avoid straining or sitting too long on the toilet, as this increases colonic pressure and the risk of developing diverticula.
Limiting red meat and processed foods: Reducing red meat intake and adopting a more plant-based, high-fibre diet can decrease inflammation and improve gut microbiota, both of which are protective against diverticular complications.
Quitting smoking and alcohol: Limiting alcohol intake and avoiding smoking are also suggested, as alcohol may be associated with diverticular bleeding, and smoking with increased risk of complications.
Avoiding NSAIDs: NSAIDs can increase the risk of diverticular bleeding and inflammation by weakening the gut lining and impairing mucosal defence mechanisms. Long-term or frequent use of these drugs is discouraged in individuals with diverticulosis.
Screening and monitoring: Routine screening for diverticulosis is not recommended for prevention in asymptomatic individuals, as the condition is usually found incidentally during colonoscopy or imaging for other reasons.
Difference Between Diverticulosis and Diverticulitis
Diverticulosis vs diverticulitis
Diverticular disease has two stages: diverticulitis and diverticulosis. A proper diagnosis, effective therapy, and appropriate patient education all depends on an understanding of their differences. Although diverticula, or small pouches, are found in the intestinal wall in both disorders, their clinical findings, effective treatment, and related risks may vary. Being aware of the distinctions between the two conditions, confusion can be prevented and treatment can be individualised to the patient's condition/ severity. The table below highlights key differences between diverticulosis and diverticulitis:
| Parameters | Diverticulosis | Diverticulitis |
|---|---|---|
| Definition | Presence of small pouches (diverticula) in the colon wall | Inflammation or infection of one or more diverticula |
| Symptoms | Usually asymptomatic; may cause mild abdominal discomfort, bloating, constipation, diarrhea, or bleeding | Acute abdominal pain (often lower left), fever, nausea, vomiting, and sometimes changes in bowel habits |
| Prevalence | Very common, especially with increasing age | Less common; occurs in 10–15% of those with diverticulosis |
| Causes | Increased intraluminal pressure, often related to low-fibre diet, aging, and colonic wall weakness | Obstruction of a diverticulum (often by stool), leading to inflammation and/or infection |
| Pathophysiology | Structural herniation through weak colon walls, often related to ageing and colonic pressure. | Fecalith impaction, trauma to diverticulum, bacterial overgrowth → inflammation/infection; possible abscess/perforation. |
| Complications | May cause painless rectal bleeding (diverticular bleeding); rarely leads to other complications | May cause abscess, perforation, peritonitis, fistula, or obstruction |
| Treatment | No treatment required unless symptomatic; fiber for mild symptoms | Antibiotics, bowel rest, possible hospitalisation or surgery in severe cases |
Frequently Asked Questions (FAQs) on Diverticulosis
Is diverticulosis reversible?
Diverticulosis is considered to be a permanent structural alteration of the colon, and diverticula cannot be reversed. A healthy weight, a decrease in red meat consumption, and an increase in dietary fibre are some examples of lifestyle changes that may help stop the disease's progression and effects. Even while the diverticula themselves do not decrease, these steps can greatly lower the probability of developing symptoms.
What foods aggravate diverticulosis?
Excessive intake of red meat, fat, and refined grains can exacerbate diverticulosis and raise the risk of diverticulitis. On the other hand, a lower risk of complications is linked to diets high in fibre from fruits, vegetables, and whole grains. Nuts, seeds, and popcorn do not appear to exacerbate diverticulosis; in fact, they may even be protective.
Can diverticulosis heal?
Diverticulosis (the presence of diverticula) itself does not heal or go away, as the pouches are permanent structural changes in the colon wall. However, mild, uncomplicated diverticulitis (inflammation of the diverticula) can resolve on its own or with conservative treatment such as rest, dietary modification, and sometimes antibiotics.
Diverticulosis coli best treated with?
Diverticulosis coli (the presence of colonic diverticula without inflammation or complications) is best managed with lifestyle and dietary modifications, primarily increasing dietary fiber, adequate fluid intake, and regular exercise. Most patients are asymptomatic and do not require medication. Antibiotics, bowel rest, and surgery are reserved for cases that progress to diverticulitis or develop complications.
What is the difference between diverticulitis and diverticulosis?
Diverticulosis describes the presence of tiny pouches (diverticula) in the colon wall, which are usually accidentally found and are asymptomatic. When these pouches become inflamed or infected, diverticulitis develops, resulting in symptoms like fever, altered bowel habits, and abdominal pain. The main difference is that diverticulitis is an acute, symptomatic complication that necessitates medical attention, whereas diverticulosis is usually a benign, chronic condition.
Does diverticulosis cause stomach pain?
Most people with diverticulosis have no symptoms of stomach pain because the condition is usually asymptomatic, and diverticulitis or other gastrointestinal disorders are more frequently linked to abdominal pain. Diverticulosis symptoms are uncommon and generally only appear when complications develop.
What is colonic diverticulosis?
Colonic diverticulosis is defined as the presence of one or more sac-like protrusions, known as diverticula, in the wall of the colon. These diverticula are pseudodiverticula, meaning they involve herniation of the mucosa and submucosa through the muscular layer of the colon. The condition is commonly asymptomatic, but in some cases, diverticula may become inflamed or bleed, leading to clinical symptoms or complications.
What is severe diverticulosis?
The condition known as severe diverticulosis is characterised by a large number or frequent distribution of diverticula throughout the colon, which is frequently linked to a higher risk of complications like bleeding, inflammation, perforation, or the development of an abscess. severe diverticulosis can cause serious clinical manifestations and require more intensive management, including medical or surgical intervention, particularly if complications arise, even though the majority of cases remain asymptomatic.
Are enemas good for diverticulosis?
Enemas are generally not recommended for diverticulosis. Both laxatives and enemas must be avoided in people with diverticular disease, as they can worsen symptoms or potentially lead to complications. The preferred approach for managing diverticulosis is to increase dietary fibre and fluid intake to help maintain regular bowel movements and reduce the risk of constipation, rather than using enemas or laxatives.
Which is worse, diverticulitis or diverticulosis?
Diverticulitis is worse than diverticulosis since it presents with inflammation or infection of the diverticula, and thus has more severe symptoms than diverticulosis, including abdominal pain, fever, and possible complications like abscess, perforation, or peritonitis. Diverticulitis, in contrast, can lead to severe health consequences and might even need medical or surgical treatment.
What does mild sigmoid diverticulosis mean?
The presence of small diverticula, which are tiny, rising pouches, in the sigmoid colon, the lower portion of the large intestine, is known as mild sigmoid diverticulosis. This is a common condition that usually has no symptoms, especially in older adults. The majority of people with mild sigmoid diverticulosis do not exhibit any symptoms, and the condition is frequently found by chance when imaging or a colonoscopy is done for another purpose.
How to remove pouches of diverticulosis?
The pouches of diverticulosis, known as diverticula, cannot be removed without surgery. Surgical removal, such as a sigmoid resection, is generally reserved for patients with severe, recurrent, or complicated disease, including persistent symptoms, bleeding, or complications like fistulas or strictures.
What is descending and sigmoid diverticulosis?
Descending and sigmoid colon diverticulosis is a condition where small pouches (diverticula) form and bulge outward through weak spots in the wall of the colon, most commonly in the sigmoid and descending regions. Most people have no symptoms, but complications like inflammation (diverticulitis) or bleeding can occur.
Will the platelet count fall in multiple pan-colonic diverticulosis?
In the majority of cases, pan-colonic diverticulosis is unlikely to cause a decrease in platelet count. In actuality, diverticulosis by itself usually does not affect platelet counts. Nevertheless, depending on the circumstances, diverticulosis complications like bleeding or infection (diverticulitis) may cause the platelet count to rise or fall.
When to consult a doctor for diverticulosis?
Consult a doctor for diverticulosis if you experience persistent abdominal pain, frequent bloating, or long-term changes in bowel habits such as constipation or diarrhoea. Signs that indicate a need for medical assistance are:
- Rectal bleeding
- Unexplained weight loss
- Ongoing abdominal discomfort
- Digestive issues that affect daily life
If these symptoms continue, it is best to see a diverticulosis doctor for proper evaluation and care. Seek emergency medical attention if you suddenly develop strong abdominal pain, fever, nausea, or vomiting, as these can be signs of diverticulitis or serious complications. A primary care doctor or gastroenterologist can provide the proper diverticulosis treatment to control symptoms and lower future risks.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles