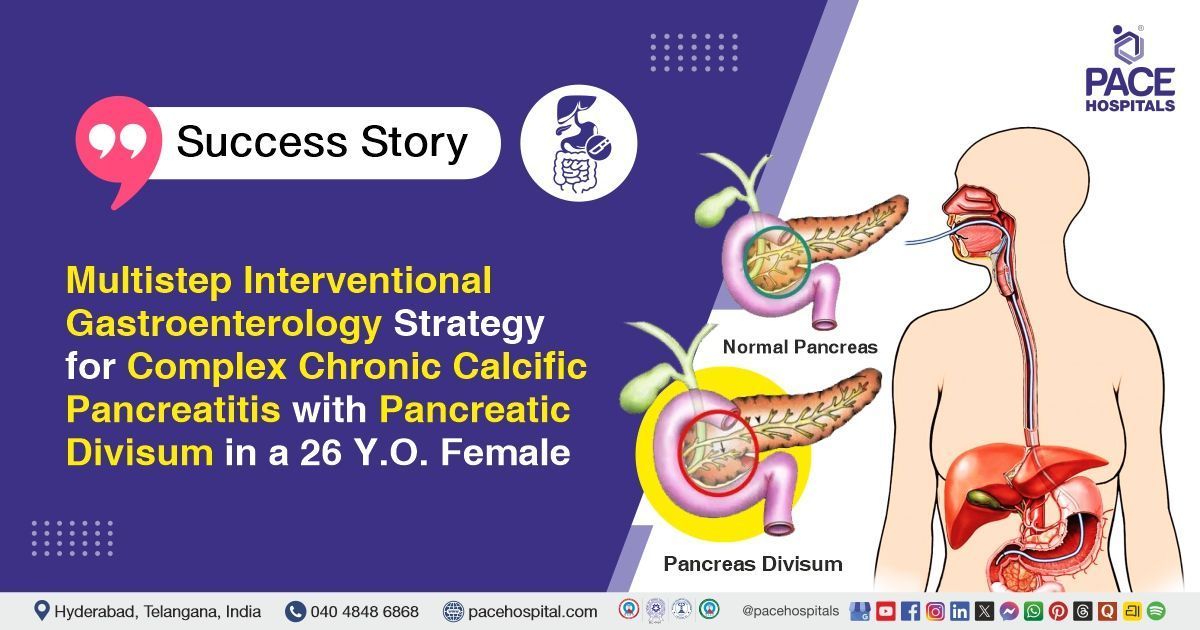
Multistep Interventional Gastroenterology Strategy for Complex Chronic Calcific Pancreatitis with Pancreatic Divisum in a 26 Y.O. Female
PACE Hospitals
PACE Hospitals’ expert Gastroenterology team successfully performed Endoscopic Retrograde Cholangiopancreatography (ERCP) with pancreatic duct (PD) stent removal and pancreatic duct clearance on a 26-year-old female patient diagnosed with chronic calcific pancreatitis. The procedure aimed to relieve pancreatic duct obstruction by removing the stent and calcific deposits, restore normal drainage, reduce pain, and prevent further pancreatic damage.
Chief Complaints
A 26-year-old female with a
body mass index (BMI) of 19 presented to the Gastroenterology Department at
PACE Hospitals, Hitech City, Hyderabad, with complaints of abdominal bloating, a burning sensation in the chest, and belching for the past two months. These symptoms were associated with
constipation without medication, watery stools with medication, and generalized myalgias including neck pain and backache.
Past Medical History
The patient had a known history of chronic calcific pancreatitis associated with pancreatic divisum (a congenital condition where pancreatic ducts do not join properly) previously managed with ERCP, pancreatic sphincterotomy, and pancreatic duct stenting, migraine without aura, depressive disorder, sickle cell trait, and polycystic ovary syndrome (PCOS). She also underwent an appendectomy in the past.
On Examination
On general examination, the patient was conscious, coherent and oriented, and hemodynamically stable. Vital signs were within normal limits. Systemic examination revealed a soft, non-tender abdomen, with no abnormal findings noted.
Diagnosis
Upon admission to PACE Hospitals, the patient was thoroughly evaluated by the Gastroenterology team, which included a clinical examination and a history of abdominal bloating, burning sensation in the chest, belching for two months, constipation without medication, watery stools with medication, and generalized myalgias including neck pain and backache.
The patient underwent necessary investigations. CT abdomen revealed an atrophied pancreas with parenchymal calcifications predominantly in the head and uncinate process, a mildly dilated main pancreatic duct with stent in situ, and small intraductal calculi, suggestive of chronic calcific pancreatitis. Ultrasound abdomen confirmed pancreatic atrophy with a prominent main pancreatic duct. Routine laboratory investigations, including complete blood picture, renal and liver function tests, electrolytes, coagulation profile, thyroid profile, pancreatic enzymes, lipid profile, and urine examination, were within normal limits. Glycosylated hemoglobin was consistent with de novo diabetes mellitus.
Based on the confirmed diagnosis, the patient was advised to undergo Chronic Calcific Pancreatitis Treatment in Hyderabad, India, under the expert care of the Gastroenterology Department, to effectively relieve symptoms and prevent further progression of the disease.
Medical Decision Making (MDM)
After a detailed consultation with consultant gastroenterologists, Dr. Govind Verma, Dr. M Sudhir, Dr. Padma Priya and cross consultation with endocrinologist, Dr. Tripti Sharma, a thorough evaluation was conducted considering the patient’s complaints of abdominal bloating, epigastric burning, belching, constipation, and history of chronic calcific pancreatitis. All relevant laboratory, imaging, and prior procedural data were reviewed.
Based on these clinical and imaging findings, it was determined that Endoscopic Retrograde Cholangiopancreatography (ERCP) with Pancreatic Duct (PD) stent removal and pancreatic duct clearance was identified as the most appropriate intervention to relieve her symptoms, prevent recurrent ductal obstruction, and mitigate further complications associated with chronic calcific pancreatitis.
The patient and her family members were counselled regarding the diagnosis, the planned procedure, its associated risks, including pancreatitis, bleeding, or infection, and its potential to relieve symptoms, improve digestive function, and enhance quality of life.
Surgical Procedure
Following the decision, the patient was scheduled to undergo ERCP with Pancreatic Duct Stent Removal and Pancreatic Duct Clearance in Hyderabad at PACE Hospitals under the expert care of the Gastroenterology Department.
The following steps were carried out during the procedure:
- Patient Positioning and Anesthesia: The patient was positioned in the left lateral decubitus position. After obtaining informed consent, conscious sedation or general anesthesia was administered, and vital signs were continuously monitored throughout the procedure.
- Endoscopic Access: A side-viewing duodenoscope was gently introduced through the mouth, esophagus, and stomach to reach the second part of the duodenum. The major duodenal papilla was identified as the entry point to the pancreatic duct.
- Pancreatic Duct Cannulation and Imaging: Using a guidewire and catheter, the pancreatic duct was selectively cannulated. Contrast dye was injected under fluoroscopic guidance to delineate the pancreatic duct anatomy, identify the stent position, and detect any strictures or intraductal calculi.
- Stent Removal and Duct Clearance: The previously placed pancreatic duct stent was carefully grasped and removed using specialized retrieval devices. Any intraductal debris, protein plugs, or calculi were cleared using balloon catheters or extraction baskets to ensure complete ductal clearance.
- Final Assessment and Recovery: A final fluoroscopic check was performed to confirm complete ductal clearance and absence of immediate complications. The endoscope was withdrawn carefully, and the patient was shifted to the recovery area for observation.
Postoperative Care
The patient was managed for infection, acid suppression, and general supportive care during the hospital stay. She showed significant symptomatic improvement and remained hemodynamically stable and was therefore discharged with appropriate medical advice.
Discharge Medications
Upon discharge, the patient was prescribed medications to manage infection, reduce acid-related symptoms, support pancreatic enzyme function for digestion, relieve constipation, provide antioxidant support, address mood-related concerns, and treat severe headaches as needed.
Advice on Discharge
The patient was advised to consume small, frequent meals to improve digestion, reduce pancreatic workload, and help manage symptoms effectively.
Emergency Care
The patient was informed to contact the emergency ward at PACE Hospitals in case of any emergency or development of symptoms such as fever, abdominal pain, vomiting and chest pain.
Review and Follow-up Notes
The patient was advised to return for a follow-up visit with the Gastroenterologist in Hyderabad at PACE Hospitals after 3 months for further evaluation and follow-up visit with the endocrinologist after 3 months.
Conclusion
This case highlights a patient with chronic calcific pancreatitis associated with pancreatic divisum (a congenital condition where pancreatic ducts do not join properly), who underwent ERCP with PD stent removal and pancreatic duct clearance. The patient showed significant symptomatic improvement and remained hemodynamically stable. She was discharged with appropriate medical therapy, dietary guidance, and instructions for follow-up.
Multidimensional Care in Chronic Calcific Pancreatitis with Comorbidities
Chronic calcific pancreatitis often requires a holistic approach due to its progressive nature and potential multisystem involvement. Management typically combines endoscopic interventions, such as pancreatic duct stenting or stone clearance, with supportive care including enzyme supplementation, pain control, and dietary modifications. Comorbid conditions like diabetes, metabolic disorders, or psychological issues should be addressed simultaneously to optimize overall health.
Regular monitoring of pancreatic function and systemic complications is essential for early detection of deterioration. A multidisciplinary team including gastroenterologist/gastroenterology doctor, endocrinologists, dietitians, and mental health professionals ensures comprehensive care. Emphasizing patient education and lifestyle modifications further supports long-term outcomes and quality of life.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles