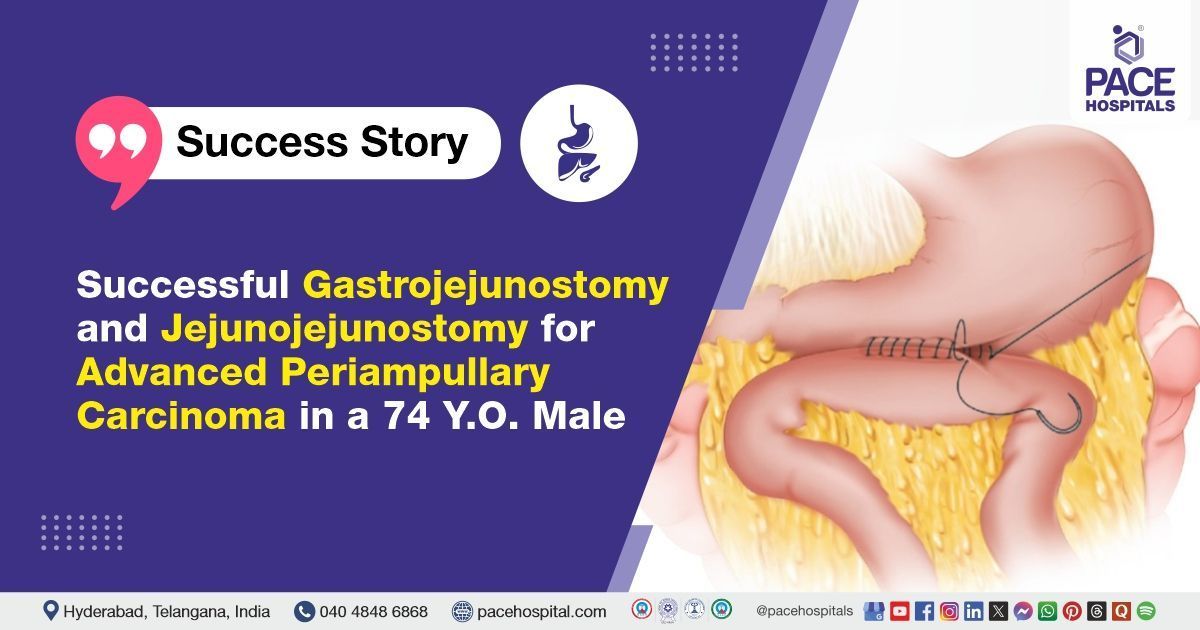
Successful Gastrojejunostomy and Jejunojejunostomy for Advanced Periampullary Carcinoma in a 74 Y.O. Male
PACE Hospitals
PACE Hospitals’ expert Surgical Gastroenterology team successfully performed a Gastrojejunostomy along with a Jejunojejunostomy on a 74-year-old male patient diagnosed with gastric outlet obstruction secondary to a periampullary mass. The aim of the procedure was to bypass the obstructed segment of the gastrointestinal tract, restore continuity of the intestinal pathway, relieve the obstruction, facilitate adequate oral intake, and thereby improve the patient’s nutritional status and overall quality of life.
Chief Complaints
A 74-year-old male patient with a
body mass index (BMI) of 22 presented to the Surgical Gastroenterology Department at
PACE Hospitals, Hitech City, Hyderabad, with complaints of abdominal distension and vomiting for the past 2 days.
Past Medical History
The patient is a known case of
type 2 diabetes mellitus on regular treatment. He previously underwent an emergency exploratory laparotomy with T tube insertion into the common bile duct (CBD) and peritoneal lavage for biliary peritonitis following a laparoscopic common bile duct exploration (LCBDE).
On Examination
On examination, the patient was alert and oriented and appeared mildly dehydrated with signs of volume depletion. General physical examination revealed no pallor, icterus, cyanosis, clubbing, or pedal edema, though mild cachexia was noted. The abdomen was distended with visible peristalsis and a well-healed midline laparotomy scar. On palpation, there was mild diffuse tenderness without guarding or rigidity. A firm, non-mobile mass was palpable in the epigastric region, suggesting a periampullary or pancreatic head lesion. Bowel sounds were sluggish, and there was no evidence of free fluid. Systemic examination showed normal heart sounds without murmurs, clear lung fields on auscultation, and no focal neurological deficits.
Diagnosis
Following clinical examination, the Surgical Gastroenterology team conducted a comprehensive assessment, including a detailed review of the patient’s medical history and focused clinical evaluation. Routine blood investigations revealed microcytic hypochromic anemia, tumor marker (CA) was markedly elevated, neutrophilic predominance, and with normal renal and liver function tests.
Diagnostic investigations included CECT abdomen and histopathology, which identified it as Gastric outlet obstruction secondary to periampullary mass with peritoneal metastatic adenocarcinoma.
Based on the confirmed diagnosis, he was advised to undergo Gastric Outlet Obstruction Treatment in Hyderabad, India, under the expert care of the Surgical Gastroenterology team, ensuring accurate diagnosis, effective treatment, and optimal recovery.
Medical Decision Making
After a detailed consultation with Dr. Suresh Kumar S, Surgical Gastroenterologist GI and HPB Oncologist and cross consultations with Dr. Tripti Sharma, Dr. Pradeep Kiran Panchadi, Dr. Seshi Vardhan Janjirala, a thorough evaluation was conducted considering the patient's complaints of abdominal distension, vomiting, history of emergency exploratory laparotomy for biliary peritonitis following laparoscopic common bile duct exploration (LCBDE), and a known history of diabetes mellitus under regular treatment.
Clinical examination, imaging studies including CECT abdomen, and histopathology confirmed the diagnosis of gastric outlet obstruction secondary to a periampullary mass with metastatic peritoneal deposits. Given the patient’s deteriorating symptoms and underlying malignancy, it was determined that gastrojejunostomy along with jejunojejunostomy was identified as the most appropriate intervention to bypass the obstruction and improve quality of life.
The patient and his family members were counselled regarding the diagnosis, the planned surgical procedure, its associated risks, and its potential to alleviate symptoms and improve his quality of life.
Surgical Procedure
Following the decision, the patient was scheduled to undergo Gastrojejunostomy along with Jejunojejunostomy (Braun loop) Surgery in Hyderabad at PACE Hospitals, under the supervision of an expert in the Surgical Gastroenterology Department.
The following steps were carried out during the procedure:
- Abdominal Exploration and Adhesiolysis: After achieving general anesthesia and ensuring proper sterile draping, a midline laparotomy incision was made. On entering the abdominal cavity, dense interbowel adhesions and adhesions to the abdominal wall were encountered. These were carefully dissected and adhesiolysis was performed to gain access to the operative field.
- Identification of the Obstruction and Pathology: Upon exploration, the stomach was found to be grossly distended, and a hard mass was palpable at the head of the pancreas, consistent with a periampullary growth causing gastric outlet obstruction. Peritoneal deposits, likely metastatic, were also noted in the right upper quadrant. A suspicious lymph node was identified, and a biopsy was taken for histopathological evaluation.
- Gastrojejunostomy Construction: A jejunal loop approximately 40 cm distal to the duodenojejunal flexure (DJ) was identified. A side-to-side Gastrojejunostomy (GJ) was performed between the posterior wall of the stomach and the antimesenteric border of the jejunum using hand-sewn technique, ensuring a wide and tension-free anastomosis to bypass the obstructed duodenum.
- Jejunojejunostomy (Braun Loop) Creation: To divert bile and pancreatic secretions and reduce the risk of bile reflux gastritis, a Jejunojejunostomy (Braun loop) was constructed distal to the GJ site. This was performed by a side-to-side anastomosis between the afferent and efferent limbs of the jejunal loop, providing smooth passage of intestinal contents.
- Hemostasis and Closure: After ensuring adequate hemostasis and peritoneal lavage, a drain was placed if indicated. The abdominal wall was closed in layers using appropriate sutures. The patient was then shifted to recovery in a hemodynamically stable condition.
Postoperative Care
The procedure was completed without complications, and the patient remained stable throughout. Postoperatively, he was managed with IV fluids, antibiotics, analgesics, antacids, and laxatives. Due to delayed gastric emptying, he was started on total parenteral nutrition (TPN). CT scan showed minimal left paracolic collection, which did not required intervention. The patient improved gradually and was discharged in a stable condition.
Discharge Medications
Upon discharge, the patient was prescribed a proton pump inhibitor for acid suppression, a magnesium supplement for electrolyte balance, and a laxative to aid in bowel regulation. A nutritional supplement was advised to support overall nutritional needs. Additionally, oral antidiabetic medications were continued for the management of type 2 diabetes mellitus.
Advice on Discharge
The patient was advised to maintain proper wound care to prevent infection and promote healing. Use of an abdominal binder was recommended to provide support and reduce postoperative discomfort.
Dietary Advice
A soft, easily digestible diet was advised to facilitate smooth gastrointestinal recovery.
Emergency Care
The patient was informed to contact the emergency ward at PACE Hospitals in case of any emergency or development of symptoms such as fever, abdominal pain and vomiting.
Review and Follow-up Notes
The patient was advised to return for a follow-up visit with the Surgical Gastroenterologist in Hyderabad at PACE Hospitals, after 5 days, for further evaluation.
Conclusion
This case highlights the successful palliative management of gastric outlet obstruction secondary to a periampullary mass with metastatic deposits through gastrojejunostomy with Braun jejunojejunostomy. The patient recovered well postoperatively, was discharged in a stable condition, and was advised on wound care, dietary modifications, diabetes management, and regular follow-up to ensure optimal recovery and improved quality of life.
Integrative Approaches to Optimizing Outcomes in GI Disorders: A Multidisciplinary Perspective
Management of complex gastrointestinal conditions, such as malignant obstructions requiring surgical bypass, benefits significantly from an integrative multidisciplinary approach. A surgical Gastroenterologist / Surgical gastroenterology doctor plays a crucial role in performing the necessary surgical intervention, while collaboration with endocrinology helps manage comorbidities like diabetes. Targeted nutritional support, including soft diets and supplements, combined with meticulous postoperative care, such as wound management and the use of an abdominal binder, is essential for optimal recovery. Regular monitoring through imaging and laboratory tests allows early detection of complications, further enhancing patient outcomes. This comprehensive strategy demonstrates how combining surgical, medical, nutritional, and supportive care tailored to the patient’s overall health leads to improved stability and quality of life in challenging GI disorders.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868