Crohn's Disease - Symptoms, Types, Causes, Complications & Prevention
PACE Hospitals
Crohn’s disease meaning
Crohn's disease is an immunologically mediated chronic inflammatory bowel disease (autoimmune disorder) of the gastrointestinal (GI) tract that extends along the whole gut wall thickness, from the mucosa (inner layer) to the serosa (outer layer). Crohn's disease can advance from mild /moderate inflammatory conditions to severe piercing (fistulisation) or structuring illness with multiple relapses.
In Crohn's disease, the immune system targets the gut, resulting in bowel inflammation, leading to a bowel blockage, severe diarrhoea, painful bowel movements, rectal bleeding, and other severe symptoms through destruction of the intestinal tissue.
The disease has recurrent and remitting symptoms such as severe diarrhoea, weight loss, malnutrition, and abdominal pain. Nearly one-third of patients have small bowel involvement, particularly in the terminal ileum; 20% have only colon involvement, and 50% have both the colon and small bowel involved.
The Crohn’s disease cure is still under research, as there is no permanent treatment for this condition, and the majority of patients go through unexpected remission and relapse cycles. The average Crohn’s disease life expectancy will be shorter compared to those without the illness.
Juvenile Crohn’s disease
Juvenile Crohn's disease is also termed paediatric Crohn's disease, a rare form of inflammatory bowel disease characterised by chronic inflammation of the intestinal wall or any part of the GI tract. Poor linear growth and insufficient weight gain are frequently presenting problems in children. Although adults are more likely to be diagnosed with Crohn's disease, adolescents and teenagers make up about 25% of all diagnoses that just affect the small intestine.
Types of Crohn's disease
Based on the inflammation location in the gastrointestinal tract (GI), they are classified as follows:
- Ileocolitis
- Ileitis
- Gastroduodenal Crohn’s
- Jejunoileitis
- Crohn's (granulomatous) colitis
- Ileocolitis: The most typical form of Crohn's disease that causes inflammation of the colon (large intestine) and the terminal (last) part of the ileum (small intestine)
- Ileitis: Inflammation in the terminal ileum
- Gastroduodenal Crohn’s: Inflammation of the stomach and duodenum (initial part of the small intestine)
- Jejunoileitis: Inflammation of the jejunum, a middle part of the small intestine
- Crohn's (granulomatous) colitis: Inflammation of the colon
Incidence and prevalence of Crohn’s disease in India
As per 2012-2013 data, the mean annual incidence was reported as 3.91 (3.31-4.57) per 1,00,000 people, which is more than the pooled data of Southeast Asia (0.36; 0.28-0.46) and East Asia (0.34; 0.17-0.68). Read the report
The rising frequency of Crohn’s disease in India may be related to the combination of dietary, genetic and environmental factors. Overall, the incidence and prevalence of Crohn’s disease in the Asia-Pacific area are reported to be lower than those in North America or Europe. Read the report
Crohn's disease causes
Crohn's disease, a category of inflammatory bowel disease (IBD), has a complex genetic and environmental basis, but its precise cause is still idiopathic (unknown). The disease appears to be caused by an inappropriate intestine's immune system to medications, toxins, infections, or intestinal bacteria in a genetically susceptible host. However, the likelihood of having the disorder may be higher with the following risk factors:
- Autoimmune disease
- Smoking
- Genes
Over a hundred genes connected to IBD have been found with a genetic link with Crohn's disease, particularly the NOD2/CARD15 mutations. These mutations are associated with ileal (last part of the small intestine) involvement, greater severity of ileal illness necessitating surgical intervention / reoperation, and diagnosis at a younger age.
Crohn’s disease symptoms
Crohn's disease symptoms can vary in males and females from minor to severe and develop gradually. Any area of the small or large intestine may be affected by Crohn's disease (intestinal symptoms). In addition, it also manifests with extraintestinal symptoms.
Intestinal symptoms of Crohn's disease
- Difficult to pass stools
- Pain and cramps in the abdomen
- Feeling of an incomplete bowel evacuation
- Bleeding in the rectum
- Urgency is passing bowel
- Persistent diarrhoea
- Anal fistulas/Anal fissures
Extraintestinal manifestations (symptoms) of Crohn's disease
Systemic symptoms outside the GI tract caused by inflammatory bowel disease (IBD) can significantly impact a patient's health and quality of life.
- Increase in body temperature.
- Sweating during nights
- Stones in kidneys
- Osteoporosis (decrease in bone mineral density and bone mass)
- Reduction in weight
- General malaise
- Back pain
- Abnormal menstrual cycle
- Sores in mouth
- Joint pains
- Skin rashes
- Loss of hunger
- Vision problems
Crohn’s disease symptoms in females
Most females with Crohn's disease begin to exhibit symptoms before the age of 35. Women may experience certain specific symptoms, such as:
- Oligomenorrhea (Irregular periods)
- Dyspareunia (pain in genitals before/during/after intercourse)
- Deficiency in iron
- Low fertility
Crohn’s disease complications
Crohn's disease has both intestinal (local) and extraintestinal complications (systemic). The following are a few of them.
Intestinal (local) complications include
- Stricture formation (swelling and scarring of intestinal walls)
- Malabsorption and malnutrition.
- Fistulae and abscesses
Extraintestinal (systemic) complications include
- Arthritis - Ankylosing spondylitis
- Skin problems - Pyoderma gangrenosum (painful sores on the skin), Skin tags, Erythema nodosum (painful bumps under the skin)
- Eye problem (Crohn’s disease eyes) - Scleritis (inflammation of the sclera), Uveitis (inflammation of the eye), Episcleritis (inflammation of episcleral)
- Renal problem - Hydronephrosis (swollen kidneys build-up of urine), Kidney stones
- Liver and pancreatic problems - Gall stones, Fatty liver disease, Pancreatitis (inflammation of the pancreas), Hepatitis (inflammation of the liver)
- Anaemia (reduced count of red blood cells)
- Colorectal cancer
- Mouth ulcers
- Osteoporosis (reduced bone mass and mineral density)
Crohn’s disease risk factors
The following are the Crohn's disease risk factors that increase the chance of having the disease, that include:
- Age (< 30 years)
- Smoking
- Usage of anti-inflammatory medications
- Family history of Crohn’s disease
- Increased consumption of high-fat or processed foods
- Presence of bacterial infection
Crohn's Disease Prevention
Crohn’s disease cannot be prevented; however, the following might lessen flare-ups and ease symptoms:
- Quit smoking
- Daily yoga for stress management
- Avoid intake of painkillers
- Consumption of a low-fat diet
- Regular exercise
Crohn’s disease diagnosis
The gastroenterologist would like to know about the patient's medical and family history, including medications, and jot down the patient's symptoms. The gastroenterologist would perform a thorough physical examination and would like to prescribe any or in combination of the following Crohn’s disease test.
- Blood test
- Stool test
- Intestinal endoscopy
- Capsule endoscopy
- Colonoscopy
- Upper GI endoscopy
- Balloon-assisted enteroscopy
- Upper GI series
- Computerised tomography
Crohn’s disease treatment
The treatment for Crohn's disease is still under research, where medication can help control or lessen the symptoms and prevent recurrence. The major forms of treatment are medications; however, occasionally, surgery may be required.
The medications include:
- Steroids
- Immunosuppressants
- Anti-inflammatory drugs
- Biological medicines
- Liquid diet
Surgery: The gastroenterologist will suggest surgery if the benefits are more in comparison to the risks. Surgery can aid in managing symptoms and prevent them from returning. Depending on the patient's condition, a gastro-surgeon can treat Crohn’s disease by the following surgical procedures:
- Small bowel resection
- Subtotal colectomy
- Proctocolectomy and ileostomy
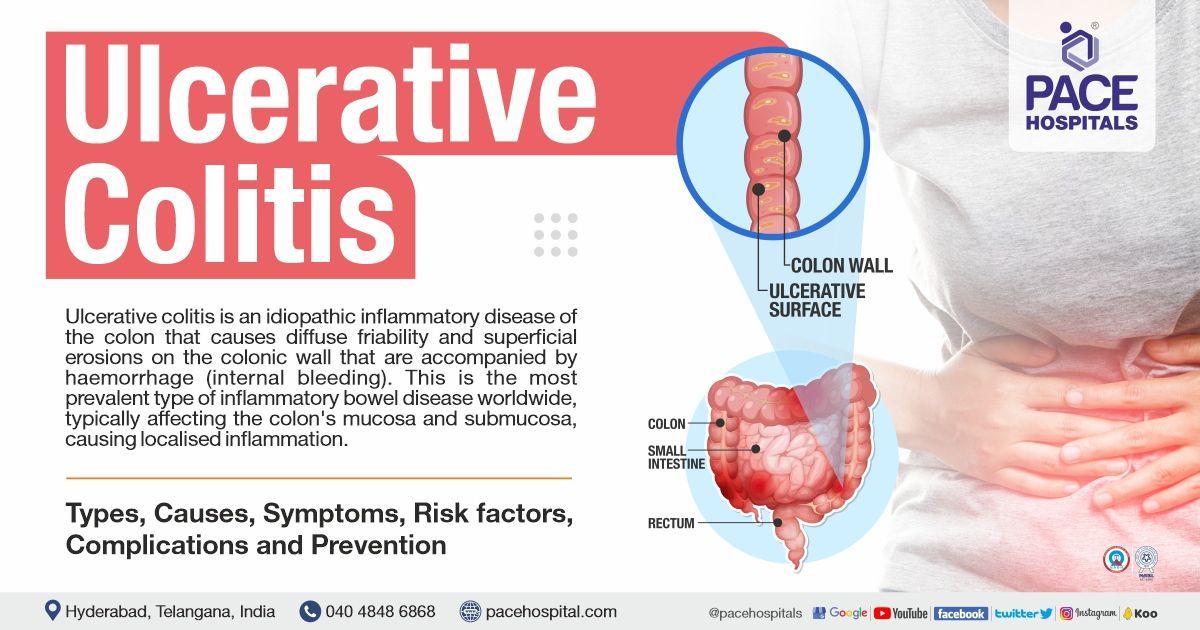
Difference between Ulcerative Colitis and Crohn's Disease
Both diseases affect the bowel in slightly different ways. Ulcerative colitis and Crohn’s disease difference are as follows:
| Elements | Ulcerative colitis | Crohn’s disease |
|---|---|---|
| Disease Location | Colon | Entire gastrointestinal tract (anywhere from the mouth to the anus) |
| Distribution | Complete and continuous inflammation of the colon | Inflammation occurs in between the healthy areas of the GI tract |
| Extent of damage | Only the innermost lining of the colon will be affected | It affects all the layers of the bowel wall (serosa to the mucosa) |
| Perianal disease, fistulae and stricture | Absent | Present |
| Prominent symptoms | Bloody diarrhoea, urgency in defecating, abdominal cramping, weight loss due to severe diarrhoea | Abdominal bloating, fissures with anal bleeding, weight loss due to severe diarrhoea |
Difference between Crohn's disease and Intestinal tuberculosis | Crohn's disease vs Intestinal tuberculosis
Crohn's disease and TB of the intestine are two chronic inflammatory diseases that can affect the gastrointestinal system. However, some significant distinctions between the two conditions are as follows:
| Elements | Crohn's disease | Intestinal tuberculosis |
|---|---|---|
| Fever Symptom | No specific pattern | Fever in evening with night sweats |
| Causes | Autoimmune diseases | Bacterial infection (Mycobacterium tuberculosis and Mycobacterium bovis) |
| Commonly affected area | Entire gastrointestinal tract; rectum, and terminal ileum | Ileocecal region, right colon, and ileum |
| Recurrence after surgery | Yes | Unlikely |
| Management | Continue immunosuppressive therapy | Short duration of therapy in compared to CD (anti-tubercular agents for 6 months) |
| Extraintestinal manifestations | More common | Less likely |
| Fistula formation | Common | Rare |
| Perianal disease | More common | Might present |
| Endoscopic findings | Skip lesions, Anorectal lesions, cobblestone appearance, longitudinal and aphthous ulcers | Circumferential ulcers, pseudopolyps, hypertrophic mucosa, and strictures |
| Clinical manifestations | Aphthous ulcers, fatigue, perianal disease, bloody stools, weight loss, and arthropathies | Fever, weight loss, abdominal pain, vomiting, loose stools, and night sweats |
Frequently Asked Questions - FAQs
Related article
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868