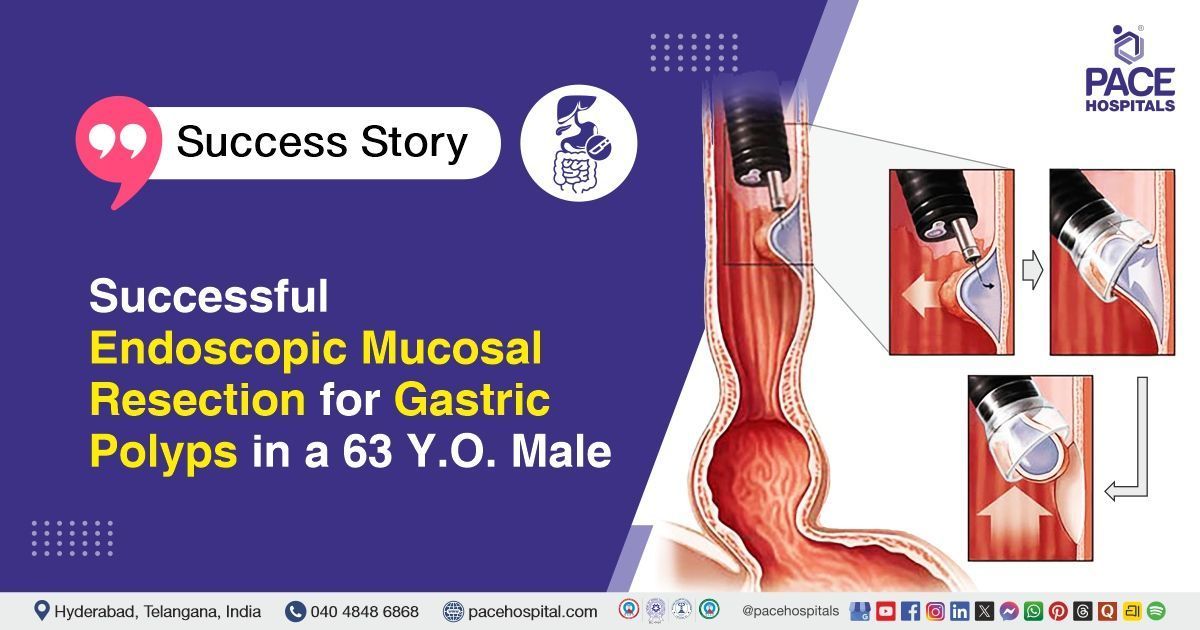
Successful Endoscopic Mucosal Resection for Gastric Polyps in a 63 Y.O. Male
PACE Hospitals
PACE Hospitals’ expert Gastroenterology team successfully performed an Endoscopic Mucosal Resection (EMR) on a 63-year-old male patient diagnosed with gastric fundal polyps. The procedure was aimed at removing the polyps and preventing potential progression to gastric cancer.
Chief Complaints
A 63-year-old male with a
body mass index (BMI) of 21.3 presented to the Gastroenterology Department at
PACE Hospitals, Hitech City, Hyderabad, with a one-month history of epigastric abdominal pain and persistent nausea.
Past Medical History
The patient had a history of diabetes mellitus, which was poorly controlled, with an HBA1C indicating inadequate glycemic control. He also had hypertension and dyslipidemia, with laboratory reports showing elevated triglycerides. Additionally, he had benign prostatic hyperplasia (BPH).
On Examination
On examination, the patient was conscious, coherent and oriented . Vital signs were normal. Abdominal examination revealed a soft, non-tender abdomen. Cardiovascular, respiratory, and other systemic examinations were normal.
Diagnosis
Upon admission to PACE Hospitals, the patient was thoroughly evaluated by the Gastroenterology team. He presented with abdominal pain in the epigastric region and nausea for one month. Past medical history included diabetes mellitus, hypertension, dyslipidemia, and benign prostatic hyperplasia (BPH).
The patient underwent necessary investigations. Upper gastrointestinal endoscopy revealed a small sessile polyp 2 cm below the gastroesophageal junction with surrounding ulceration and another sessile polyp measuring 6 mm in the body of the stomach. CECT abdomen (Contrast-Enhanced CT) showed grade II fatty liver, a simple cortical cyst in the right kidney, and a small fat-containing umbilical hernia. Ultrasound abdomen and pelvis confirmed altered liver echotexture, right renal cyst, and otherwise normal findings. Routine laboratory investigations, including complete blood picture, renal and liver function tests, electrolytes, coagulation profile, thyroid profile, lipid profile, and urine examination, were largely within normal limits, except for elevated HbA1c (8.7%) and hypertriglyceridemia (259 mg/dl), indicative of uncontrolled diabetes mellitus and dyslipidemia.
Based on the confirmed diagnosis, the patient was advised to undergo Gastric polyps Treatment in Hyderabad, India, under the expert care of the Gastroenterology Department, to manage the condition and prevent complications.
Medical Decision Making (MDM)
After a detailed consultation with consultant gastroenterologists, Dr. Govind Verma, Dr. M. Sudhir, Dr. Padma Priya, and cross consultation with general physician, Dr. Mounika Jetti, and with maxillofacial surgeon Dr. B Arvind a thorough evaluation was conducted considering the patient’s complaints of epigastric pain, nausea, abdominal discomfort, along with a history of Metabolic Dysfunction–Associated Steatotic Liver Disease (MASLD), diabetes mellitus, dyslipidemia, hypertension, and benign prostatic hyperplasia (BPH). All relevant laboratory, imaging, and prior procedural data were reviewed.
Based on these clinical and imaging findings, it was determined that Endoscopic Mucosal Resection (EMR) of gastric fundal polyps was identified as the most appropriate intervention to remove the polyps, obtain histopathology, prevent potential complications, including malignant transformation, and relieve gastrointestinal symptoms.
The patient and his family members were counselled regarding the diagnosis, the planned procedure, its associated risks, including bleeding, perforation, or infection, and its potential to relieve symptoms, improve digestive function, and prevent further complications related to gastric polyps.
Surgical Procedure
Following the decision, the patient was scheduled to undergo an Endoscopic mucosal resection procedure in Hyderabad at PACE Hospitals under the expert care of the Gastroenterology Department.
The following steps were carried out during the procedure:
- Preparation and Anesthesia: The patient was brought to the endoscopy suite and placed under general anesthesia. Standard aseptic precautions were followed, including sterile drapes and equipment preparation. The patient’s vital signs were continuously monitored throughout the procedure.
- Lesion Identification and Marking: An upper gastrointestinal endoscope was introduced through the mouth to visualize the gastric fundus. The polyp located 2 cm below the gastroesophageal junction and the smaller polyp in the body were identified. Dye was injected at the base of the polyp to lift the lesion and delineate its margins for safe resection.
- Polyp Resection: A snare device was advanced through the endoscope. The polyp was captured with the snare and resected en bloc, removing the entire polyp in one piece. The resected polyp measured approximately 1.5 x 1.4 cm.
- Hemostasis and Site Management: After resection, bleeding at the polyp base was controlled using Argon Plasma Coagulation (APC). The resection site was carefully inspected for any residual tissue or active bleeding.
- Final Inspection and Completion: The site was thoroughly examined to ensure complete removal of the lesion and adequate hemostasis. The procedure was concluded successfully without immediate complications.
Postoperative Care
The procedure was uneventful. Post-procedure, the patient was initially kept nil per oral (NPO) and was started on liquids on the first day, which were well tolerated. He was subsequently advanced to a soft diet. The patient was advised to undergo liver elastography and consult endocrinology, but opted for follow-up in the outpatient department. He was stable, symptomatically improved, and was discharged with appropriate medical instructions.
Discharge Medications
Upon discharge, the patient was prescribed medications for the management of gastric acid suppression, blood sugar control, hypertension, urinary symptoms related to prostate enlargement, lipid management, nutritional supplementation, and gastric mucosal protection. These medications were intended to support glycemic control, maintain blood pressure within normal limits, improve lipid profile, manage lower urinary tract symptoms, promote healing of the gastric mucosa after polyp removal, and provide necessary nutritional support during recovery.
Advice on Discharge
The patient was advised to follow a diabetic-appropriate diet to help maintain optimal blood sugar levels and support overall health.
Emergency Care
The patient was informed to contact the emergency ward at PACE Hospitals in case of any emergency or development of symptoms such as fever, abdominal pain, or vomiting.
Review and Follow-up Notes
The patient was advised to return for a follow-up visit with the Gastroenterologist in Hyderabad at PACE Hospitals after 2 weeks for further evaluation and follow-up visit with the endocrinologist in view of uncontrolled Diabetes mellitus (DM) as early as possible.
Conclusion
This case highlights the successful management of gastric fundal polyps in a patient with metabolic and systemic comorbidities. The endoscopic mucosal resection was performed uneventfully under general anesthesia, and post-procedure recovery was smooth with stable vitals. The patient was discharged in stable condition with medical management, dietary advice, and planned follow-up for further evaluation of liver and endocrine status.
Integrated Approach to Gastric Polyps in Patients with Metabolic Risk
Management of gastric polyps requires careful evaluation of gastrointestinal findings alongside systemic health, especially in patients with metabolic conditions like diabetes, dyslipidemia, or fatty liver disease. Pre-procedure assessment should include imaging, blood tests, and risk stratification to guide safe endoscopic interventions. Endoscopic mucosal resection is an effective minimally invasive technique for removing polyps while controlling procedure-related complications.
Post-procedure care involves gradual dietary progression, monitoring for bleeding or infection, and ongoing management of underlying metabolic disorders. Coordination with a gastroenterologist/gastroenterology doctor ensures appropriate procedural planning and follow-up. Regular follow-up and targeted investigations, such as liver elastography or metabolic optimization, support long-term health and preventive care.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles