Ulcerative Colitis Treatment in Hyderabad, India
Widely regarded as the best hospital for ulcerative colitis treatment in Hyderabad, PACE Hospitals offers expert, patient-focused care. Our expert team of gastroenterologists provides individualized care for patients living with ulcerative colitis—an inflammatory bowel disease (IBD) that affects the inner lining of the colon and rectum. We use advanced diagnostic tools such as colonoscopy with biopsy, stool and blood tests, and imaging studies to assess the severity of the condition and ensure accurate diagnosis.
Book Appointment for Ulcerative Colitis Treatment
Ulcerative Colitis Treatment Online Appointment
Thank you for contacting us. We will get back to you as soon as possible. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Oops, there was an error sending your message. Please try again later. Kindly save these contact details in your contacts to receive calls and messages:-
Appointment Desk: 04048486868
WhatsApp: 8977889778
Regards,
PACE Hospitals
HITEC City and Madeenaguda
Hyderabad, Telangana, India.
Why Choose PACE Hospitals for Ulcerative Colitis Treatment?

Complete Ulcerative Colitis Diagnosis & Treatment with Advance Technology
Dedicated IBD Specialist Gastroenterologist in Hyderabad
Minimally Invasive Colectomy & J-Pouch Surgery with Endoscopic Management of UC Complications
Affordable & Transparent Ulcerative Colitis Treatment with Insurance & Cashless Options
Ulcerative Colitis Diagnosis
Diagnosing ulcerative colitis (UC) is a comprehensive process that requires careful evaluation by gastroenterologists. Because ulcerative colitis can present symptoms similar to other inflammatory bowel diseases (IBD) and gastrointestinal conditions, gastroenterologists use a systematic approach to confirm the diagnosis. The goal is to determine whether inflammation is present in the colon, assess the extent and severity of the disease, and rule out other possible causes of similar symptoms.
The diagnostic evaluation includes the following:
- Risk assessment – To identify individuals with conditions, genetic factors, or environmental exposures that increase their likelihood of developing inflammatory bowel disease.
- Medical history – To understand symptom patterns, family history, previous treatments, and factors that may have triggered the condition.
- Physical examination – To evaluate signs of inflammation, complications, or extraintestinal manifestations that may suggest ulcerative colitis.
- Diagnostic tests – To confirm intestinal inflammation, assess disease extent and severity, and exclude other conditions with similar presentations.
- Staging and classification – To determine disease location, severity, and activity level, which guides treatment decisions and helps predict disease course.
Risk Assessment
Ulcerative colitis (UC) risk involves a mix of factors. Age distribution shows peaks in the second-third and sixth-seventh decades. Family history is significant, with first-degree relatives having a higher likelihood. Genetic factors contribute substantially to the risk. Environmental factors include smoking cessation, processed food consumption, antibiotic use, and NSAID exposure. Geographic patterns show higher prevalence in developed countries and urban areas, supporting the hygiene hypothesis, suggesting reduced early-life microbial exposure contributes to immune dysfunction. These factors collectively shape an individual's susceptibility to developing ulcerative colitis.
Medical History
Ulcerative colitis generally presents with bloody diarrhea, abdominal cramping (especially in the left lower quadrant), urgency, and tenesmus (A constant, urgent urge to empty the bowels or bladder despite being empty).
Symptoms follow a chronic remitting pattern. Constitutional symptoms like fatigue, weight loss, and fever suggest severe disease. Extraintestinal manifestations include joint pain, skin lesions, and eye inflammation. The family history of inflammatory bowel disease (IBD) or autoimmune diseases is crucial. Recent antibiotic use, NSAID exposure, or infectious triggers should be explored. The impact on daily functioning, work, and social activities helps assess severity and treatment urgency.
Physical Examination
Physical examination assesses disease severity and complications. Vital signs may reveal fever, tachycardia, or hypotension indicating active inflammation or complications. Abdominal examination focuses on left lower quadrant tenderness, distension (suggesting toxic megacolon), and bowel sounds.
Digital rectal examinations may reveal blood, mucus, or tenderness. Signs of anemia include pallor of conjunctiva and nail beds. Extraintestinal manifestations affect 25-30% of patients, including arthritis, skin lesions (erythema nodosum, pyoderma gangrenosum), eye inflammation, and hepatomegaly (enlargement of liver). Malnutrition signs and growth retardation in children should be assessed.
Diagnostic Tests
Diagnostic tests are essential for confirming ulcerative colitis (UC), assessing its extent and severity, and ruling out other conditions with similar symptoms. These tests encompass a range of evaluations, including laboratory tests to identify inflammation and assess overall health, endoscopic evaluations for direct visualization and tissue sampling, and imaging studies to evaluate the colon and identify complications.
Laboratory Tests
Ulcerative colitis lab tests play a crucial part in the diagnosing and managing ulcerative colitis. These tests help to identify inflammation, assess disease severity, rule out other conditions, and monitor complications. The following laboratory tests are commonly performed in patients with suspected or confirmed ulcerative colitis:
- Complete blood count (CBC)
- Inflammatory markers (ESR, CRP)
- Comprehensive metabolic panel (CMP)
- Iron studies (ferritin, TIBC, transferrin saturation)
- Vitamin levels (B12, folate, vitamin D)
- Liver function tests (LFTs)
- Infectious screening (Tuberculosis, Hepatitis B/C, CMV)
- Stool studies (Bacterial/Parasitic)
- Fecal calprotectin
- Serologic markers (pANCA, ASCA)
Complete Blood Count (CBC): This test measures red blood cells, white blood cells, and platelets. It is indicated to evaluate for anemia (common in ulcerative colitis due to chronic blood loss) and signs of inflammation or infection (elevated white blood cell count).
Inflammatory Markers (ESR, CRP): Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are indicators of inflammation in the body. Elevated levels suggest active inflammation in the colon, helping to confirm the presence and severity of ulcerative colitis.
Comprehensive Metabolic Panel (CMP): This panel measures electrolytes, kidney function, and liver function. It is indicated to assess electrolyte imbalances (common due to diarrhea) and to evaluate kidney and liver function, which can be affected by ulcerative colitis or its treatments.
Iron Studies (Ferritin, TIBC, Transferrin Saturation): These tests evaluate iron levels in the body. They are indicated to assess iron deficiency anemia, which is common in ulcerative colitis due to chronic blood loss and impaired iron absorption.
Vitamin Levels (B12, Folate, vitamin D): These tests measure vitamin levels in the blood. They are indicated to assess vitamin deficiencies, which can occur due to malabsorption or dietary restrictions in ulcerative colitis patients.
Liver Function Tests (LFTs): These tests measure liver enzymes and bilirubin levels. They are indicated to evaluate liver inflammation or damage, which can occur in ulcerative colitis patients, particularly those with primary sclerosing cholangitis (PSC).
Infectious Screening (Tuberculosis, Hepatitis B/C): These tests screen for infections that can be reactivated or worsened by immunosuppressive medications used to treat ulcerative colitis. They are indicated before starting biologically or other immunosuppressive therapies.
Stool Studies (Bacterial/Parasitic): These tests analyze stool samples for the presence of bacteria, parasites, or toxins. They are indicated to rule out infectious causes of colitis, such as Salmonella, Shigella, Campylobacter, or Clostridium difficile.
Fecal Calprotectin: This test assesses the amount of calprotectin, a protein produced by white blood cells in the colon (intestines). Elevated levels indicate intestinal inflammation, helping to differentiate ulcerative colitis from non-inflammatory conditions like irritable bowel syndrome (IBS).
Serologic Markers (pANCA, ASCA): Perinuclear anti-neutrophil cytoplasmic antibodies (pANCA) and Anti-Saccharomyces cerevisiae antibodies (ASCA) are antibodies that can help differentiate between ulcerative colitis and Crohn's disease. pANCA is more commonly associated with ulcerative colitis, while ASCA is more commonly associated with Crohn's disease.
Endoscopic Evaluation
Ulcerative colitis colonoscopy with biopsy is the gold standard diagnostic test to diagnose the disease. Ulcerative colitis shows continuous inflammation beginning in the rectum and extending proximally. Endoscopic findings include mucosal erythema, loss of vascular pattern, friability, ulceration, and pseudo polyps.
The disease can affect just the rectum (proctitis), the left side of the colon (left-sided colitis), or the entire colon (pancolitis). Ulcerative colitis endoscopy usually shows continuous inflammation in the colon lining. Tissue samples often reveal long-term inflammation, damage to the colon lining, and small collections of pus. Capsule endoscopy can be used to check the small intestine and help tell it apart from Crohn's disease.
Imaging Studies
Cross-sectional imaging (CT/MRI) assesses disease extent and complications. Computed tomography (CT) or magnetic resonance (MR) enterography evaluates small bowel involvement to differentiate ulcerative colitis from Crohn's disease. In acute presentations, ulcerative colitis CT scan rules out toxic megacolon (abnormal dilation of large intestine), perforation, or abscess formation.
Plain abdominal radiographs monitor severe colitis for colonic dilatation. Imaging helps assess disease distribution, wall thickening, and extraintestinal manifestations. Fecal elastase testing may be performed to evaluate pancreatic function in selected cases.
Staging and Classification
Disease extent includes proctitis (rectum only), left-sided colitis (rectum to splenic flexure), and pancolitis (entire colon). Disease severity uses Truelove and Witts criteria: mild disease has <4 stools daily with minimal blood, while severe disease involves ≥6 bloody stools daily with systemic toxicity including fever, tachycardia, anemia, and elevated ESR.
Ulcerative Colitis Differential Diagnosis
Figuring out whether someone has ulcerative colitis can be challenging because many other conditions can look very similar in terms of symptoms, test results, and tissue samples. The most important condition to tell apart from ulcerative colitis is Crohn’s disease, which is another type of inflammatory bowel disease. Unlike ulcerative colitis, Crohn’s disease can affect patches of the bowel, go deeper into the bowel wall, often cause problems around the anus, and may show certain signs under the microscope.
Gastroenterologists also need to rule out infections caused by bacteria (like Clostridioides difficile, Salmonella, or Shigella), viruses, or parasites (such as those that cause amebiasis or schistosomiasis). This is usually done by checking stool samples and considering the patient's symptoms.
Other conditions to consider include:
- Microscopic colitis, which causes long-lasting watery diarrhea and needs a tissue sample to diagnose.
- Ischemic colitis, more common in older adults, causes sudden belly pain and bleeding due to reduced blood flow.
- Radiation colitis, found in people who have had radiation treatment to the pelvic area.
- Drug-related colitis, caused by medications like painkillers, antibiotics, or chemotherapy drugs.
- Intestinal tuberculosis, mostly in places where tuberculosis is common, can look like inflammatory bowel disease but usually affects a specific area of the bowel and is confirmed by lab or tissue tests.
- Colorectal cancer, which can have similar symptoms and must be ruled out through scope and biopsy.
- Acute self-limiting colitis, a short-term bowel inflammation usually due to a passing infection or unknown cause.
To make a clear diagnosis, gastroenterologists rely on a mix of symptoms, lab tests, imaging, endoscopy, and tissue analysis. No single test can confirm it alone. Newer tools like advanced lab tests and special imaging are being used more often, especially since about 10 percent of people with inflammatory bowel disease cannot be clearly diagnosed with either ulcerative colitis or Crohn’s disease.
Keeping a Close Watch: Regular Check-Ups to Prevent Cancer in Ulcerative Colitis
People who have had ulcerative colitis for many years are more likely to develop colon cancer. That is why regular check-ups, especially colonoscopies, are an important part of their care. These tests allow gastroenterologists to look for early signs of cancer or changes in the colon that could become serious later. How often someone needs these check-ups depends on how long they have had ulcerative colitis and their personal risk factors.
By keeping up with these visits, people can catch problems early and feel more in control of their health. It is a team effort between the patient and the healthcare provider, based on trust and regular care.
These check-ups are also a good time for people to talk about any new symptoms, ask questions, and get tips on staying healthy. This ongoing support helps people feel more confident and less alone in managing their condition. In the end, regular check-ups are not just about preventing cancer—they help people with ulcerative colitis live better and healthier lives.
The treatment of ulcerative colitis aims to induce and maintain remission, prevent complications, and improve quality of life. Since ulcerative colitis is a chronic condition with no cure, the goal is to control inflammation, heal the intestinal mucosa, and prevent disease progression and complications.
Treatment strategies are individualized based on disease extent, severity, location, and patient factors. The approach generally includes:
- Ulcerative colitis medications
- Lifestyle modifications and dietary management
- Nutritional support and supplementation
- Management of complications
- Monitoring and follow-up care
- Surgical intervention when necessary
- Emergency management protocols
- Psychosocial support and patient education
Ulcerative colitis medications
Anti-inflammatory Agents (Aminosalicylates): Anti-inflammatory agents are first-line therapy for mild to moderate ulcerative colitis and maintenance of remission. These medications reduce intestinal mucosal inflammation through multiple mechanisms including inflammatory mediator inhibition and antioxidant effects. Oral formulations deliver active ingredients to different colon parts, while topical formulations (enemas/suppositories) are effective for distal disease. Proctitis responds well to suppositories, left-sided colitis to enemas, and extensive colitis requires oral therapy. Combination oral and topical therapy is more effective than either alone for inducing remission in extensive disease.
Corticosteroids: Corticosteroids treat moderate to severe ulcerative colitis flares but aren't suitable for long-term maintenance due to significant side effects. Oral corticosteroids are used for moderate to severe disease, while intravenous forms are necessary for hospitalized patients with severe colitis. Topical corticosteroids (enemas/foam) effectively treat distal disease with fewer systemic effects.
Newer formulations with high first-pass metabolism have reduced systemic effects. The goal is rapid corticosteroid tapering while maintaining remission with other medications. If a patient needs to take steroids often or can't stop taking them without their condition getting worse, they may need stronger medications that help calm down the immune system.
Immunosuppressive Agents: Antimetabolites (a class of immunosuppressive medications) help keep the disease under control in patients who rely on steroids or don't respond well to them. These drugs need careful monitoring because they can affect the bone marrow, harm the liver, and increase the risk of infections. Testing certain enzymes before starting the medication helps find patients who might have serious side effects. Other immune-suppressing drugs are used less often in ulcerative colitis than in Crohn's disease, but they might be an option for patients who can't tolerate antimetabolites. Calcineurin inhibitors are used as a backup treatment for severe ulcerative colitis that doesn't respond to steroids, to avoid emergency surgery to remove the colon. Regular check-ups are important to make sure the treatment is safe, works well, and to avoid problems.
Biologic Therapies: Biologic drugs for ulcerative colitis (a type of advanced treatment that targets specific parts of the immune system) have transformed how ulcerative colitis is treated, especially in moderate to severe cases. These targeted treatments block certain inflammation pathways that cause the disease. Anti-tumor necrosis factor agents work well to start and keep the disease under control, but patients need to be monitored for infections, cancer risks, and possible reactions to infusions. Integrin antagonists block certain immune cells from reaching the gut, offering good safety and fewer whole-body immune effects. Interleukin inhibitors are another option for patients who don't respond to anti-TNF therapy. Newer drugs like JAK inhibitors are also being added to the list of treatments for ulcerative colitis.
Symptomatic and Supportive Medications: Antispasmodics (medications that reduce muscle spasms) help relieve cramping and belly pain during ulcerative colitis flares. Anti-diarrheal drugs can be used carefully to ease symptoms but are avoided in severe flares because they can enhance the risk of a serious condition called toxic megacolon. Topical anesthetics (numbing creams or ointments) can ease pain and discomfort around the anus. Antibiotics are used in certain cases, such as treating pouchitis (inflammation of the ileal pouch), infections, or as extra support in severe colitis. These supportive treatments work alongside the main anti-inflammatory drugs to improve comfort and help patients feel better while managing the disease.
Lifestyle Modifications and Dietary Management
While diet doesn't cause ulcerative colitis, certain modifications help manage symptoms and support overall health. Patients should maintain balanced, nutritious diets while identifying personal trigger foods. During active flares, low-residue diets reduce symptoms by decreasing stool frequency and abdominal pain, limiting high-fiber foods, raw fruits/vegetables, nuts, and seeds.
During remission, high-fiber diets benefit overall colon health. Adequate hydration is crucial, especially during flares with increased fluid losses. Probiotics may help maintain remission though evidence is mixed. Stress management through meditation, yoga, or counseling helps prevent flares. Regular exercise improves health and reduces stress.
Nutritional Support and Supplementation
Nutritional deficiencies are common in people with ulcerative colitis because of poor absorption, limited diets, and long-term inflammation. Vitamin B12 and folate supplements help correct deficiencies caused by damage to the end of the small intestine or side effects from medications. Iron supplements, either taken by mouth or through a vein, are used to treat anemia from ongoing blood loss.
Vitamin D supplements are helpful because people with inflammatory bowel disease (IBD) often have low levels of this vitamin. Zinc and magnesium may also need to be replaced in patients with widespread disease or poor absorption. Liquid nutrition through a feeding tube (enteral nutrition) can help, especially in children, while nutrition through a vein (parenteral nutrition) is used only in cases of severe malnutrition.
Management of Complications
Ulcerative colitis complications require specific management approaches. Anemia from chronic blood loss needs iron supplementation (oral or intravenous based on severity/tolerance). A blood transfusion may be required for severe anaemia or acute bleeding. Bone health is important, particularly in corticosteroid-receiving patients, requiring calcium/vitamin D supplementation and bone density monitoring. Bone-strengthening medications may be necessary for osteoporosis. Colorectal cancer surveillance is crucial for long-standing ulcerative colitis patients, especially with pancolitis, beginning 8-10 years post-diagnosis with regular colonoscopic intervals. Extraintestinal manifestations may need specific treatments: arthritis, eye complications requiring ophthalmologic evaluation, and primary sclerosing cholangitis needing hepatologic management.
Monitoring and Follow-up
Regular monitoring assesses disease activity, treatment response, and potential complications through clinical assessment, laboratory monitoring, and endoscopic evaluation. Patients on immunosuppressive or biologic therapies require regular monitoring for side effects including complete blood counts, liver function tests, and infection/malignancy screening. Disease activity monitoring uses clinical symptoms, laboratory markers (CRP, fecal calprotectin), and endoscopic assessment when indicated. The goal is achieving and maintaining clinical and endoscopic remission. Monitoring frequency depends on disease severity, treatment type, and patient response to therapy.
Surgical Treatment (ulcerative colitis surgery)
Surgical management of ulcerative colitis is necessary for medically refractory disease, complications, or malignancy. Total proctocolectomy is the standard ulcerative colitis surgical procedure, performed with either permanent ileostomy or ileal pouch-anal anastomosis (IPAA). IPAA (J-pouch surgery) allows continence maintenance and avoids permanent stoma but requires multiple stages with potential complications including pouchitis requiring ongoing medical management. Emergency surgery may be necessary for complications like toxic megacolon, perforation, or severe bleeding unresponsive to medical therapy. Surgical timing and approach depend on disease severity, patient factors, and response to medical management.
Specialized Procedures: Endoscopic procedures may be necessary for specific complications. Stricture dilation can be performed endoscopically for benign strictures, though malignancy must be excluded. Pouch endoscopy and management are important for patients who have undergone ileal pouch-anal anastomosis, particularly for diagnosing and treating pouchitis. Chromoendoscopy or narrow-band imaging enhances dysplasia detection during surveillance colonoscopy. These specialized procedures require expertise and should be performed at centers experienced in IBD management. Regular surveillance and appropriate intervention can prevent complications and improve long-term outcomes.
Emergency Management
Severe ulcerative colitis complications require immediate intervention. Toxic megacolon necessitates bowel rest, intravenous corticosteroids, broad-spectrum antibiotics, and surgical consultation. Fluid resuscitation protocols address dehydration and electrolyte imbalances from severe diarrhea. Blood transfusion criteria guide management of severe anemia or active bleeding. Intensive care management may be required for patients with systemic toxicity, hemodynamic instability, or multi-organ involvement. Emergency surgery may be necessary for perforation, uncontrolled bleeding, or failed medical management. Early identification and prompt treatment of complications are crucial for preventing morbidity and mortality.
Patient Education and Psychosocial Support
Patient education is crucial for successful long-term management. Patients should understand their condition, treatment options, potential side effects, and when to seek medical attention. Support groups and educational resources help patients cope with their chronic condition. The psychological impact shouldn't be underestimated, as many patients experience anxiety, depression, or social isolation related to symptoms. Mental health support, counseling, and peer support groups are important comprehensive care components. Education empowers patients to actively participate in their care, improving adherence and outcomes.
Treatment Timeline by Disease Severity
Mild Disease (Proctitis or Left-sided Colitis): Topical anti-inflammatory agents as first-line therapy, oral anti-inflammatory agents if topical therapy is insufficient, short courses of topical corticosteroids if needed, maintenance therapy with anti-inflammatory agents, symptomatic support with antispasmodics as needed.
Moderate Disease: Combination oral and topical anti-inflammatory agents, oral corticosteroids for flares, consider immunosuppressive agents for steroid-dependent patients, biologic therapy for refractory cases, nutritional assessment and supplementation, regular monitoring for complications.
Severe Disease: Hospitalization may be required, intravenous corticosteroids, rescue therapy with calcineurin inhibitors or biologic agents, surgical consultation for refractory cases, intensive monitoring for complications, fluid resuscitation and nutritional support, emergency management protocols if needed.
Maintenance Therapy: Anti-inflammatory agents for mild disease, immunosuppressive agents or biologics for moderate to severe disease, regular monitoring and dose optimization, lifestyle modifications and dietary counseling, cancer surveillance for long-standing disease, management of extraintestinal manifestations.
The management of ulcerative colitis requires a multidisciplinary approach involving gastroenterologists, nurses, dietitians, surgeons, and other specialists as needed. With appropriate treatment, most patients can achieve good symptom control and maintain a good quality of life. The key to successful management is early diagnosis, appropriate treatment selection based on disease characteristics, regular monitoring, strong patient-provider communication, and comprehensive care addressing both intestinal and extraintestinal manifestations of the disease.
Difference Between Ulcerative Colitis and Crohn’s Disease
Ulcerative Colitis vs Crohn’s Disease
Ulcerative colitis and Crohn’s disease are the two main forms of inflammatory bowel disease (IBD). Although they share some symptoms, they differ in location, pattern of inflammation, complications, and treatment approach. Understanding these differences helps in accurate diagnosis and long-term management as follows:
| Feature | Ulcerative Colitis | Crohn’s Disease |
|---|---|---|
| Area affected | Limited to the colon and rectum | Can affect any part of the digestive tract, from mouth to anus |
| Pattern of disease | Continuous inflammation starting from the rectum | Patchy inflammation with normal areas in between (“skip lesions”) |
| Depth of inflammation | Affects only the inner lining of the bowel | Involves all layers of the bowel wall |
| Common symptoms | Bloody diarrhea, urgency, rectal bleeding | Abdominal pain, diarrhea, weight loss, fatigue |
| Complications | Severe bleeding, colon dilation, increased colon cancer risk | Fistulas, strictures, abscesses, bowel obstruction |
| Surgery outcome | Removing the colon can be curative | Surgery helps symptoms, but disease can recur |
| Smoking effect | Smoking may worsen disease after quitting | Smoking often worsens disease activity |
Ulcerative Colitis Treatment Cost in Hyderabad, India
The cost of Ulcerative Colitis (UC) Treatment in Hyderabad generally ranges from ₹1,000 to ₹18,500 (approx. US $12 – US $225).
The exact ulcerative colitis treatment cost varies depending on the severity of inflammation, need for colonoscopy, medication type (5-ASA, steroids, immunomodulators, biologics), diagnostic tests, gastroenterologist expertise, and hospital facilities — including cashless treatment options, TPA corporate tie-ups, and assistance with medical insurance wherever applicable.
Cost Breakdown According to Type of Ulcerative Colitis Treatment
- Gastroenterology Consultation – ₹600 – ₹900 (US $7 – US $11)
- Basic Blood Tests (CBC, CRP, ESR) – ₹400 – ₹1,200 (US $5 – US $14)
- Stool Calprotectin Test (Inflammation Marker) – ₹1,200 – ₹3,000 (US $14 – US $36)
- Ulcerative Colitis Medications (1 Month – 5-ASA, Steroids) – ₹800 – ₹3,500 (US $9 – US $42)
- Immunomodulators / Biologics (If Severe) – ₹8,000 – ₹18,500 (US $97 – US $225)
Frequently Asked Questions (FAQs) on Ulcerative Colitis
What is the best treatment for ulcerative colitis?
The best treatment for ulcerative colitis depends on disease severity. For mild-to-moderate cases, aminosalicylates are the first line. For moderate-to-severe disease or if first-line therapy fails, corticosteroids, immunomodulators, biologics, or Janus kinase (JAK) inhibitors may be used. The choice of drug class is based on patient response, side effect profile, and disease extent.
Which Is the best hospital for Ulcerative Colitis Treatment in Hyderabad, India?
PACE Hospitals, Hyderabad, is one of the leading centres for inflammatory bowel disease (IBD) care, offering comprehensive Ulcerative Colitis diagnosis and treatment with advanced therapeutic options.
We have team of expert gastroenterologists and IBD specialists use endoscopic evaluation, personalised medication plans, nutritional guidance, and modern monitoring strategies to control flare-ups, maintain remission, and improve long-term gut health.
We provide best services with high-definition endoscopy suites, advanced diagnostic labs, experienced clinical teams, and specialised IBD care pathways, PACE Hospitals ensures safe, accurate, and patient-focused UC management — supported by cashless insurance options, TPA tie-ups, and complete medical documentation assistance.
What is the latest treatment for ulcerative colitis?
The latest treatments for ulcerative colitis include advanced biologic agents and Janus kinase (JAK) inhibitors. These newer drug classes target specific immune pathways to control inflammation and are used for moderate-to-severe cases, especially when conventional therapies have failed. Sphingosine 1-phosphate (S1P) receptor modulators are also emerging as a novel option.
Is there a permanent cure for ulcerative colitis?
There is no permanent medical cure for ulcerative colitis. Most patients require ongoing therapy to manage symptoms and maintain remission. Surgical removal of the colon (colectomy) can be curative for the disease, but this is generally reserved for severe or refractory cases and comes with significant lifestyle changes.
Can quitting smoking cause ulcerative colitis?
Peer-reviewed studies indicate that quitting smoking is associated with an increased risk of developing ulcerative colitis. Nicotine appears to have a protective effect against ulcerative colitis, though the mechanism is not fully understood. However, the health risks of smoking far outweigh any potential benefits, so smoking is not recommended.
What Is the cost of Ulcerative Colitis Treatment at PACE Hospitals, Hyderabad?
At PACE Hospitals, Hyderabad, the cost of ulcerative colitis treatment typically ranges from ₹900 to ₹16,500 and above (approx. US $11 – US $200), making it an affordable and reliable option for comprehensive IBD care. However, the final cost depends on:
- Severity of UC (mild, moderate, severe)
- Need for colonoscopy or sigmoidoscopy
- Stool and blood inflammatory markers
- Type of medication (5-ASA, steroids, biologics)
- Need for hospitalization during flare-ups
- Nutritional supplements and follow-up visits
- Additional tests (fecal calprotectin, CT/MRI abdomen)
For mild UC requiring basic medications, costs remain on the lower end; moderate-to-severe UC requiring biologics or prolonged therapy falls toward the higher range.
After a detailed gastroenterology evaluation, imaging/endoscopy review, and treatment planning, our specialists will provide a personalised UC management plan and transparent cost estimate tailored to your condition.
Can ulcerative colitis cause cancer?
Chronic ulcerative colitis increases the risk of colorectal cancer, especially in patients with extensive or long-standing disease. The risk is related to the duration and severity of inflammation. Regular colonoscopic surveillance is recommended to detect precancerous changes early.
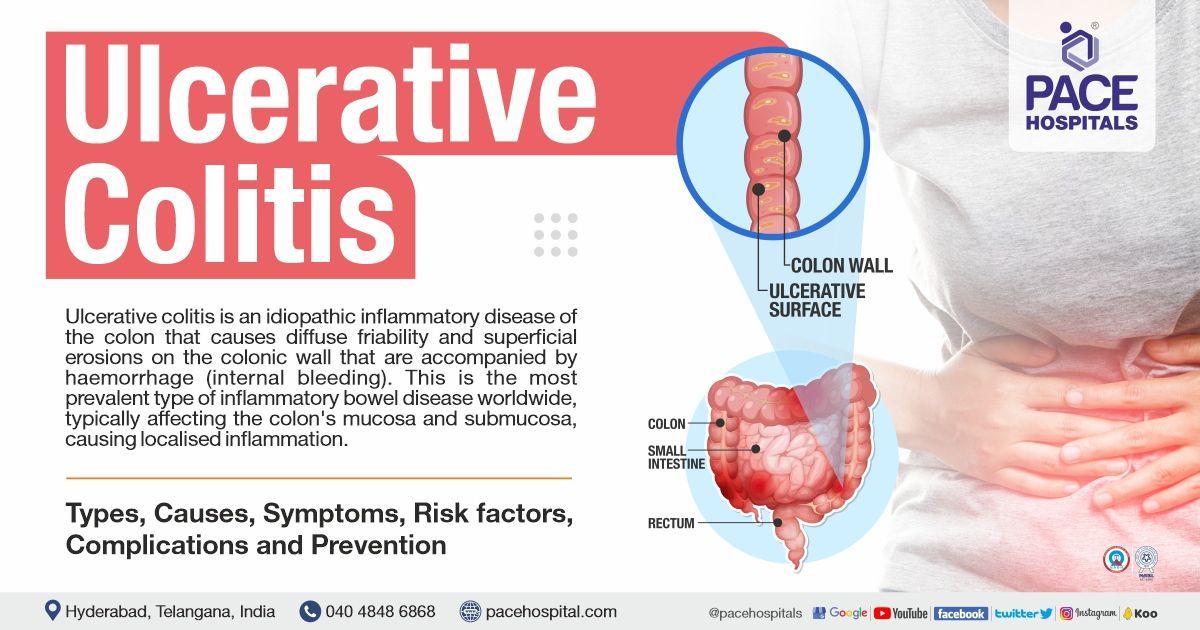
What Is Ulcerative Colitis?
Ulcerative colitis is a chronic inflammatory condition of the large intestine (colon) also known as Colitis, Distal colitis, Pancolitis, Ulcerative proctitis as it causes irritation, swelling, and sores in the inner lining of the bowel. It is one of the main types of inflammatory bowel disease (IBD) and usually follows a pattern of flare-ups and periods of remission.
The disease typically begins in the rectum and may extend continuously to involve part or all of the colon. Inflammation in ulcerative colitis is limited to the innermost layer of the bowel, which helps distinguish it from other inflammatory bowel conditions.
What is mild ulcerative colitis treatment?
Mild ulcerative colitis is generally treated with anti-inflammatory agents from the amino salicylate (5-ASA) class, administered orally or rectally depending on disease location. These medications reduce inflammation in the colon and are effective for inducing and maintaining remission in mild cases. If symptoms persist, topical corticosteroids may be considered as an adjunct therapy (additional treatments used alongside the primary therapy).
What is CMV ulcerative colitis treatment?
When cytomegalovirus (CMV) infection complicates ulcerative colitis, antiviral therapy is required alongside standard ulcerative colitis management. Standard management includes anti-inflammatory agents, corticosteroids, immunomodulators, or biologics, depending on disease severity. Antiviral therapy is essential to address the viral component, as immunosuppression alone may worsen the CMV infection.
What is the first-line treatment for ulcerative colitis?
The first-line treatment for mild-to-moderate ulcerative colitis is the aminosalicylate (5-ASA) class of medications, which can be given orally or rectally. These agents are effective in reducing inflammation and inducing remission. If symptoms are more severe, corticosteroids may be introduced as a short-term measure.
What are the foods to avoid with ulcerative colitis?
Patients with ulcerative colitis are advised to avoid foods that can worsen symptoms, especially during flares. These include high-fiber foods, spicy dishes, fatty foods, caffeine, alcohol, and dairy if lactose intolerant. A low-residue diet may be recommended during active disease to minimize irritation and reduce stool frequency.
What is the difference between ulcerative colitis and colon cancer?
Ulcerative colitis is a chronic inflammatory disease of the colon, while colon cancer is a malignant growth of colonic cells. ulcerative colitis increases the long-term risk of developing colon cancer, but they are distinct conditions with different causes, treatments, and prognoses. Regular surveillance is recommended for ulcerative colitis patients due to this increased risk.
Is ulcerative colitis lifelong?
Ulcerative colitis is generally a lifelong, relapsing-remitting disease. While long periods of remission are possible with appropriate therapy, most patients will experience intermittent flares and require ongoing management. Surgical intervention can be curative, but is not commonly pursued unless necessary.
What is the difference between peptic ulcer and ulcerative colitis?
Peptic ulcer disease involves ulceration of the stomach or duodenal lining, often due to acid or infection, while ulcerative colitis is an inflammatory condition of the colon's mucosal layer. They differ in location, causes, symptoms, and treatment approaches, with ulcerative colitis being an immune-mediated disease and peptic ulcers often related to infection or medication use.
Can ulcerative colitis cause diverticulitis?
Ulcerative colitis and diverticulitis are in distinct conditions, but they can coexist. Ulcerative colitis does not directly cause diverticulitis; however, chronic inflammation may alter the colon's structure, potentially increasing susceptibility. There is no direct causal relationship established in peer-reviewed literature.
Is there any new medicine for ulcerative colitis?
Yes, new drug classes such as Janus kinase (JAK) inhibitors and sphingosine 1-phosphate (S1P) receptor modulators have been developed for ulcerative colitis. These medications offer alternatives for patients who do not respond to traditional therapies like aminosalicylates, corticosteroids, immunomodulators, or biologics.
Can salmonella cause ulcerative colitis?
Salmonella infection does not cause ulcerative colitis, but enteric infections can trigger flares in those with pre-existing ulcerative colitis. Some studies suggest enteric infections may play a role in the onset of inflammatory bowel disease, but a direct causal relationship with salmonella is not established.
Does ulcerative colitis spread?
Ulcerative colitis can extend to involve more of the colon over time, but it does not spread like an infection. The disease typically starts in the rectum and may progress proximally. It is not contagious and does not spread between individuals.
Is ulcerative colitis an autoimmune disease?
Ulcerative colitis is considered an immune-mediated inflammatory disorder with autoimmune features. The immune system attacks the colon's lining, causing chronic inflammation. The exact cause is multifactorial, involving genetic, environmental, and immune factors.
What is the difference between Crohn's disease and ulcerative colitis?
Crohn's disease and ulcerative colitis are both inflammatory bowel diseases. Crohn's can affect any part of the gastrointestinal tract and involves transmural inflammation, while ulcerative colitis is limited to the colon and rectum with inflammation confined to the mucosa. Crohn's often has skip lesions, whereas ulcerative colitis is continuous
Can ulcerative colitis cause diverticulitis?
Ulcerative colitis does not directly cause diverticulitis, but both conditions can coexist. Chronic inflammation from ulcerative colitis may alter colonic structure, potentially increasing susceptibility to diverticula, but a direct causal link is not established in peer-reviewed literature.
Can ulcerative colitis cure itself?
Ulcerative colitis does not cure itself spontaneously. While some patients may experience long periods of remission, ongoing treatment is necessary to control symptoms and prevent complications. Without therapy, most patients will experience relapses and worsening disease.
Can MRI detect ulcerative colitis?
Yes, MRI can identify ulcerative colitis. While MRI is not the major diagnostic technique for ulcerative colitis, it can detect inflammation and other abnormalities in the colon, assisting in the diagnosis and assessment of disease severity. An MRI can also assist distinguish ulcerative colitis from Crohn's disease, another kind of inflammatory bowel disease.
What is the general ulcerative colitis pain location observed in clinical presentations?
Ulcerative colitis pain is usually felt in the lower left side of the belly and around the rectum. This matches the common areas of inflammation in the colon. The pain often feels like cramping and can get worse during flare-ups. While the exact spot of the pain can vary depending on how much of the colon is affected, pain on the left side of the abdomen and rectum is typical in people with ulcerative colitis.
What are extraintestinal manifestations of ulcerative colitis?
Extraintestinal symptoms of ulcerative colitis often affect areas outside the digestive system. The most common are joint pain or swelling (such as arthritis), skin problems (like red, painful bumps or open sores), eye inflammation (including conditions like uveitis and episcleritis), and liver issues (especially a condition called primary sclerosing cholangitis).
These symptoms can appear in about 27 to 47 percent of people with ulcerative colitis and may cause serious health problems. Some of these symptoms come and go with changes in gut inflammation, while others, like liver disease, may happen on their own, regardless of how active bowel disease is.
What are some effective home remedies for ulcerative colitis that may help manage symptoms alongside medical treatment?
Research studies show that some home remedies may help ease the symptoms of ulcerative colitis, although they do not offer a cure. Probiotics, which are found in foods like yogurt and other fermented products, can support gut health and help keep the disease in remission. Natural remedies such as aloe vera, wheatgrass juice, turmeric (which contains curcumin), and neem have shown anti-inflammatory effects and may help lower disease activity. Making changes to the diet, managing stress, and staying physically active are also useful steps that can support regular medical treatment.
What are the signs and symptoms of ulcerative colitis?
Ulcerative colitis often causes bloody diarrhea and frequent loose stools. People may also have rectal bleeding, cramping or pain in the lower belly, a strong urge to have a bowel movement, and mucus in the stool. Other common symptoms include feeling very tired, losing weight, having a reduced appetite, and in more serious cases, fever and low red blood cell levels.
Some individuals may wake up at night to use the bathroom, feel like they cannot fully empty their bowels, or have a tender abdomen. The type and severity of symptoms can differ based on how much of the colon is affected and how active the disease is.
What does the lead pipe sign ulcerative colitis indicate on imaging studies, and how it is related to disease progression?
The lead pipe sign in ulcerative colitis refers to the colon looking smooth and stiff on imaging tests, especially on a barium enema X-ray. This happens because the normal folds in the colon are lost over time. It is a sign of long-term disease and shows that the colon has gone through lasting changes due to ongoing inflammation. Seeing this sign means the condition has been present for a while and is more serious.
How Much Does Ulcerative Colitis Surgery Cost in Hyderabad, India?
At PACE Hospitals, the cost of ulcerative colitis surgery in Hyderabad depends on the type of surgical procedure required, disease severity, and individual clinical needs.
Approximate Ulcerative Colitis Surgery Cost at PACE Hospitals:
- Subtotal or Total Colectomy: ₹2,80,000 – ₹4,50,000 (USD $3,350 – $5,400)
- Proctocolectomy with Ileostomy or J-pouch Surgery: ₹3,80,000 – ₹6,50,000 (USD $4,550 – $7,800)
The overall cost may vary based on:
- Nature of surgery (planned or emergency)
- Surgical approach (open or minimally invasive)
- Length of hospital stay and ICU care, if required
- Preoperative evaluation and postoperative recovery support
Ulcerative colitis surgery at PACE Hospitals is delivered by an experienced multidisciplinary team with access to advanced operation theatres, comprehensive perioperative care, and transparent treatment planning, ensuring safe outcomes and cost clarity for patients.