Pulmonary Hypertension -Types, Symptoms, Causes, Diagnosis and Treatment
PACE Hospitals
Overview | Prevalence | Types | Causes | Symptoms | Risk Factors | Complications | Diagnosis | Treatment | Prevention | Primary vs Secondary Pulmonary Hypertension | FAQs | When to consult a Doctor
Pulmonary hypertension definition
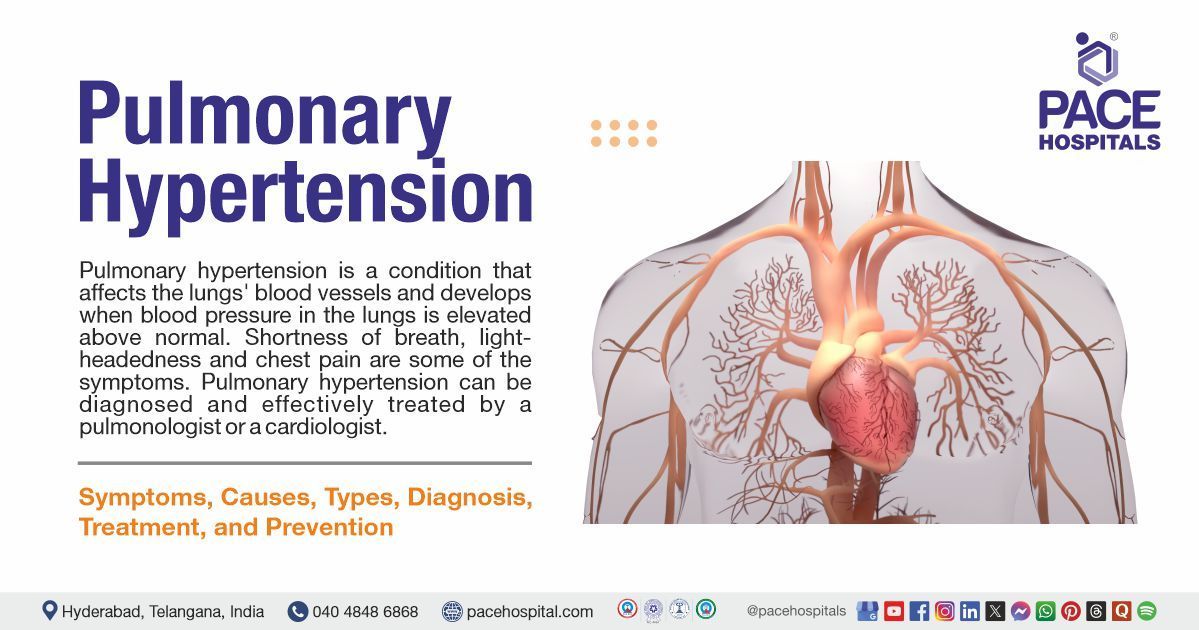
Pulmonary hypertension is a condition that affects the lungs' blood vessels and develops when blood pressure in the lungs is elevated above normal. The heart must, therefore, use more effort to pump blood into the lungs. Shortness of breath, lightheadedness and chest pain are some of the symptoms that might result from this increased cardiac strain.
It's a serious illness that can damage the heart's right side. It is more difficult for the pulmonary arteries to expand and allow blood to pass through when their walls thicken and stiffen. Due to this decreased blood flow, the right side of the heart finds it more challenging to pump blood through the arteries.
Pulmonary hypertension can be diagnosed and effectively treated by a pulmonologist (a specialist in the lungs) or a cardiologist (a specialist in the heart and blood vessels).
Pulmonary hypertension meaning
The term “pulmonary hypertension” is derived from two components: “pulmonary”, from the Latin word "pulmonarius", meaning “of the lungs”, and “hypertension”, which combines the Greek prefix hyper (meaning excessive) and the Latin word "tensio" (meaning pressure). Together, the term refers to abnormally high blood pressure in the arteries of the lungs.
Prevalence of Pulmonary Hypertension
Prevalence of pulmonary hypertension in the world
According to estimates, pulmonary hypertension affects roughly 1% of people worldwide (including all WHO groups), and in people over 65, the prevalence can reach 10%. The global age-standardized prevalence of pulmonary arterial hypertension (PAH), a distinct and less common subgroup, is roughly 2.28 cases per 100,000 population, with an estimated 192,000 affected globally in 2021.
The most prevalent form of pulmonary hypertension in the US is brought on by left-sided heart conditions, such as left heart failure. Several additional medical conditions and environmental variables can increase the risk of getting pulmonary hypertension.
Prevalence of pulmonary hypertension in India
In India, the estimated prevalence of pulmonary arterial hypertension (PAH) is 0.15 per lakh population, of which 0.06 per lakh are idiopathic cases.
According to hospital-based research conducted in India, individuals with underlying conditions such as congenital heart disease, coronary artery disease, rheumatic heart disease, and chronic obstructive pulmonary disease (COPD) have a high burden of PH.
In a study of 100 patients undergoing conservative management, hemodialysis (HD), or continuous ambulatory peritoneal dialysis (CAPD), the overall prevalence of pulmonary hypertension (PH) was found to be 41%. The highest prevalence was observed in the HD group, where 53% of patients had pulmonary hypertension (PH).
Types of Pulmonary Hypertension
Pulmonary hypertension classification mainly includes 5 groups based on underlying causes. Below are the different types of pulmonary hypertension:
- Group 1: Pulmonary arterial hypertension (PAH)
- Group 2: Pulmonary hypertension because of left-sided heart disease
- Group 3: Hypoxia / Pulmonary hypertension due to lung disease
- Group 4: Chronic thromboembolic pulmonary hypertension (CTEPH)
- Group 5: Pulmonary hypertension with unknown/multiple causes
Group 1: Pulmonary arterial hypertension (PAH)
This type 1 pulmonary hypertension develops when the lungs' arteries constrict, thicken, or harden. This makes it harder for the right side of the heart to pump blood through the lungs, putting extra strain on the heart. Over time, this can weaken the heart and reduce its ability to pump enough blood to meet the body’s needs.
There are different types of PAH. Idiopathic PAH occurs without a known cause, while heritable PAH (HPAH) is associated with genetic factors passed down through families. Other medical conditions like HIV, liver disease, congenital heart disease, and connective tissue disorders like lupus or scleroderma can also be associated with pulmonary arterial hypertension (PAH). It may also be linked to drug use, including the central nervous system (CNS) stimulants and certain diet pills. Although treatments are available to help manage pulmonary arterial hypertension (PAH), there is currently no cure.
Group 2: Pulmonary hypertension because of left-sided heart disease
Despite the arteries and lungs in this PH group not being as thick or rigid as those in pulmonary arterial hypertension (PAH), there are issues with the left side of the heart's valves or the way the heart contracts and relaxes. This results in a backup in the blood, which increases lung pressure because the left ventricle cannot keep up with the blood returning from the lungs. The most prevalent type of PH is pulmonary hypertension of left-side heart disease.
Group 3: Hypoxia / Pulmonary hypertension due to lung disease
These lung diseases include sleep apnea, restrictive lung disease, where the lungs struggle to expand when inhaled (e.g., interstitial lung disease or pulmonary fibrosis), obstructive lung disease, where the lung airways narrow and make it difficult to exhale (e.g., COPD or emphysema), and prolonged exposure to high altitude. Lung arteries constrict, allowing blood to flow entirely to the parts of the lungs that are getting the most oxygen and air.
Group 4: Chronic thromboembolic pulmonary hypertension (CTEPH)
When the body lacks the ability to break up a blood clot in the lungs, CTEPH may result. This can result in scar tissue in the lungs' blood arteries, which prevents regular blood flow and increases the workload for the heart's right side. Because the blood clots can be removed with pulmonary thromboendarterectomy (PTE) surgery, However, this operation is not appropriate for all patients with CTEPH. For patients with CTEPH, medication is also available if a physician determines that the patient is not suitable for PTE surgery or if PH persists after the procedure.
Group 5: Pulmonary hypertension with unknown or multiple causes
This involves the mechanisms by which PH develops secondary to other diseases, which are unclear. Among these related illnesses include sarcoidosis, sickle cell anaemia, chronic hemolytic anaemia, splenectomy (removal of the spleen), and specific metabolic problems.
Pulmonary Hypertension Causes
The exact cause of pulmonary hypertension (PH) is not known, but it can develop due to certain medical conditions that damage, block, or affect the blood vessels in the lungs. This leads to high blood pressure in the pulmonary arteries.
Some of the medical conditions that cause pulmonary hypertension include:
- Left-sided heart disease: The most common causes of pulmonary hypertension are issues with the left side of the heart, including left ventricular dysfunction, mitral or aortic valve disease, and left heart failure. As the right side of the heart needs to work hard to pump blood through the lungs, these conditions raise the pressure in the pulmonary arteries.
- Lung diseases and low oxygen levels: Pulmonary hypertension may result from chronic lung conditions such as chronic obstructive pulmonary disease (COPD), interstitial lung disease (like pulmonary fibrosis), and conditions that cause low oxygen levels (hypoxia), such as sleep apnea or continuous exposure to high altitude. These conditions raise blood pressure in the lungs and narrow the pulmonary arteries.
- Blood clots in the lungs: Previous blood clots (pulmonary emboli) or scarring in the lung arteries cause chronic thromboembolic pulmonary hypertension (CTEPH), which narrows or blocks the vessels, thereby raising blood pressure.
- Pulmonary arterial changes and other medical conditions: Pulmonary hypertension can result from changes to the small branches of the pulmonary arteries, which are frequently caused by congenital heart defects, HIV infection, portal hypertension, connective tissue diseases (such as scleroderma), or certain medications. Some cases are inherited (heritable) or occur with no known cause (idiopathic).
- Other rare causes: Inflammatory conditions like sarcoidosis, blood disorders like sickle cell disease, metabolic disorders like thyroid disease, chronic kidney disease (CKD), tumors, and persistent neonatal pulmonary hypertension are less frequent causes.
Pulmonary Hypertension Symptoms
Signs and symptoms of pulmonary hypertension may persist for years before a diagnosis is made. This is because pulmonary hypertension frequently presents symptoms that are also indicative of other illnesses. The following are the symptoms of pulmonary hypertension:
Symptoms of pulmonary hypertension in adults
- Coughing that is dry or produces blood
- Chest pain
- Hoarseness
- Weaknesses
- Nausea and vomiting
- Wheezing
- Swelling of the abdomen, legs, or feet
- Shortness of breath
- Dizziness that may lead to fainting
- Cyanosis (A bluish colour to the lips and skin)
- Fatigue
Pulmonary arterial hypertension symptoms
Early signs of pulmonary hypertension, absent or very mild, making the condition difficult to detect. As the disease progresses, individuals often begin to experience symptoms that are common to other lung conditions. The most common symptoms of PAH include
- Increased shortness of breath, especially with activities like walking up the stairs or exercise
- Edema, or swelling of the legs, feet and eventually the abdomen and neck
- Fatigue
- Chest pain
- Heart palpitations (Racing or pounding)
Pulmonary hypertension symptoms in babies
Persistent pulmonary hypertension of the newborn symptoms arises when a baby’s circulation doesn’t adapt properly after birth. It is a condition where high blood pressure in the lungs leads to low oxygen levels because blood flows abnormally from the right to the left side of the heart through the foramen Ovale and ductus arteriosus, bypassing the lungs.
- Asphyxia (deprived of oxygen)
- Respiratory acidosis
- Tachypnea, respiratory distress
- Low Apgar scores (a baby may need immediate medical attention to help them adjust)
- Loud, single-second heart sound (S2) or a harsh systolic murmur (secondary to tricuspid regurgitation)
- Cyanosis: Poor cardiac function and perfusion
- Meconium staining (refers to the presence of meconium (the first stool of a baby) in the amniotic fluid before or during birth)
- Systemic hypotension
- Symptoms of shock
Chronic thromboembolic pulmonary hypertension symptoms
- Chronic thromboembolic pulmonary hypertension (CTEPH) can cause symptoms like shortness of breath, chest pain, dizziness, fainting, and tiredness.
- These symptoms may be mild at first but can worsen over time if left untreated. The most common signs are trouble breathing during physical activity and reduced ability to exercise.
- Less common symptoms include coughing, coughing up blood, unusual chest pain, and a fast or irregular heartbeat.
Pulmonary Hypertension Risk Factors
Identifying the risk factors for pulmonary hypertension is essential for early diagnosis and prevention. Individuals with one or more of these risk factors need to monitor their health closely and consult a doctor if they experience symptoms like unexplained shortness of breath, fatigue, or chest pain. These risk factors include:
- Age: Pulmonary hypertension (PH) can occur at any age, but is most often diagnosed between 30 and 60. Ageing increases the risk due to changes in the heart and blood vessels.
- Environmental exposure: Long-term exposure to harmful substances like asbestos or infections from parasites can damage lung vessels, increasing pulmonary hypertension (PH) risk.
- Family history & genetics: Genetic conditions such as Down syndrome, congenital heart disease, Gaucher disease, and a family history of blood clots can raise pulmonary hypertension (PH) risk.
- Lifestyle habits: Smoking and illegal drug use can damage the heart and lungs, leading to inflammation and higher pressure in the lungs.
- Medications: Certain cancer and depression medications may affect lung blood vessels and increase the risk of pulmonary hypertension.
- Sex: Women are more likely than men to develop pulmonary hypertension (PH), particularly related to heart failure or idiopathic forms, possibly due to hormones or autoimmune diseases.
Pulmonary Hypertension Complications
Pulmonary hypertension can lead to several serious complications that affect both the heart and other organs. These include:
- Right heart failure: Right ventricular hypertrophy, dilation, and failure—the primary cause of death in pulmonary hypertension—are caused by prolonged pressure overload.
- Pulmonary artery complications: Angina or myocardial infarction may result from massive pulmonary artery dilatation that compresses nearby structures, such as the left main coronary artery (left main compression syndrome). Although uncommon, pulmonary artery dissection or rupture frequently results in death.
- In situ thrombosis and thromboembolism: A higher chance of blood clots developing in the pulmonary arteries, which can exacerbate pulmonary hypertension and cause more issues.
- Hemoptysis (Coughing up blood): Ruptures of the delicate pulmonary or bronchial arteries can cause severe bleeding, which can occasionally result in life-threatening respiratory compromise.
- Respiratory failure: Acute or chronic respiratory failure may arise from a progressive deterioration of gas exchange and hypoxemia, particularly in advanced disease.
- Pericardial effusion and tamponade: Heart tamponade, a medical emergency, can develop from fluid buildup around the heart, which can affect cardiac function.
- Sudden cardiac death: It can result from arrhythmias, severe right heart failure, or severe circumstances like pulmonary artery rupture or dissection.
These complications demonstrate the extensive effects of pulmonary hypertension on both the heart and other body systems. To improve long-term health outcomes, maintain quality of life, and improve patient care, early detection and effective management are crucial.
Pulmonary Hypertension Diagnosis
Pulmonary hypertension is difficult to diagnose because the symptoms of pulmonary hypertension (PH) are like those of other heart or lung conditions. Below are the steps involved in the diagnosis of pulmonary hypertension:
- Clinical history of patients
- Physical examination
- Initial noninvasive tests
- Blood tests (to rule out other causes)
- Electrocardiogram (ECG OR EKG)
- Chest X-ray
- Key screening test
- Transthoracic echocardiography
- Additional diagnostic tests
- Lung function tests
- Sleep study
- Exercise tests
- Advanced imaging
- Computed Tomography (CT) scan
- Cardiovascular Magnetic Resonance (CMR)
- Ventilation/perfusion (V/Q) scan
- Confirmatory test
- Right heart catheterization
- Specialized tests (if indicated)
- Genetic testing
- Lung biopsy
Pulmonary Hypertension Treatment
While pulmonary hypertension cannot be cured, treatment can help alleviate symptoms and improve management of the condition. The following are the treatment options for pulmonary hypertension:
Non-pharmacological treatment of PH
- Dietary changes
- Lifestyle changes
- Oxygen therapy
Pharmacological treatment of PH
- Targeted therapies: Endothelin receptor antagonists, phosphodiesterase type-5 inhibitors, prostacyclin analogues and receptor agonists and soluble guanylate cyclase stimulators
- Calcium channel blockers
- Diuretics
- Anticoagulants
Surgical management of PH
- Pulmonary endarterectomy
- Balloon angioplasty
- Balloon atrial septostomy
- Lung transplantation
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
Prevention of Pulmonary Hypertension
The preventive aspects of pulmonary hypertension can significantly lower the risk of developing pulmonary hypertension, even if not all cases can be avoided, particularly in people who already have heart or lung conditions. Below are some of the preventive measures for pulmonary hypertension:
- Addressing modifiable risk factors: Early detection and treatment of underlying lung and heart conditions, such as sleep disorders, chronic lung disease, and left heart disease. People need to avoid being around toxins and substances that are known to cause pulmonary hypertension, such as illegal drugs and some appetite suppressants.
- Lifestyle modifications: People need to quit smoking and stay away from secondhand smoke. Maintaining a healthy weight and practising regular physical activity appropriate for their health status.
- Infection prevention: To lower the risk of respiratory diseases that can worsen PH, people need to get the recommended vaccinations, particularly those for influenza and pneumococcal infections.
- Early detection and screening: Getting regular health checkups for individuals with risk factors or symptoms suggestive of PH. Screening for sleep apnea and other conditions that can cause pulmonary hypertension (PH).
- Managing comorbid conditions: Ensuring proper diagnosis and treatment of conditions like
obstructive sleep apnea (OSA), chronic obstructive pulmonary disease (COPD) and connective tissue diseases (CTDs).
Difference Between Primary and Secondary Pulmonary Hypertension
Primary vs Secondary Pulmonary Hypertension
Understanding the difference between primary (idiopathic) and secondary pulmonary hypertension is essential for an accurate diagnosis and successful treatment. The table below indicates some of the parameters that help in differentiating primary and secondary pulmonary hypertension:
| Parameters | Primary pulmonary hypertension | Secondary pulmonary hypertension |
|---|---|---|
| Definition | Elevated pulmonary artery pressure that has no known cause (known as IPAH, or idiopathic pulmonary arterial hypertension) | Elevated pulmonary artery pressure caused by a known underlying illness (such as thromboembolic, lung, or heart disease) |
| Causes | It is unknown, and it may be genetic or idiopathic | It is caused by left heart disease, chronic thromboembolism, lung disease, or other systemic conditions. |
| Symptoms | Chest pain, fatigue, syncope, progressive dyspnea, palpitations | Dyspnea plus symptoms/signs of the underlying disease (like orthopnea in heart failure and cough in lung disease) |
| Diagnosis | Right heart catheterization confirms the diagnosis. | Using imaging, laboratory testing, and echocardiography to determine the underlying cause |
| Treatment | Prostacyclin analogues, endothelin receptor antagonists, and PDE5 inhibitors are examples of targeted PAH treatments. | To treat the underlying illness (e.g., oxygen for lung disease, anticoagulation for thromboembolism, and diuretics for heart failure). |
Frequently Asked Questions (FAQs) on Pulmonary Hypertension (PH)
How serious is pulmonary hypertension?
Pulmonary hypertension is a serious condition characterised by high blood pressure in the arteries of the lungs. It can lead to issues including blood clots and heart failure, and in extreme situations, it can even be fatal. While most people cannot find a permanent cure, the disease can be slowed down, and symptoms may be effectively treated with proper care.
Is pulmonary hypertension fatal?
Idiopathic pulmonary artery hypertension (IPAH), another name for pulmonary hypertension, is a progressive condition that affects the precapillary pulmonary vasculature with no clearly identified underlying risk factor. During rest, the pulmonary artery pressure consistently exceeds 25 mmHg, and during exercise, it exceeds 30 mmHg. It is a rare but deadly illness with a high death rate. Untreated, it could lead to rising back pressure, right heart failure, and even death.
Can stress increase pulmonary hypertension?
Yes, in patients with severe pulmonary hypertension, even mild mental stress may worsen the right heart strain. This is brought on by the sympathetic nervous system being activated, which constricts the pulmonary blood vessels, raising the pulmonary artery pressure and pulmonary vascular resistance. This increases cardiac stress because the right side of the heart must work harder to pump blood through the lungs.
How does oxygen therapy help with pulmonary hypertension?
When pulmonary hypertension is caused by underlying lung diseases, such as COPD, oxygen therapy is especially important. It helps by raising blood oxygen levels, alleviating symptoms including fatigueand dyspnoea, and may enhancing the general quality of life. It can be an essential supportive treatment for pulmonary hypertension, even though it is not a cure.
How does hypoxiacause pulmonary hypertension?
Hypoxia plays an important role in the development of pulmonary hypertension. Short-term (acute) hypoxia causes the pulmonary arteries to constrict, leading to an increase in pulmonary artery pressure. Long-term (chronic) hypoxia leads to changes in the structure of the pulmonary blood vessels, including thickening of the vessel walls and growth of smooth muscle into smaller arteries.
Can pulmonary edema cause pulmonary hypertension?
Yes, Pulmonary edema increases fluid accumulation in the lungs, raising the pressure in the pulmonary capillaries and leading to elevated pulmonary artery pressure. This persistent pressure overload can contribute to vascular remodeling and the progression of pulmonary hypertension, especially in conditions like left heart failure.
How does portal hypertension cause pulmonary hypertension?
Portopulmonary hypertension (PPH) is a type of pulmonary hypertension that can result from
portal hypertension, a condition marked by increased blood pressure in the portal vein, which drains blood from the spleen and digestive tract. This can lead to pulmonary vasoconstriction and structural alterations in the pulmonary arteries when elevated portal pressure allows blood to avoid the liver's filtration and enter the lungs unfiltered.
How to treat pulmonary hypertension?
In addition to treating the underlying cause of pulmonary hypertension (PH), treatment includes some pulmonary hypertension medications, procedures, and lifestyle changes that enhance the patient's quality of life. Typically, management employs a combination of strategies.
Does heart failure cause pulmonary hypertension?
Yes, heart failure, particularly left-sided heart failure, is a well-recognized cause of pulmonary hypertension, classified as Group 2 pulmonary hypertension. In this condition, increased pressure on the left side of the heart leads to a backup of blood into the pulmonary circulation, raising pressure in the pulmonary arteries. Over time, this elevated pressure can cause structural changes in the pulmonary vessels, worsening the hypertension and contributing to further strain on the heart.
Can I live a normal life with pulmonary hypertension?
Yes, early identification and timely medical intervention are essential to manage symptoms and prevent complications. Although there is currently no cure for PH, a combination of medications, lifestyle changes, and occasionally surgery can significantly reduce symptoms, slow the progression of the condition, and improve overall quality of life. Maintaining stability and well-beingrequires regular follow-up with medical professionals and adherence to the treatment plan.
How long can you live with pulmonary hypertension?
The type, severity, and management of pulmonary hypertension all affect life expectancy. It is a progressive and potentially fatal condition. While there is no cure for most forms, advances in therapy, especially for pulmonary arterial hypertension (PAH), have significantly improved outcomes. Without treatment, idiopathic PAH may have a mean survival of 2–3 years, but with proper management, many patients can live 7–10 years or more.
Can mild pulmonary hypertension be reversed?
Although pulmonary hypertension cannot be cured, symptoms and underlying causes may be managed, which may lower or even restore lung blood pressure to normal. Depending on the type and underlying reason, this can occasionally lead to the reversal of moderate cases.
Can a CT scan detect pulmonary hypertension?
Yes, a CT scan, especially a CT pulmonary angiogram (CTPA), can be very helpful in diagnosing and evaluating pulmonary hypertension. It can show possible causes of the condition and help doctors understand how serious it is.
What is the difference between pulmonary hypertension and pulmonary arterial hypertension?
Increased blood pressure in the lungs' arteries due to any cause, such as heart, lung, or blood vessel illnesses, is referred to as pulmonary hypertension (PH). Classified as WHO Group 1 pulmonary hypertension, pulmonary arterial hypertension (PAH) is a distinct and uncommon subtype of pulmonary hypertension (PH) caused by the constriction or blockage of the small pulmonary arteries, which raises resistance and pressure. Consequently, not all PH is PAH, but all PAH is PH.
When to consult a doctor for pulmonary hypertension?
Consult a doctor for pulmonary hypertension when symptoms like shortness of breath (SOB), chest pain, or fatigue do not go away over time or begin to make daily activities difficult.
Other warning signs may include:
- Swelling in the ankles, legs, or abdomen
- Bluish lips or skin (cyanosis)
- Dizziness, fainting spells, or a rapid heartbeat
- A feeling of chest tightness or pressure
When these problems become persistent or worsen, a pulmonary hypertension specialist can carry out the right tests and recommend proper treatment. In urgent situations, such as sudden breathing difficulties, severe chest pain, or fainting, emergency care is needed without delay. Depending on the condition, a cardiologist or pulmonologist may suggest the most effective pulmonary hypertension treatment to relieve symptoms, improve heart and lung function, and lower the risk of complications.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles