Obstructive Sleep Apnea - Symptoms, Causes, Risk factors, Diagnosis and Treatment
PACE Hospitals
Obstructive sleep apnea (OSA) is a sleep disorder characterised by repeated episodes of partial or complete obstruction of the upper airways during sleep, associated with decreased oxygen saturation leading to a cessation of breathing (defined as a period of apnea or hypopnea more than 10 seconds), followed by agitation (a state of nervousness or anxiety) and hyperpnea (increased depth and rate of breathing).
OSA that is related to excessive daytime sleepiness is commonly known as obstructive sleep apnea syndrome, also called obstructive sleep apnea-hypopnea syndrome.
Primary care physicians (general physician) assess symptoms and may refer patients to specialists, such as pulmonologists, otolaryngologists (ENT specialist), or sleep specialists, depending on the patient's respiratory system health and sleep disorders.
Obstructive sleep apnea meaning
- Obstructive: Is derived from Latin word “obstructus” which means to block, build up, stop or something that causes blockage or obstruction.
- Sleep: Is derived from the word "slaep," which is related to sleeping or resting.
- Apnea: It is a Greek word which means "without breath."
Obstructive sleep apnea means an obstruction (blockage) of the airway during sleep that results in interruptions or pauses in breathing.
Obstructive sleep apnea prevalence
The global prevalence of obstructive sleep apnea, is approximately 12.5% worldwide. Of these, almost 93.6% of adults aged 30-69 have mild to severe OSA. Among these, 45.4% of adults have moderate to severe OSA, which is based on a diagnostic measure called apnea-hypopnea index (AHI), indicating five or more events per hour.
Prevalence of obstructive sleep apnea in an Indian population
A meta-analysis found that about 1040 lakh Indians of the working age group are suffering from OSA, with 470 lakhs having moderate-to-severe OSA. The overall prevalence of OSA is 11%, with 13% in males and 5% in females. OSA is more common in males than in females.
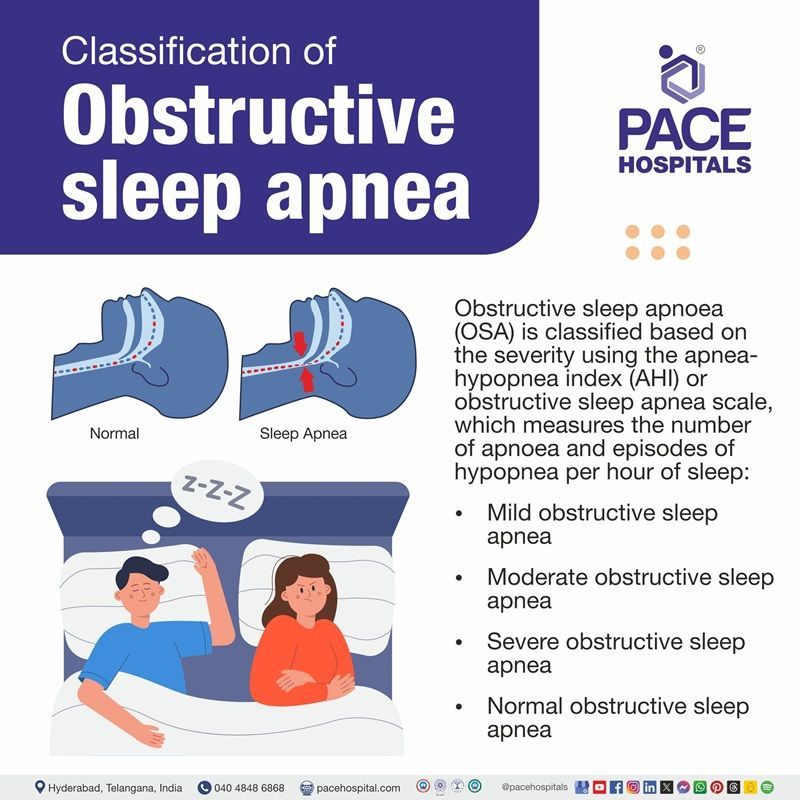
Obstructive sleep apnea classification
Obstructive sleep apnea (OSA) is classified based on the severity using the apnea-hypopnea index (AHI) or obstructive sleep apnea scale, which measures the number of apnea and episodes of hypopnea per hour of sleep:
- Mild obstructive sleep apnea: AHI is between 5 and 14.9 events per hour
- Moderate obstructive sleep apnea: AHI is between 15 and 29.9 events per hour
- Severe obstructive sleep apnea: AHI is greater than or equal to 30 events per hour
- Normal obstructive sleep apnea: AHI is less than five events per hour
Obstructive sleep apnea symptoms
The signs and symptoms of obstructive sleep apnea might vary from person to person and can happen both during sleep as well as in the daytime as mentioned below:
Obstructive sleep apnea OSA symptoms during sleep
- Loud snoring that disrupts others' sleep
- Gasping or choking sounds
- Observed pauses in breathing
- Sudden or jerky body movements
- Restless tossing and turning
- Frequent awakenings
Day time symptoms of obstructive sleep apnea
- Feeling unrested despite sleeping for many hours
- Morning headaches
- Dry or sore throat
- Daytime sleepiness or fatigue
- Personality changes (e.g., mood swings, irritability)
- Difficulty concentrating or remembering things
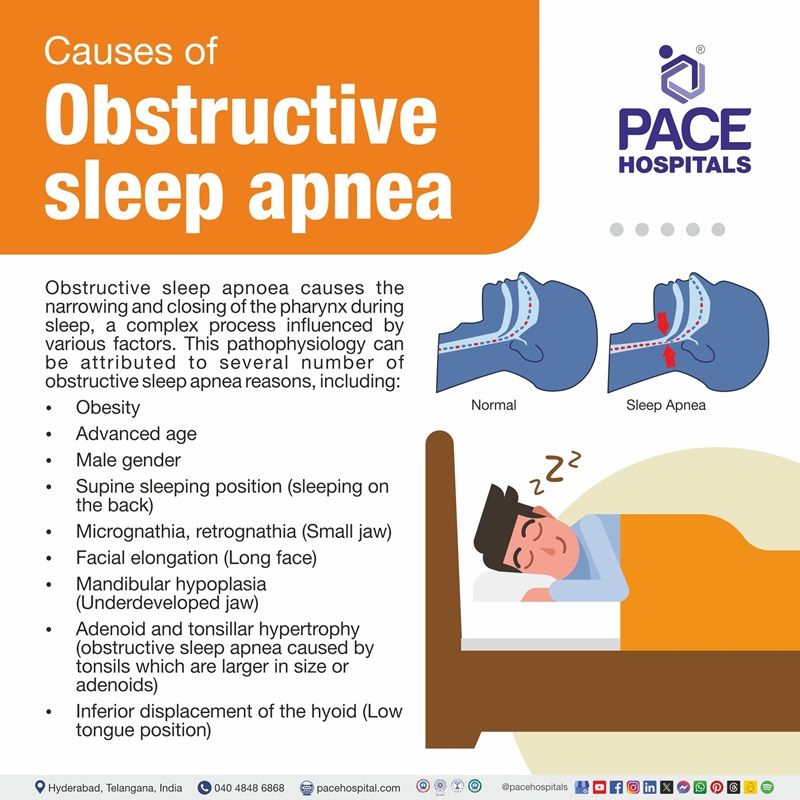
Obstructive sleep apnea causes
Obstructive sleep apnea causes the narrowing and closing of the pharynx during sleep, a complex process influenced by various factors. This pathophysiology can be attributed to several obstructive sleep apnea reasons, including:
Structural Factors or anatomical factors
- Micrognathia, retrognathia (Small jaw)
- Facial elongation (Long face)
- Mandibular hypoplasia (Underdeveloped jaw)
- Adenoid and tonsillar hypertrophy (obstructive sleep apnea caused by tonsils which are larger in size or adenoids)
- Inferior displacement of the hyoid (Low tongue position)
Non-structural factors or nonanatomic Factors
- Central fat distribution (accumulation of fat in the abdominal area)
- Obesity
- Advanced age
- Male gender
- Supine sleeping position (sleeping on the back)
- Pregnancy
Additional Factors
- Alcohol use
- Smoking
- Use of sedatives and hypnotics
Medical disorders that can cause OSA include
- Nocturnal gastroesophageal reflux (Stomach acid flowing back into the throat)
- Acromegaly (the body produces excess amount of growth hormone)
- Hypothyroidism (underactive thyroid)
- Prior stroke (a stroke that occurred in the past)
- Obesity hypoventilation syndrome (it is a condition where obesity and sleep apnea coexist)
Obstructive sleep apnea risk factors
Identifying and addressing these multiple risk factors linked to obstructive sleep apnea helps in the diagnosis and management. The following are the obstructive sleep apnea risk factors in adults:
- Obesity (weight gain): Obesity can worsen OSA due to fat deposition at particular places, such as the craniofacial area and the upper airway. Apnea appears to be caused by fat buildup in the tissues surrounding the upper airway, which causes a narrower lumen and increased collapsibility of the upper airway.
- Inheritance: It is unknown how obstructive sleep apnea is inherited. Generally, siblings or children (first-degree relatives) of affected individuals have a 50% higher chance of having this condition compared to the general population.
- Smoking: Exposure to smoke leads to inflammation in the airways, which may cause the upper airways to narrow and collapse. This increases the risk of obstructive apnea, while nicotine stimulation and sudden withdrawal of nicotine disturb the quality of sleep.
- Menopause: The relevant age for OSA is menopause due to fluctuations in hormones and changes in the female physiological system. After menopause, OSA becomes more common in post-menopausal women because individuals who go through menopause often gain weight, which raises their BMI and makes harder for them to breathe at night.
- Alcohol use before sleep at night time: Alcohol relaxes muscles, particularly those in the throat, which increases the likelihood of airway collapse while sleeping. This inactivity plays a role in the beginning of OSA or its severity.
- Nasal obstruction: Nasal obstruction can trigger sleep-disordered breathing problems like apnea, hypopnea, and snoring due to pathologic changes in the speed or velocity and resistance of airflow.
Obstructive sleep apnea complications
Obstructive sleep apnea complications can lead to abnormal physiology and serious consequences if left undiagnosed and untreated. These complications may include:
- Hypertension: Obstructive sleep apnea causes hypertension due to the sudden and repeated drop of oxygen levels in blood during sleep causing the body to raise blood pressure and heart rate. OSA can also cause sleep deprivation, which causes endothelial dysfunction (impaired functioning of the blood vessel lining) and arterial stiffness (reduced elasticity of arteries), both of which can contribute to hypertension.
- Pulmonary hypertension: Obstructive sleep apnea causes pulmonary hypertension, a complication that can lead to high blood pressure in the lungs through intermittent hypoxia (reduced oxygen levels availability). This is because, during OSA episodes, the obstruction can decrease oxygen levels and increase carbon dioxide levels in the blood, leading to pulmonary vasoconstriction. This extra pressure can damage the blood vessels in the lungs.
- Diabetes: Obstructive sleep apnea causes diabetes, which is mainly associated with type 2 diabetes during sleep apnea episodes. The low level of oxygen and buildup of carbon dioxide can disrupt glucose metabolism. This can lead to resistance to insulin, which means the body cells become less reactive to insulin.
- Heart failure: Obstructive sleep apnea leads to left ventricular diastolic dysfunction, a condition where the heart fails to fill with blood during diastole, which increases the risk of heart failure.
- Cardiac arrhythmia: Obstructive sleep apnea leads to cardiac arrhythmia, mostly nocturnal arrhythmias due to intermittent hypoxia (reduced oxygen levels availability), and fluctuations in the oxygen during sleep cause disturbance in the heart electric system in obstructive sleep apnea patients.
- Myocardial infarction: The repetitive hypoxia and reoxygenation (a cycle of low oxygen levels and quickly returns to normal levels) in obstructive sleep apnea leads to oxidative stress and causes inflammation, which increases the risk of myocardial infarction.
- Depression: Individuals with sleep apnea may develop depression due to repeated breath disturbances because of hypoxia (low oxygen levels). This increases daytime sleepiness and negative moods; these factors develop depression symptoms.
- Stroke: Obstructive sleep apnea causes stroke by a sudden reduction in oxygen levels in the blood, leads to high blood pressure, which causes stress to the heart, and leads to hypertension and some heart-related problems such as irregular heartbeat and atrial fibrillation.
Obstructive sleep apnea diagnosis
Obstructive sleep apnea diagnosis often involves overnight monitoring of breathing and other body functions during sleep testing. Here are the obstructive sleep apnea diagnosis steps:
- Medical history
- Physical examination
- Sleep studies
- Obstructive sleep apnea polysomnography
- Home sleep apnea testing for obstructive sleep apnea in adults
Medical history: The general physician gathers a medical history by asking about symptoms or risk factors, while housemates provide risk assessment information.
Physical examination: The physical examination of obstructive sleep apnea involves measuring body weight, height, and neck circumference. Blood pressure is also measured, as well as mouth-throat assessment, nasal polyps, and rhinitis.
Sleep studies: Obstructive sleep apnea sleep studies include
- Polysomnography
- Home sleep testing
- Obstructive sleep apnea polysomnography: This test is also called as obstructive sleep apnea gold standard diagnosis test. It helps in diagnose OSA by classifying sleep stages and apneic (Breathless) and hypopneic (reduced breathing) periods. However, it requires overnight stays in a sleep laboratory, making it complex and costly. Polysomnography typically includes:
- EEG (electroencephalography): Used to measure sleep activity in brain
- Chin electromyography: It is used to detect hypotonia (muscle weakness in the upper airway)
- Electro-oculography: It assesses the rapid eye movements
- Airflow sensors: It is used at mouth and nose to detect apneas and hypopneas
- Chest or abdominal sensors: It is used to detect respiratory efforts
- Pulse oximetry: It is used to measure oxygen saturation levels during sleep
- ECG: It is used to detect arrhythmias related to apneic episodes
- Home sleep apnea testing for obstructive sleep apnea in adults: Home sleep testing using moveable diagnostic tools detects apnea and severity using heart rate, pulse oximetry, respiratory effort, position, and nasal airflow. The role of home sleep apnea is expanded due to its convenience, cost-effectiveness, and accurate estimation of respiratory disturbances.
Obstructive sleep apnea treatment
Obstructive sleep apnea treatment is provided to patients based on symptoms such as fatigue, sleeplessness, snoring, gasping, and choking with an AHI value of 15 or higher. The following are the different treatment modalities for obstructive sleep apnea that include:
- Lifestyle changes or control of risk factors
- Positional Therapy
- Continuous positive airway pressure (CPAP)
- Oral appliances
- Surgery
- Medicine for obstructive sleep apnea
Obstructive sleep apnea lifestyle changes or control risk factors:
The initial treatment for obstructive sleep apnea (OSA) aims to manage risk factors including obesity, hypertension, alcohol, and sedative use, while also exploring obstructive sleep apnea treatment at home. Good sleep hygiene, such as sleeping longer, discontinuing sedative medications, and weight loss, can reduce daytime sleepiness and its severity.
The impact of bariatric surgery on obstructive sleep apnea can reduce AHI and symptoms, while GLP-1 receptor antagonists have been increasingly used for weight loss and lower the OSA severity.
Positional therapies for obstructive sleep apnea:
It aims to prevent supine positions and promote obstructive sleep apnea sleeping positions known as side sleeping or non-supine positions by using devices such as binders, backpacks, pillows, tennis balls, and positional sensors. It is specially used in spine related obstructive sleep apnea.
Continuous positive airway pressure (CPAP) (Positive airway pressure therapy for obstructive sleep apnea)
It is considered the best treatment for obstructive sleep apnea in some patients with daytime sleepiness that impairs cognitive function. This CPAP treatment reduces sleepiness and snoring and repeatedly improves the bed partner sleep.
Obstructive sleep apnea oral appliance therapy:
For patients who are unable or unwilling to use CPAP or have difficulty accessing electricity reliably, the mandibular advancement appliances for obstructive sleep apnea are the most common oral appliances that can bring the lower jaw forward and relieve the obstruction of airways. These appliances are considered effective for both mild to moderate obstructive sleep apnea treatment and snoring.
Obstructive sleep apnea surgical treatment:
The following are some of the obstructive sleep apnea surgery options:
- Uvulopalatopharyngoplasty (UPPP): Removes any excess tissue from the back of the throat that improves airflow and reduce apnea.
- Maxillomandibular advancement for treatment of obstructive sleep apnea: Fix problems with the facial structures.
- Tracheostomy: It is recommended for patients who are most seriously affected (such as those with cor pulmonale) and cannot tolerate CPAP since it avoids the location of obstruction. This is only used as a last resort.
- Tonsillectomy and adenoidectomy: Removes the tonsils and adenoids.
- Hypoglossal nerve stimulator (HNS): Places an appliance that mimics as pacemaker to stimulate the throat muscles to remain open during sleep.
Drug therapy for obstructive sleep apnea
Obstructive sleep apnea medication therapy is generally not recommended as part of the first-line treatment. The following are some of the obstructive sleep apnea medications:
- Wakefulness-promoting agents: These are FDA-approved drugs for obstructive sleep apnea use in individuals who have residual daytime sleepiness despite adequate usage of CPAP
- Dopamine norepinephrine reuptake inhibitor (DNRI): Is suggested to improve wakefulness in individuals with OSA who experience excessive daytime sleepiness.
Prevention of obstructive sleep apnea
It is possible to avoid obstructive sleep apnea by adopting healthy lifestyle modifications such as:
- Maintaining a healthy weight
- Maintaining a diet low in fat (heart-healthy diet)
- Stopping smoking
- Reducing the amount of alcohol and caffeine intake
- Getting adequate sleep
Difference between Central sleep apnea and Obstructive sleep apnea
Central sleep apnea vs obstructive sleep apnea
Both central and obstructive sleep apnea’s cause breathing to stop and start repeatedly during sleep; they differ in their causes and symptoms, including:
| Elements | Central sleep apnea | Obstructive sleep apnea |
|---|---|---|
| Definition | Central sleep apnea can lead when the brain temporarily ceases transmitting signals to the muscles responsible for breathing. | Obstructive sleep apnea (OSA) is a condition where the airway is narrowed or blocked, causing breathing pauses during sleep. |
| Causes | It can be caused by brainstem issues, certain medications, and high altitude, including brain infections, strokes, cervical spine conditions, and certain medications. | Causes of OSA includes anatomical factors such as small jaw, long face, and other factors like obesity, age, alcohol, smoking, hypothyroidism etc |
| Symptoms | It is characterized by disrupted breathing during sleep, chronic fatigue, daytime sleepiness, morning headaches, and restless sleep. | Symptoms include loud snoring that disrupts others' sleep, gasping or choking sounds, observed pauses in breathing, sudden or jerky body movements |
| Prevalence | It is less common than obstructive sleep apnea but is not rare. | This is a common medical condition that is becoming more prevalent as obesity rates grow. |
Frequently Asked Questions (FAQs) on Obstructive sleep apnea
What are the complications of obstructive sleep apnea in adults?
The complications of obstructive sleep apnea in adults include hypertension, pulmonary hypertension, diabetes, heart failure, cardiac arrhythmia, depression, stroke, and myocardial infarction.
How to cure obstructive sleep apnea?
Obstructive sleep apnea is not curable; research indicates that some lifestyle choices may improve or reduce the severity of the condition. The disease can also manage by additional therapies or surgeries.
Is obstructive sleep apnea dangerous?
Yes, obstructive sleep apnea is dangerous because, if left untreated, it leads to severe complications such as accidents, daytime sleep, heart problems, high blood pressure, and depression, and it may be life-threatening and lead to sudden cardiac death.
What are the symptoms of obstructive sleep apnea syndrome?
Intermittent hypoxemia (a periodic drop in oxygen levels in the blood), oxidative stress, sleep fragmentation or disturbed sleep, and excessive daytime sleepiness are the symptoms obstructive sleep apnea syndrome.
Does obstructive sleep apnea causes weight gain?
Yes, obstructive sleep apnea can cause weight gain because sleep deprivation can lead to a craving for high-calorie foods. The body produces less leptin and increases ghrelin levels, which makes a person feel hungry.
What are the cardiovascular complications of obstructive sleep apnea?
The cardiovascular complications of obstructive sleep apnea are hypertension, coronary artery disease, heart failure, and cardiac arrhythmias.
What is obstructive sleep apnea syndrome definition?
Obstructive sleep apnea syndrome, also known as obstructive sleep apnea-hypopnea syndrome, is a sleep disorder characterized by excessive daytime sleepiness.
Can obstructive sleep apnea cause central sleep apnea?
Yes, in some cases, obstructive sleep apnea can lead to central sleep apnea, also called Treatment-emergent central sleep apnea (TECSA). It happens while treating with continued airway.
How to treat obstructive sleep apnea?
The treatment of obstructive sleep apnea is based on healthy lifestyle changes, such as weight loss, quitting alcohol, and healthy sleep through positive airway pressure machine called obstructive sleep apnea machines, oral appliances, surgical implants, position therapy, and surgical procedures.
Which doctor to consult for obstructive sleep apnea?
Primary care physicians (General medicine doctor) evaluate patients' symptoms and, if necessary, refer them to a specialist such as pulmonologist (a lung specialist) who focuses on respiratory system health and manage other breathing disorders related to OSA, otolaryngologists (ear, nose, and throat doctors). In some cases, a sleep specialist may be the best choice to focus on sleep disorders.
Does obstructive sleep apnea increase hematocrit?
The meta-analysis found that patients with OSA, particularly severe ones, showed slight increases in hematocrit values, but this was uncertain and not clinically significant.
Does untreated obstructive sleep apnea cause secondary erythrocytosis?
Erythrocytosis is uncommon in patients with suspected or confirmed OSA and is linked to both awake and nocturnal hypoxemia, but not to OSA presence or its severity.
What is the best treatment for obstructive sleep apnea?
The best treatment method for obstructive sleep apnea is using a breathing device, such as a continuous positive airway pressure machine. A (CPAP) machine continuously provides air pressure. It keeps the upper airways open and facilitates breathing during sleep.
Is obstructive sleep apnea a disability?
SSA (Social Security Administration) does not recognize obstructive sleep apnea as a disability but considers it only in severe cases when symptoms that qualify for benefits, such as heart disease, breathing disorders, or mental issues, may be regarded as a disability and significantly impact daily activities for over a year or more.
List out few obstructive sleep apnea symptoms in children?
Snoring, restless sleep, nighttime sweating, apnea, and nocturnal enuresis(bedwetting) are observed.
Daytime signs and symptoms include nasal blockage, mouth breathing, morning headaches, difficulty concentrating, and hyperactivity (a symptom of sleepiness). Children with obstructive sleep apnea experience less sleepiness during the day than adults.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868