Peptic Ulcer - Types, Symptoms, Causes, Diagnosis & Treatment
PACE Hospitals
Peptic ulcer disease definition
A peptic ulcer is an open sore that develops in the lining of the stomach (gastric ulcer) or the first part of the small intestine, called the duodenum (duodenal ulcer). These ulcers form when the protective lining of the duodenum or stomach is damaged, allowing stomach acid to irritate the surrounding tissue. The most common causes are Helicobacter pylori infection and prolonged use of nonsteroidal anti-inflammatory drugs (NSAIDs).
Symptoms of a peptic ulcer include burning or gnawing pain in the upper abdomen, bloating, nausea, vomiting, loss of appetite, and, in more severe cases, passing black stools or vomiting blood. Complications may include bleeding, perforation of the stomach or intestines, and blockage of the digestive tract.
Peptic ulcers are primarily managed by healthcare professionals, such as primary care physicians and gastroenterologists, who are responsible for diagnosing, treating, and managing the condition.
Peptic ulcer disease meaning
The term "peptic ulcer" comes from the Greek word "peptikos", meaning "digestive," and the Latin word "ulcus", meaning "sore" or "wound."
The word "peptic" refers to the digestive process, specifically involving gastric acid and the enzyme pepsin, which are essential for breaking down food in the stomach. Therefore, a peptic ulcer is a sore in the lining of the upper digestive tract, most commonly the stomach or duodenum, caused or worsened by the corrosive effects of digestive acids and enzymes.
Epidemiology of Peptic Ulcer Disease Worldwide
Incidence of peptic ulcer worldwide
The global incidence of peptic ulcer disease is estimated to be 0.3% to 1.9% each year. This indicates that up to two out of every 100 individuals may develop a new peptic ulcer each year. Although the number of cases has dropped in many countries because of increased awareness and treatment, it remains a major health concern in both industrialised and developing nations.
Peptic ulcer prevalence worldwide
Peptic ulcer disease (PUD) affects a significant percentage of the global population, with an estimated lifetime prevalence of 5-10%.
Epidemiology of Peptic Ulcer Disease in India
Incidence of peptic ulcer in India
Peptic ulcer disease in India affects approximately 0.1% to 0.3% of the population each year, meaning that one to three new cases occur per 1,000 people annually.
Prevalence of peptic ulcer in India
The prevalence of peptic ulcer disease in India varies by region and population group, but studies estimate that about 4% to 10% of the population may be affected at any given time. This means that up to 1 in 10 individuals in India could be living with peptic ulcer disease, highlighting it as a notable public health concern in the country.
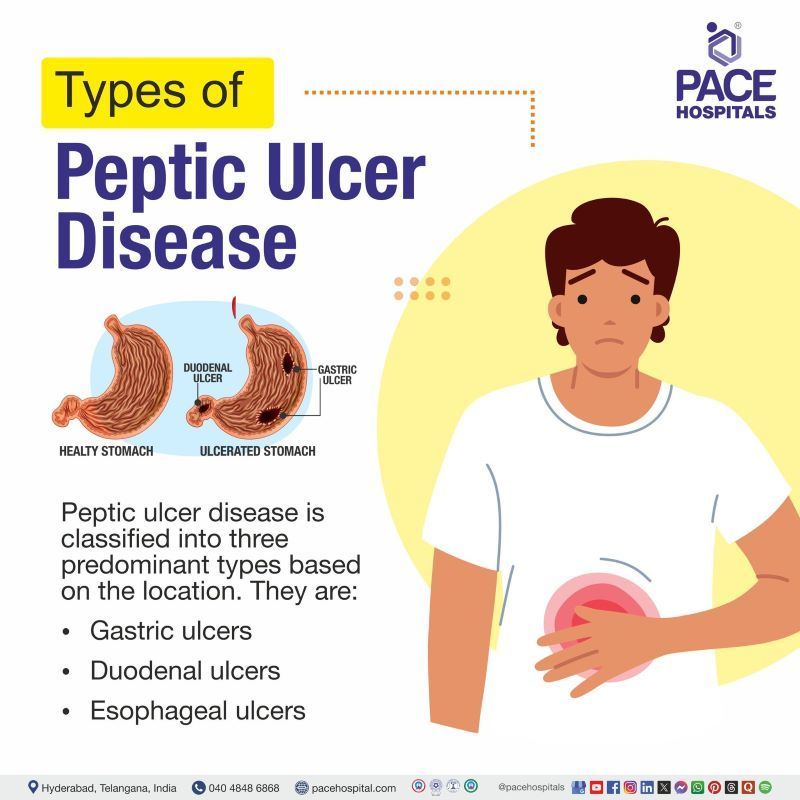
Types of Peptic Ulcer
Depending on where the damage occurs, peptic ulcers are categorized into different types affecting the stomach, the beginning of the small intestine, or the lower part of the esophagus.
Main types of peptic ulcer disease include:
- Gastric ulcers
- Duodenal ulcers
- Esophageal ulcers
Gastric ulcers: These ulcers form on the inner lining of the stomach. They are often associated with pain that worsens shortly after eating, as the stomach produces more acid to digest food.
Duodenal ulcers: These occur in the duodenum, which is the first part of the small intestine just beyond the stomach. Pain from duodenal ulcers often improves with eating, but may return a few hours later, especially when the stomach is empty.
Esophageal ulcers: These are less common and develop in the lower part of the esophagus. They are usually caused by acid reflux or the long-term use of certain medications that irritate the esophageal lining.
Peptic ulcer classification based on cause
Peptic ulcers can also be classified based on their underlying cause. Understanding what triggers an ulcer helps guide effective treatment.
Types of peptic ulcers based on cause include the following:
- Helicobacter pylori (H. pylori)–associated ulcers
- NSAID-induced ulcers
- Stress ulcers
Helicobacter pylori (H. pylori)–associated ulcers: Caused by infection with H. pylori, a common type of bacteria that weakens the protective lining of the stomach or small intestine, making it more prone to acid damage.
NSAID-induced ulcers: Result from frequent or long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or aspirin. These medications can irritate or erode the lining of the digestive tract over time.
Stress ulcers: These develop in response to severe physical stress, such as serious illness, trauma, or major surgery. They are commonly seen in hospitalized patients and may occur suddenly.
Peptic Ulcer Pathophysiology
Peptic ulcers develop when the protective mechanisms of the stomach or duodenum are overwhelmed by damaging factors, leading to tissue erosion and ulcer formation. The key players are imbalances between aggressive factors like stomach acid and pepsin, and protective factors like mucus, bicarbonate, and blood flow.
Mechanisms involved
Harmful (Aggressive) Factors
These are the elements that can damage the lining of the stomach or duodenum:
- Stomach Acid and Digestive Enzymes (like pepsin): These substances are essential for breaking down food, but in excess, they can irritate and erode the protective lining.
- H. pylori Infection: A common type of bacteria called Helicobacter pylori can live in the stomach lining. It causes inflammation and weakens the stomach’s natural defenses, allowing acid to do more damage. It can also interfere with substances that normally help neutralize acid.
- NSAID Use (Pain Relievers): Medications like aspirin, ibuprofen, and naproxen can reduce the stomach’s ability to protect itself. These drugs lower levels of natural chemicals (called prostaglandins) that help maintain the stomach lining and regulate acid production.
Protective Factors
These are the body’s natural defenses that help prevent damage:
- Mucus and Bicarbonate: Mucus coats the stomach lining, and bicarbonate helps neutralize acid. Together, they form a barrier that protects the tissue underneath.
- Blood Flow to the Stomach Lining: Good blood flow brings oxygen and nutrients to the tissue and helps remove waste. It also supports healing when there is damage.
- Prostaglandins: These natural chemicals support mucus and bicarbonate production, help control acid levels, and keep the stomach lining healthy.
Imbalance and Ulcer Development:
If the harmful factors become too strong or the protective factors become too weak, the stomach or intestinal lining starts to break down and may lead to:
- Surface Damage (Erosion): The first stage involves damage to the outermost layer of the lining.
- Ulcer Formation: If the damage goes deeper, it creates a true ulcer which may cause a break in the tissue that cause pain, bleeding, or other problems.
In summary, peptic ulcers are developed by a breakdown in the natural balance of the digestive system. When damaging factors like acid, bacteria, or medications overpower the body’s defenses, the lining becomes vulnerable. This leads to erosion and eventually ulcer formation, with the potential for serious complications if not treated properly.
Peptic Ulcer Symptoms
Recognizing the peptic ulcer disease symptoms early is crucial for timely diagnosis and effective treatment. Since many people may have ulcers without symptoms, awareness of the clinical manifestation of peptic ulcer is important to prevent serious complications.
Signs and symptoms of peptic ulcer disease include:
- Burning stomach pain
- Bloating
- Feeling full quickly
- Frequent burping
- Nausea
- Vomiting
- Loss of appetite
- Unexplained weight loss
- Black or tarry stools
- Vomiting blood
- Indigestion or upper abdominal discomfort
- Pain between meals or at night
- Burning Stomach Pain: One of the most common and noticeable symptoms. This pain is usually felt in the upper middle part of the abdomen and is often described as burning, gnawing, or aching. It tends to occur when the stomach is empty, such as between meals or at night. The pain may improve for a short time after eating or taking antacids, but then returns. The reason this happens is that stomach acid irritates the raw area of the ulcer, which doesn’t have the same protective layer as healthy tissue.
- Bloating: Many people with peptic ulcers feel a sense of bloating or tightness in their abdomen, especially after eating. This happens because the ulcer interferes with the stomach’s normal digestion process, slowing down how it empties. This delayed emptying leads to gas buildup, causing discomfort and a feeling of fullness or swelling.
- Feeling Full Quickly: People with ulcers often feel full after eating just a small amount of food. This is not because the stomach is full, but because the ulcer can irritate the nerves that signal fullness. As a result, even a light meal may lead to a sensation of being overly full or uncomfortable.
- Frequent Burping: Burping more than usual can be a sign of a peptic ulcer. This happens when the ulcer causes irritation that slows digestion and leads to more gas in the stomach. Additionally, discomfort from the ulcer may lead to swallowing more air, which results in burping as the body tries to release the trapped air.
- Nausea: Nausea is a common symptom and often occurs because the ulcer disrupts the normal movement and function of the stomach. When food and acid linger too long in the stomach, it causes irritation and the uneasy feeling known as nausea. In some people, the nausea may come and go, while in others it might be constant.
- Vomiting: In more severe cases, nausea may be followed by vomiting. This occurs when the ulcer causes enough irritation or blockage to prevent the stomach from emptying properly. The body then tries to relieve the pressure by forcing the contents out. If vomiting is persistent or contains blood, medical attention is urgently needed.
- Loss of Appetite: Discomfort, pain, or nausea associated with eating can lead people to avoid food, even when they are hungry. Over time, this pattern of eating less becomes more noticeable. The fear of pain or feeling unwell after eating can cause appetite to decrease significantly.
- Unexplained Weight Loss: Weight loss may result from eating less due to pain, nausea, or a lack of appetite. When food intake is consistently low, the body begins to use stored energy, leading to visible weight loss. This is especially concerning if the weight loss happens without trying or making dietary changes.
- Black or Tarry Stools: This is a sign of bleeding inside the digestive tract. When an ulcer bleeds slowly, the blood passes through the intestines and gets broken down by digestive enzymes. This turns the stool black and sticky, similar to tar. It may also have a distinct foul smell. This symptom suggests internal bleeding and needs to be reported to a doctor immediately.
- Vomiting Blood: If an ulcer causes a blood vessel to break, it can lead to bleeding directly into the stomach. When this blood is vomited, it may look bright red or resemble coffee grounds, depending on how long it’s been there. This is a serious symptom that indicates active internal bleeding and requires urgent medical care.
- Indigestion or Upper Abdominal Discomfort: A peptic ulcer often causes a general feeling of discomfort in the upper stomach, particularly after meals. It may feel like burning, pressure, or cramping. This happens because the ulcer affects how the stomach handles food and acid, leading to irritation and an upset stomach.
- Pain Between Meals or at Night: Ulcer pain commonly occurs when the stomach is empty. Without food to absorb the acid, the stomach lining is more exposed, making the ulcer area more irritated. This often leads to discomfort between meals or during the night, which may wake a person from sleep.
Peptic Ulcer Causes
Peptic ulcers develop when the balance between aggressive factors and the protective mechanisms of the gastrointestinal mucosa is disrupted. A variety of physiological, pathological, and pharmacological influences can contribute to this imbalance. Understanding these underlying causes is essential for effective prevention, diagnosis, and management.
The major causes linked to peptic ulcer formation are as follows:
- Infection with Helicobacter pylori (H. pylori)
- Use of Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Infection with Helicobacter pylori (H. pylori)
H. pylori is a type of bacteria that lives in the lining of the stomach. It weakens the stomach’s natural protective layer by producing certain chemicals that cause irritation and long-term inflammation. This ongoing irritation reduces the stomach’s ability to protect itself from acid, which can lead to the development of ulcers, especially in the lower part of the stomach and the beginning of the small intestine.
Chronic use of Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
NSAIDs are commonly used pain-relieving medications. They cause ulcers by blocking substances in the body that help protect the stomach lining. Without this protection, the stomach and small intestine become more likely to get damaged by stomach acid, leading to ulcers.
Other, less common causes of peptic ulcer disease
- Other Infections: Besides H. pylori- bacteria that causes peptic ulcers, some viruses, fungi, and other types of bacteria can also damage the stomach lining. These infections can lead to inflammation and make the lining more sensitive to acid, which increases the chance of ulcers forming.
- Medications (Other than NSAIDs): Some other types of medications can also irritate or damage the stomach. They may do this by increasing acid levels, slowing down the healing of the stomach lining, or causing direct irritation. When combined with NSAIDs, the risk of ulcers becomes even higher. Drugs that cause peptic ulcers other than NSAIDS include corticosteroids, certain chemotherapy agents, potassium supplements, and medications used to treat osteoporosis.
- Zollinger-Ellison Syndrome: This is a rare condition in which small tumors cause the stomach to make too much acid. The extra acid breaks down the protective lining of the stomach and small intestine, often leading to serious and hard-to-treat ulcers.
- Physiological Stress from Severe Illness or Trauma: Very serious health conditions like major surgeries, severe infections, or organ failure can reduce blood flow to the stomach. This weakens the stomach’s ability to protect itself, making it easier for ulcers to form during times of critical illness.
- Other Medical Conditions: Some diseases and health problems can lead to ulcers by damaging the stomach lining or increasing acid levels. These include conditions like chronic inflammation in the gut, poor blood flow to the stomach, certain infections, cancers, and exposure to radiation in the upper abdomen. These issues interfere with the stomach’s natural healing and defense systems, raising the risk of ulcers.
Peptic Ulcer Risk Factors
While peptic ulcers are primarily caused by specific agents, several factors can increase the likelihood of their development. These risk factors do not directly cause ulcers but can weaken the stomach’s defenses or enhance the effects of harmful agents.
The key risk factors for peptic ulcer disease include the following:
- Use of Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- Smoking
- Excessive Alcohol Consumption
- Older Age
- High Levels of Physical or Emotional Stress
- Irregular Eating Habits or Poor Diet
- Family History of Peptic Ulcers
- Use of Nonsteroidal Anti-inflammatory Drugs (NSAIDs): Frequent or long-term use of NSAIDs reduces the production of protective substances in the stomach lining. These substances normally help maintain a healthy barrier against stomach acid. When they are suppressed, the lining becomes thinner and more fragile, making it easier for acid to damage the tissue and lead to ulcer formation.
- Smoking: Smoking introduces harmful chemicals into the body that reduce blood flow to the stomach lining. It also increases the production of stomach acid and interferes with the natural repair processes of the stomach. Together, these effects weaken the stomach’s defenses and create a higher risk for ulcers to develop and heal poorly once formed.
- Excessive Alcohol Consumption: High intake of alcohol can directly irritate the stomach lining and erode its protective barrier. It also increases acid production and slows down the healing of small injuries or irritation in the stomach. Over time, repeated damage combined with impaired healing can result in ulcer formation.
- Older Age: As individuals age, the stomach’s ability to maintain and repair its protective lining becomes less efficient. Aging also increases the likelihood of using medications that affect the stomach, such as NSAIDs. These combined factors reduce resistance to acid damage and raise the risk of developing ulcers.
- High Levels of Physical or Emotional Stress: Severe stress, especially caused by serious illness, injury, or surgery, can disrupt normal blood flow to the stomach. This reduces oxygen and nutrient supply to the stomach lining, weakening its protective functions. Stress may also affect nerve signals that regulate acid production, creating conditions favorable for ulcer formation.
- Irregular Eating Habits or Poor Diet: Skipping meals, overeating, or consuming highly acidic or irritating foods does not directly cause ulcers but can lead to increased acid secretion and stomach discomfort. These dietary patterns may contribute to an environment that delays healing and increases vulnerability to ulcer development when combined with other risk factors.
- Family History of Peptic Ulcers: A family history of peptic ulcers may indicate inherited traits that influence acid production, stomach lining protection, or sensitivity to certain environmental or medication-related triggers. These genetic factors can make some individuals more prone to ulcer development under certain conditions.
Complications of Peptic Ulcer
Complications often arise when ulcers go untreated or become chronic. The most common complications of peptic ulcer are primarily due to the ongoing erosion of the stomach, which can lead to significant medical issues. Recognizing the potential complications of peptic ulcers is essential for prompt intervention and to prevent life-threatening outcomes.
Peptic ulcer disease (PUD), if not diagnosed and treated promptly, can indeed lead to serious complications. The main complications that can occur in PUD include:
- Upper gastrointestinal bleeding
- Gastric outlet obstruction
- Perforation
- Penetration
- Gastric cancer
- Hypovolemia and Shock
- Sepsis
- Gastrocolic Fistula
- Upper gastrointestinal bleeding: This is the most frequent complication, occurring when an ulcer erodes into a blood vessel. It may present as vomiting blood (hematemesis), black, tarry stools (melena), or anemia. Severe bleeding can become life-threatening and often requires urgent endoscopic or surgical treatment.
- Gastric Outlet Obstruction: This complication can happen when a peptic ulcer forms near the lower part of the stomach or the beginning of the small intestine. Over time, swelling or scarring from the ulcer can block the normal passage of food. When this blockage happens, food cannot move forward easily, which can lead to symptoms like feeling full quickly, bloating, vomiting, and unintentional weight loss.
- Perforation: In some cases, a peptic ulcer can be worn all the way through the wall of the stomach or small intestine. When this happens, the contents inside the stomach can leak into space around the organs. This is very dangerous and causes sudden, severe pain. It can lead to a serious infection in the belly, and immediate surgery is usually needed to treat it.
- Penetration: A deep ulcer may continue to grow and reach nearby organs, such as the pancreas or liver. Instead of causing a hole into the open space, the ulcer "sticks" to another organ. This can cause strong, long-lasting pain that may spread to the back. Medical treatment and sometimes surgery are needed to manage this complication.
- Gastric Cancer: Although rare, ulcers in the stomach that don’t heal over time might slowly change in a harmful way. This long-lasting damage can, in some cases, lead to the development of stomach cancer. This risk is higher with stomach ulcers than with those in the small intestine. Close medical follow-up and testing are important for ulcers that keep coming back or do not heal with treatment.
- Hypovolemia and Shock: A bleeding ulcer can cause a large amount of blood loss. If too much blood is lost, the body may not have enough fluid to keep blood pressure stable. This can lead to serious problems, such as the heart and other organs not getting enough oxygen. This condition is life-threatening and requires urgent care to replace the lost blood and stabilize the body.
- Sepsis: When a perforated ulcer causes an infection inside the belly, bacteria can sometimes spread into the bloodstream. This can trigger a widespread reaction throughout the body, known as sepsis. It can affect many organs at once and become life-threatening. Quick and strong medical treatment is needed to control the infection and support the body.
- Gastrocolic Fistula: In rare situations, a deep ulcer may create an unusual passage between the stomach and the large intestine. This is known as a fistula. When this happens, food may pass too quickly through the digestive system, leading to problems like constant diarrhea, poor absorption of nutrients, and increased risk of infection.
Peptic Ulcer Diagnosis
Identifying a peptic ulcer begins with understanding the symptoms and recognizing patterns that may suggest damage to the stomach or intestinal lining. Patients often first visit a general physician for initial evaluation. If an ulcer is suspected, they are usually referred to a gastroenterologist (specialist in digestive health) for further assessment. Early diagnosis plays a key role in preventing complications and guiding effective care.
The diagnostic approach to detect peptic ulcers include the following:
- Patient History and Physical Exam: The gastroenterologist will ask about any symptoms such as stomach pain, bloating, or nausea. Questions may also cover past illnesses and daily habits. A physical exam is done to gently press on the stomach area to check for discomfort, especially in the upper middle part of the belly.
- Blood Tests: Blood samples can be used to check for signs of infection linked to ulcers. These tests may also show if there is a low blood count, which can happen if there has been bleeding. In some cases, they help look for problems with how the body handles certain medicines.
- Stool Tests: A small sample of stool (bowel movement) may be collected to check for signs of infection. This can help identify if a certain type of bacteria that is commonly linked to ulcers is present in the body.
- Urea Breath Test: This test involves breathing into a special container before and after drinking a safe solution. If certain bacteria are present in the stomach, the test can detect them by measuring changes in the air that is breathed out
- Upper GI Endoscopy (EGD): This is a procedure where a thin, bendable tube with a light and camera is gently passed through the mouth into the stomach and small intestine. It allows doctors to see the inside of the digestive system clearly. Small samples of tissue may be taken during the procedure to check for infection or other conditions.
- Upper GI Series (Barium Swallow): In this test, a person drinks a special liquid that coats the inside of the digestive system. X-ray images are then taken, which help highlight any sores or irregular areas in the stomach or upper intestine.
- Imaging Tests (CT scans): These scans use advanced X-ray technology to take detailed pictures of the inside of the body. They are especially useful when there are signs of serious problems, such as holes in the stomach wall or fluid collections caused by complications.
Peptic Ulcer Treatment
Management of peptic ulcer disease involves a stepwise approach that begins with addressing the cause of peptic ulcer and making lifestyle modifications. Each patient's treatment varies according to the cause of peptic ulcer, the intensity of their symptoms, and whether any complications are present. In some situations, advanced therapies or surgical intervention may be necessary to manage severe or complicated ulcers and ensure long-term recovery
Peptic ulcer disease treatment includes:
- Eradication of Helicobacter pylori
- Acid Suppression Therapy
- Gastrointestinal protectants
- Prostaglandin Analogues
- Treatment of peptic ulcer cause by other medications
- Treatment of Complications
- Surgical interventions (if needed)
- Lifestyle Modifications and Supportive Care
- Eradication of Helicobacter pylori: If an infection is found, treatment usually involves taking a combination of antibiotics along with medicines that reduce stomach acid. In certain cases where the infection is harder to treat, an additional substance may be added to help clear it. After the treatment is completed, follow-up testing is often done to make sure the infection is completely gone.
- Acid suppression therapy: Antisecretory drugs used in peptic ulcer disease include:
- Proton-pump inhibitors (PPIs)
- H2-receptor antagonists
Therapy is generally continued for 4–8 weeks, depending on ulcer size and location.
- Gastrointestinal protectants
- Cytoprotective agents help to coat and protect the ulcer base and promote healing.
- Bismuth compounds coat ulcers and exhibit mild antibacterial effects.
- Prostaglandin Analogues: Prostaglandin analogues are used to treat and prevent peptic ulcer disease, primarily by protecting the stomach lining. These drugs are especially useful in patients at high risk for ulcers, such as those on long-term NSAID therapy, as they counteract the harmful effects of reduced natural prostaglandins caused by NSAIDs.
- Treatment of Complications
- Bleeding ulcers: managed with endoscopic therapy (cauterization, clipping, injection)
- Perforation or gastric outlet obstruction: may require urgent surgical intervention).
- Surgical intervention (if needed): If the patient is noncompliant, not responding to medical treatment, or has a high risk of complications, surgery is recommended. Surgery is indicated in case of perforation, recurrent bleeding, and refractory ulcers.
- Lifestyle Modifications and Supportive Care: Patients are advised to stop smoking, limit alcohol, avoid foods that worsen symptoms, and manage stress. These measures support healing and reduce recurrence risk, though they are not primary treatments.
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
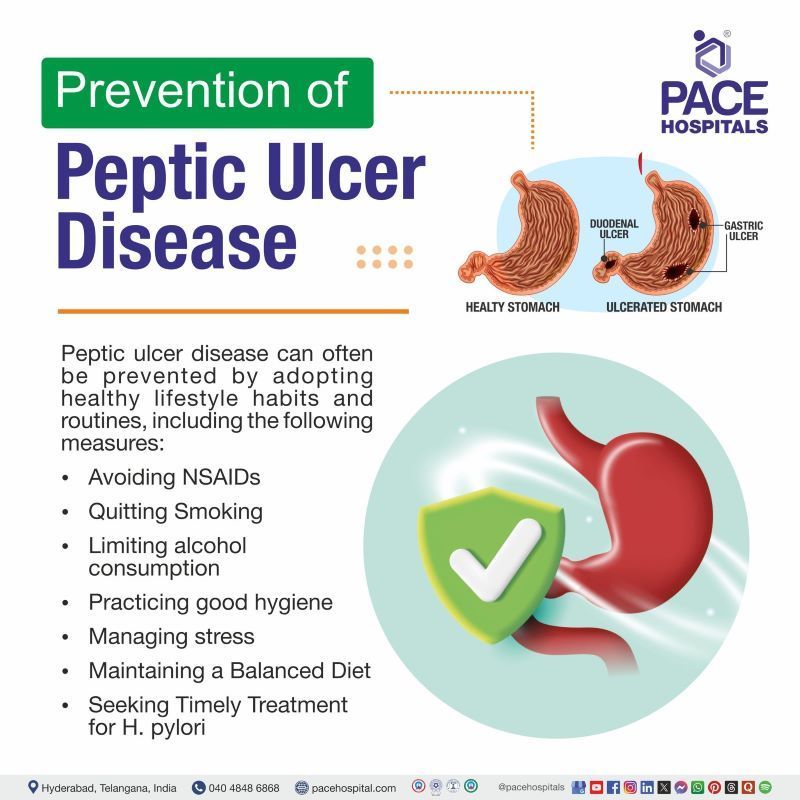
Prevention of Peptic Ulcer Disease
Preventing peptic ulcer disease involves reducing the factors that can harm the stomach lining or increase acid levels. Lifestyle changes, proper hygiene, and early treatment of infections play a key role in protecting the digestive system. Taking simple steps can lower the risk of ulcers and help maintain long-term stomach health.
The key strategies for preventing peptic ulcer disease are as follows:
- Avoiding NSAIDs
- Quitting Smoking
- Limiting alcohol consumption
- Practicing good hygiene
- Managing stress
- Maintaining a Balanced Diet
- Seeking Timely Treatment for H. pylori
- Avoiding NSAIDs: Staying away from certain pain-relieving medicines helps protect the stomach lining. These medications can wear down the stomach’s natural barrier, making it more likely for ulcers to form. Avoiding or limiting their use lowers this risk and helps keep the stomach lining intact.
- Quitting Smoking: Stopping smoking strengthens the stomach’s ability to defend itself. Smoking increases acid levels and slows healing, which makes the stomach more vulnerable to ulcers. Quitting helps reduce the damage and allows the stomach lining to stay healthy and heal properly.
- Limiting Alcohol Consumption: Cutting down on alcohol helps prevent irritation to the stomach lining. Alcohol can weaken the protective layer and increase acid, both of which raise the risk of ulcers. Limiting intake gives the stomach a better chance to stay protected and function normally.
- Practicing Good Hygiene: Washing hands regularly and eating clean, safe food helps reduce the chance of getting infected with harmful bacteria that can cause ulcers. Preventing infection keeps the stomach from becoming inflamed or damaged, which lowers the risk of ulcers forming.
- Managing Stress: Managing stress supports overall digestive health. High stress levels can lead to habits like smoking, drinking, or skipping meals, all of which raise the risk of ulcers. Staying active, eating regularly, and getting enough rest can reduce these habits and protect the stomach.
- Maintaining a Balanced Diet: A healthy diet supports the body’s ability to protect and heal the stomach lining. Fiber, fruits, vegetables, and whole grains help reduce inflammation and provide nutrients that repair tissue. Eating probiotic-rich foods may also help the body fight off harmful bacteria linked to ulcers.
- Seeking Timely Treatment for H. pylori: Getting early treatment for certain bacterial infections helps prevent long-term damage to the stomach. Removing the infection lowers inflammation and reduces the risk of ulcers forming. Early care also helps avoid complications like bleeding or blockages.
Difference Between Peptic Ulcer and Duodenal Ulcer
Peptic ulcer vs duodenal ulcer
Peptic ulcers are a broader category that includes sores in different parts of the upper digestive tract, while duodenal ulcers are a specific type that occurs in the first part of the small intestine. Understanding the difference helps in recognizing their location, symptoms, and treatment approach. The main differences between peptic ulcers and duodenal ulcers are as follows:
| Features | Peptic ulcer | Duodenal ulcer |
|---|---|---|
| Definition | Ulcers in the stomach or duodenum or esophagus | Ulcers specifically in the duodenum (first part of the small intestine) |
| Symptoms | Upper abdominal pain, bloating, nausea, and vomiting | Upper abdominal pain, heartburn, pain at night, or between meals |
| H. Pylori association | Frequently associated | Strongly associated |
| NSAIDs involvement | Often linked, especially gastric ulcers | Less commonly linked than gastric ulcers |
| Pain timing | Varies by location | Improves with meals, worsens when the stomach is empty |
| Location | Stomach or duodenum | Duodenum only |
| Age group | Occur in Any age group people | More common in 30-60 years |
Frequently Asked Questions (FAQs) on Peptic Ulcers
Can peptic ulcer be cured?
Yes, with the right care, the majority of peptic ulcers can be cured. If the cause is addressed, peptic ulcer cases heal in six to eight weeks with acid suppression medication, especially when using PPIs. A cure and prevention of recurrence depend on getting rid of the H. pylori infection or stopping NSAID use.
Where are peptic ulcers located?
Peptic ulcers can occur in the first segment of the small intestine (duodenal ulcers) or the stomach (gastric ulcers). Less frequently, they can develop in the oesophagus or in the stomach following stomach surgery (remnant gastric ulcers). For diagnostic and treatment planning, the location is crucial.
Can peptic ulcer be without symptoms?
Yes, peptic ulcers can be asymptomatic. Up to 70% of people with peptic ulcers may not exhibit any symptoms at all. These are called "silent ulcers." Only when the ulcer develops into a complication, such as bleeding or perforation, symptoms may appear.
Can peptic ulcer lead to cancer?
Peptic ulcers themselves do not directly cause cancer, but chronic Helicobacter pylori infection, a major cause of peptic ulcers, can lead to chronic gastritis and is a risk factor for gastric carcinoma. Most peptic ulcers heal with appropriate treatment, but persistent infection or inflammation may increase the risk of gastric cancer over time. Regular follow-up and eradication of H. pylori are recommended to reduce this risk.
why peptic ulcer is more common in blood group O?
Peptic ulcers are more common in people with blood group O due to certain inherited factors. Studies suggest that individuals with this blood type may have lower levels of natural substances that protect the stomach lining. They may also be more likely to get infected with the bacteria linked to ulcers. These factors together can weaken the stomach’s defenses and make it more prone to damage from stomach acid.
How to treat peptic ulcer?
Most peptic ulcers are treated with medications such as proton pump inhibitors (PPIs) or H2 receptor antagonists, which reduce stomach acid and protect the ulcerated area. If Helicobacter pylori infection is detected, a proton pump inhibitor (PPI) and two antibiotics are recommended. Stopping the offending substance and taking acid-reducing treatments are crucial for ulcers caused by NSAIDs. In severe situations, endoscopic or surgical intervention may be necessary.
How to cure peptic ulcer disease naturally?
Natural ways to help manage peptic ulcer disease, as supported by research, include using certain herbs like licorice, slippery elm, marshmallow root, aloe vera, chamomile, ginger, turmeric, meadowsweet, fenugreek, and cabbage. These herbs may help by reducing inflammation, fighting infection, and protecting the stomach lining. Along with a healthy diet, these remedies can support healing when used with regular treatments. However, their safety and possible interactions with other medicines need to be carefully considered.
Does alcohol cause peptic ulcers?
Alcohol can irritate and harm the stomach lining, which can worsen pre-existing ulcers or slow their recovery, but it does not directly cause peptic ulcers. Although it is not a major contributing factor like H. pylori infection or NSAID use, excessive alcohol use is discouraged for those with peptic ulcers.
Is peptic ulcer life threatening?
Although complications like bleeding, perforation, or obstruction can be dangerous and require immediate medical attention, peptic ulcers are generally not fatal when treated promptly. Most ulcers can be healed with the correct care, but in severe or persistent cases, surgery or other advanced techniques might be required to prevent potentially deadly outcomes.
How does smoking cause peptic ulcers?
Smoking contributes to the development of peptic ulcers in several harmful ways. It reduces blood flow to the stomach lining, which limits the supply of oxygen and nutrients needed for repair. Smoking also increases the production of stomach acid while lowering the production of protective mucus and bicarbonate. This weakens the natural defenses of the stomach and makes it more vulnerable to acid damage. Additionally, smoking may slow down healing and increase the risk of ulcer recurrence.
How long do peptic ulcers last?
Most peptic ulcers heal within a few days to weeks with proper care, but it can take up to six or eight weeks for complete healing. The duration depends on the patient's overall health, the size and location of the ulcer, adherence to treatment, and the underlying cause. Untreated or complicated ulcers are more likely to recur, cause complications, and take longer to heal.
Is curd good for peptic ulcer?
Yes, curd (yogurt) is considered helpful for managing peptic ulcers. Research shows that yogurt with live probiotics can lower the number of harmful bacteria linked to ulcers, support healing of the stomach lining, and ease symptoms. The probiotics in yogurt may also help reduce side effects from ulcer treatments and improve overall gut health. For the best results, it is recommended to choose yogurt that contains live and active cultures.
Is lemon bad for peptic ulcer?
Yes, the acidity of citrus fruits like lemons can irritate the stomach mucosa, which may make some people's symptoms worse. Although individual tolerance varies and not all patients experience worsening with citrus intake, the majority of guidelines advise avoiding highly acidic or spicy foods during active ulcer episodes.
Differentiate GERD vs peptic ulcer?
Peptic ulcer disease (PUD) and gastro-oesophageal reflux disease (GERD) both cause symptoms in the upper gastrointestinal tract, but they have different pathophysiology and complications. PUD involves stomach or duodenal mucosal breaks, which are frequently linked to Helicobacter pylori or NSAID use. In contrast, GERD is caused by reflux of gastric contents into the oesophagus, which results in heartburn and vomiting. While GERD usually does not result in ulceration, PUD can manifest as pain or bleeding.
What is the peptic ulcer investigation of choice?
The investigation of choice for diagnosing peptic ulcers is an upper gastrointestinal (GI) endoscopy (also called esophagogastroduodenoscopy or EGD) that directly visualizes the esophagus, stomach, and duodenum, allowing the gastroenterologists to see ulcers, assess their size and location, and take tissue biopsies if needed to test for Helicobacter pylori infection. Endoscopy not only confirms the diagnosis but also enables the treatment of complications such as bleeding ulcers during the procedure. Other tests, like blood, stool, or urea breath tests, are commonly used to detect H. pylori infection but do not replace endoscopy for direct ulcer diagnosis.
Is lower back pain a symptom of peptic ulcer?
Lower back pain is not a common symptom of peptic ulcer disease; however, in some cases, pain from a peptic ulcer, especially if the ulcer is severe or has penetrated nearby organs, such as the pancreas, can radiate to the back. This pain is usually felt in the mid or upper back rather than the lower back and often occurs alongside general ulcer symptoms, such as abdominal pain, nausea, or bloating. Persistent or severe back pain may indicate a complication, such as a perforating ulcer, and warrants immediate medical attention. If back pain occurs in isolation without other gastrointestinal symptoms, it is more likely due to another cause.
How NSAIDS cause peptic ulcer?
NSAIDs lead to peptic ulcers mainly by blocking substances in the body that help protect the stomach lining. This reduces the production of mucus and other protective fluids, lowers blood flow to the stomach, and weakens its natural defenses. As a result, the stomach becomes more easily damaged by its own acid. In addition, these medications can directly irritate the stomach lining, increasing the risk of ulcer formation.
When to consult a doctor for peptic ulcer?
Consult a doctor for a peptic ulcer when symptoms such as burning stomach pain, indigestion, or bloating last for more than a few days or interfere with eating and daily activities. Peptic ulcers can worsen without proper treatment and may lead to serious complications if ignored.
Warning signs that require medical attention include:
- Persistent stomach pain that improves with food but returns later
- Nausea, vomiting, or unexplained weight loss
- Black or tarry stools indicate bleeding.
- Vomiting blood that looks like coffee grounds
- Severe pain in the abdomen or chest
If these symptoms persist, a peptic ulcer doctor or a gastroenterologist can confirm the diagnosis and recommend the proper peptic ulcer treatment to promote healing and prevent complications.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles