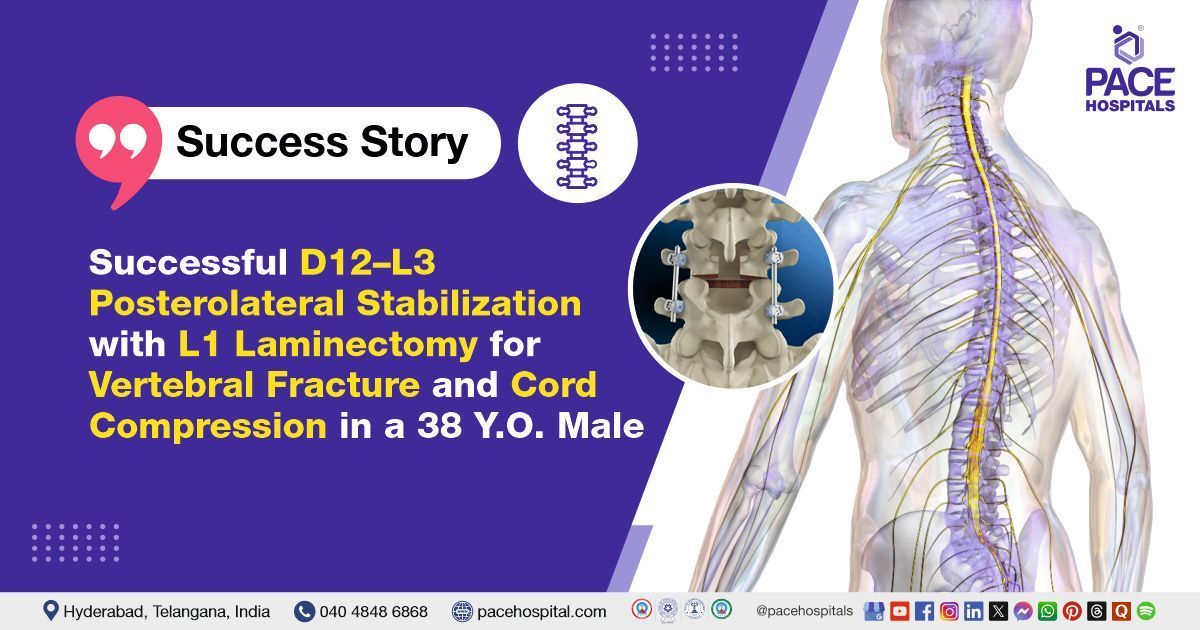
Successful D12–L3 Posterolateral Stabilization with L1 Laminectomy for Vertebral Fracture and Cord Compression in a 38-Y.O. Male
PACE Hospitals
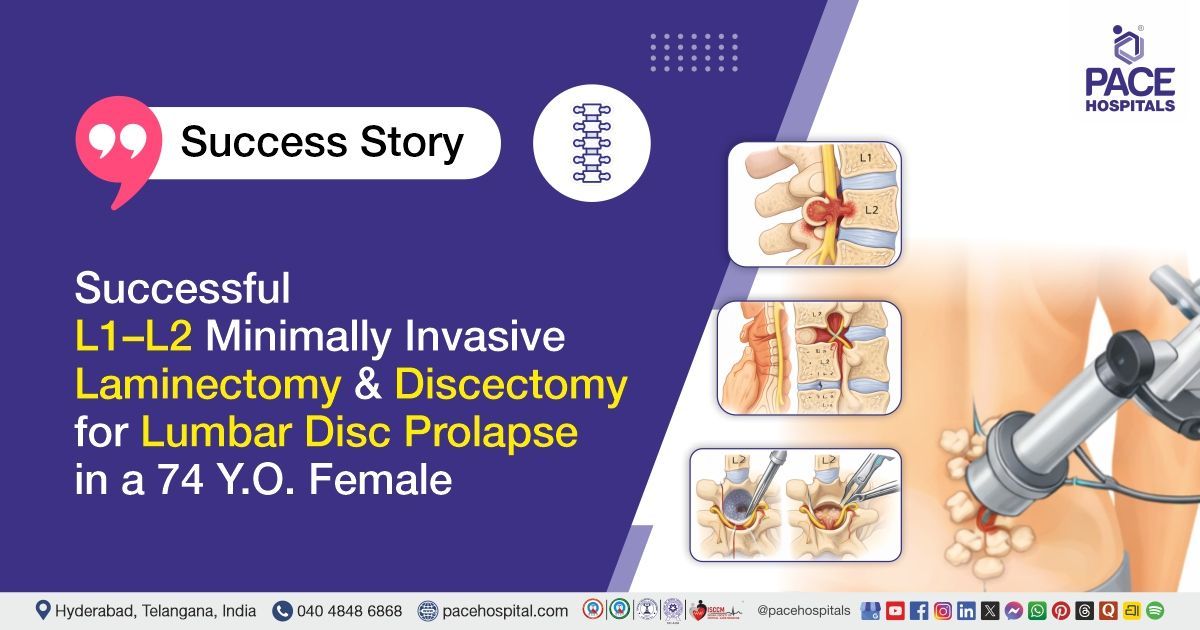
PACE Hospitals’ expert Neurosurgery team successfully performed a D12–L3 Posterolateral Stabilisation and Fusion with L1 Laminectomy on a 38-year-old male patient diagnosed with an L1 vertebral fracture with retrolisthesis and spinal cord compression. The aim of the procedure was to decompress the spinal cord, stabilise the spine, and relieve persistent back pain that had been worsening over the past two months.
Chief Complaints
A 38-year-old male patient with a
body mass index (BMI) of 18 presented to the Neurosurgery Department at
PACE Hospitals, Hitech City, Hyderabad, with complaints of severe back pain for the past two months. Initially, the pain occurred only while walking, but progressively worsened to become persistent even at rest. The patient also complained of stiffness and bowel irregularities. There was no history of limb weakness or fever.
Past Medical History
The patient is a known case of Crohn’s disease and had previously undergone a distal gastrectomy. He had a history of an alleged fall at the workplace about 9 months prior. The patient followed a mixed diet.
On Examination
On examination, the patient was moderately built and ill-nourished, conscious, coherent, and cooperative, with stable vital signs. Motor strength was 4+/5 in both lower limbs. Sensory examination was normal. Cranial nerves were normal, and cerebellar signs were absent. There were no signs of meningeal irritation. Deep tendon reflexes were normal, and the Babinski sign was absent. Cardiovascular examination revealed normal heart sounds without murmurs. Respiratory examination showed bilateral air entry. Abdominal examination was unremarkable, with a soft, non-tender abdomen and no palpable organomegaly or masses.
Diagnosis
Upon admission, the patient underwent a comprehensive clinical evaluation along with a review of medical history and detailed diagnostic investigations conducted by the Neurosurgery team.
To support clinical findings, laboratory and special investigations were carried out as part of the preoperative assessment. The complete blood count (CBC) revealed low hemoglobin and reduced red blood cell count, suggestive of anemia. There was a relative increase in neutrophils. Liver function tests (LFTs) showed low albumin and total protein levels, indicating hypoalbuminemia, whereas liver enzymes were within normal range. Serum potassium levels were found to be mildly low. Vitamin D levels were severely low, while serum vitamin B12 levels were significantly high.
Microbiological investigations revealed blood and urine cultures. Aerobic blood culture showed growth of Staphylococcus aureus (MRSA), which was sensitive to certain antibiotics but resistant to multiple others. Anaerobic blood culture and urine culture showed no bacterial growth. Gram stain of blood samples revealed moderate gram-positive cocci.
Cardiac evaluation through a 2D echocardiogram showed Grade I left ventricular diastolic dysfunction was noted. Chest X-ray revealed mild fibrotic changes in both mid-lung zones. Imaging of the lumbar spine indicated a fracture of a lumbar vertebra. Viral markers for HIV, Hepatitis B, and Hepatitis C were non-reactive. Serum calcium levels were low, while blood sugar levels were normal.
Based on the confirmed diagnosis, the patient was advised to undergo
Lumbar vertebral fracture with retrolisthesis and spinal cord compression treatment in Hyderabad, India, under the expert care of the Neurosurgery Department.
Medical Decision Making
After a detailed consultation with Dr. U.L. Sandeep Varma, Neurosurgeon, and Dr. Govind Verma, Gastroenterologist, a thorough preoperative assessment was conducted focusing on the patient’s severe back pain, history of Crohn’s disease with distal gastrectomy, and recent worsening of symptoms. Given the history of an alleged fall nine months prior, clinical findings of stiffness, bowel irregularities, and imaging confirming an L1 fracture with retrolisthesis and spinal cord compression, the risk of neurological compromise was considered significant.
Imaging of the lumbar spine showed a vertebral fracture with associated spinal instability. Cardiac evaluation indicated grade I left ventricular diastolic dysfunction, but overall cardiac function was adequate for surgery.
Based on their collective expertise and assessment, it was determined that D12-L3 posterolateral stabilization and fusion along with L1 laminectomy was identified as the most effective intervention to stabilize the spine, decompress the cord, relieve symptoms, and prevent further neurological deterioration.
The patient and his family were informed about the diagnosis, surgical procedure, associated risks, expected benefits such as symptom relief and improved mobility, and postoperative care and follow-up plans to ensure optimal recovery and monitoring.
Surgical Procedure
Following the decision, the patient was scheduled to undergo D12-L3 posterolateral stabilization and fusion along with L1 Laminectomy surgery in Hyderabad at PACE Hospitals, under the expert supervision of the Neurosurgery Department.
The procedure involved the following steps:
- Preparation and Positioning: Under strict aseptic precautions and general anesthesia, the patient was positioned prone. The surgical area from D12 to L3 was painted and draped appropriately.
- Incision and Exposure: A vertical midline incision was made extending from D12 to L2. The incision was deepened, and the paraspinal muscles were separated to expose the laminae, spinous processes, and transverse processes.
- Pedicle Screw Fixation and Stabilization: Bilateral pedicle screw fixation was performed from D12 to L3. The spine was stabilized using titanium rods bilaterally connecting the screws.
- Laminectomy and Decompression: Laminectomy was performed at the L1 vertebral level, and the ligamentum flavum was excised. The dura was found to be pulsatile at the end of the decompression procedure.
- Fusion: Posterolateral fusion was performed from D12 to L3 using autologous bone graft.
- Hemostasis and Closure: Hemostasis was secured. A drain and epidural catheter were placed. The wound was closed meticulously in layers.
Postoperative Care
The postoperative period was uneventful. The patient was initially shifted to the Intensive Care Unit (ICU) for overnight monitoring and then moved to a regular ward. The drain and Foley catheter were removed on postoperative day 2, and the patient was successfully ambulated. Medical and gastroenterology consultations were obtained, and their advice was followed. Postoperative X-rays confirmed that the implants were in proper alignment. Intravenous antibiotics, proton pump inhibitors, analgesics, and other supportive treatments were administered as per protocol.
The patient showed symptomatic improvement and remained hemodynamically stable throughout the hospital stay. Detailed instructions regarding wound care, medications, and
physiotherapy were provided. The patient was stable with healthy wound healing. Muscle strength was graded 4+/5 in both lower limbs. The patient was ambulatory and able to walk independently.
Discharge Medications
The patient was prescribed an antibiotic to prevent or treat infection, along with a muscle relaxant combined with vitamin B complex to alleviate muscle spasms and support nerve health. An opioid analgesic was given for pain management. A proton pump inhibitor was included as a gastroprotective agent to prevent gastrointestinal irritation. Calcium and vitamin C, D supplements were provided to support bone health and aid recovery. An immunosuppressant was continued to manage the patient’s underlying condition.
Advice on Discharge
The patient was advised to continue limb physiotherapy as instructed. A review with the medical gastroenterologist was recommended for ongoing management of Crohn’s disease. The patient was advised to avoid strenuous exercise but was encouraged to walk and climb stairs as tolerated. Wound care instructions were given, including that bathing is permitted. The patient was advised to avoid sitting on the floor and lifting heavy weights. Strict compliance with prescribed medications was emphasized. Stapler removal was scheduled as part of the postoperative care.
Emergency Care
The patient was informed to contact the emergency ward at PACE Hospitals in case of any emergency or development of symptoms such as fever, abdominal pain, wound drainage, and vomiting.
Review and Follow-up Notes
The patient was advised to follow up with the Neurosurgeon in Hyderabad at PACE Hospitals after 25 days to review his condition.
Conclusion
This case highlights the successful diagnosis and surgical management of an L1 fracture with retrolisthesis and cord compression. The patient underwent D12-L3 posterolateral stabilization and fusion along with L1 laminectomy. The patient showed stable postoperative recovery with planned follow-up and rehabilitation.
The Crucial Role of Imaging in Diagnosing Spinal Cord Compression
Imaging played a crucial role in this case by clearly identifying the spinal problem. While the X-rays showed the fracture and the misalignment of the vertebra (retrolisthesis), the MRI provided a detailed view of the spinal cord and confirmed the presence of cord compression. These findings not only explained the patient’s severe pain and stiffness but also guided the doctors in planning the right surgical approach to both stabilize the spine and relieve pressure on the cord. Without imaging, it would have been difficult to fully understand the extent of spinal instability and ensure that the most effective treatment was chosen. In this case, the expert guidance of a neurosurgeon / neurosurgery doctor was essential in interpreting the scans and deciding the best treatment path for a safe recovery.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868