Lupus Disease -Types, Symptoms, Causes, Treatment & Prevention
PACE Hospitals
Written by: Editorial Team
Medically reviewed by: Dr. Shweta Bhardwaj - Consultant Rheumatologist and Clinical Immunologist
Overview | Prevalence | Types | Symptoms | Causes | Risk Factors | Complications | Diagnosis | Treatment | Prevention | FAQs | When to consult a Doctor
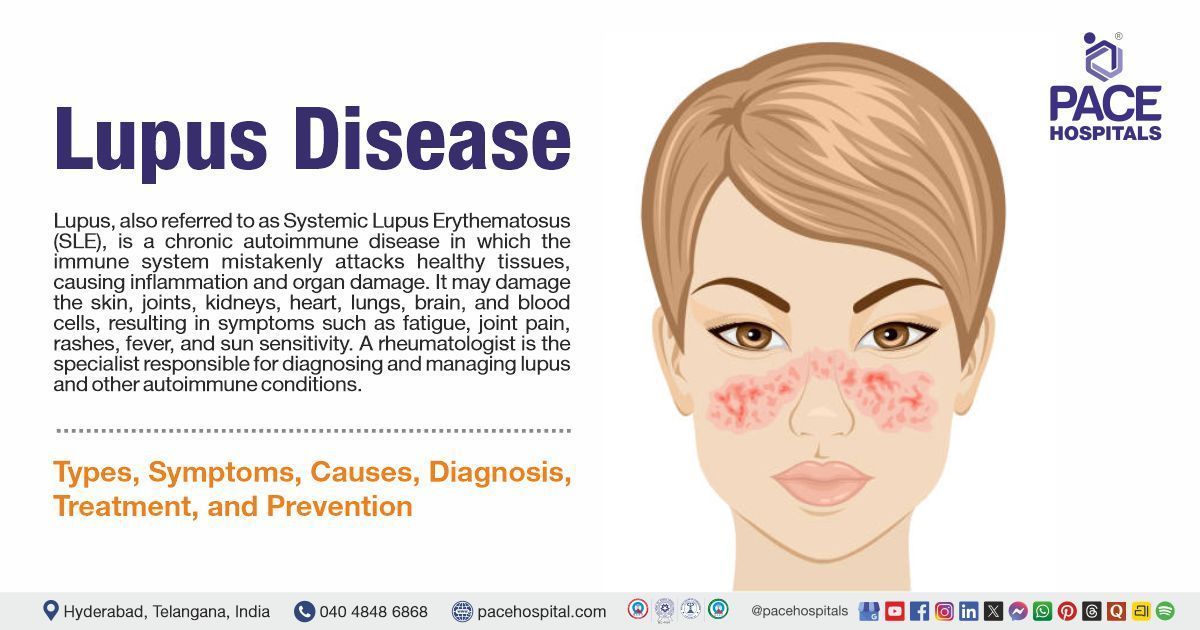
Lupus (Systemic Lupus Erythematosus) definition
Lupus, also known as Systemic Lupus Erythematosus (SLE), is a chronic autoimmune condition that can affect multiple organs and systems throughout the body. In lupus, the immune system, which normally protects the body against infections, mistakenly attacks healthy tissues. This abnormal immune response results in inflammation and, in some cases, permanent tissue damage. The effects of lupus can be widespread, potentially involving the skin, joints, kidneys, heart, lungs, brain, blood cells, and other organs, resulting in a variety of symptoms, including fever, sensitivity to sunlight, skin rashes (often a butterfly-shaped rash on the face), joint pain and swelling, and chronic fatigue.
A Rheumatologist is a doctor who specializes in diagnosing and managing autoimmune and inflammatory diseases, including systemic lupus erythematosus (SLE).
Lupus meaning
The word "lupus" originates from the Latin term lupus, meaning "wolf." It was first used in the late 14th century to describe skin diseases that caused severe sores or ulcers. The name was likely chosen due to the damage to the skin, which appeared as if it had been eaten away, similar to a wolf's bite. In early medical texts, it was sometimes referred to simply as "wolf." Over time, the term became specifically associated with systemic lupus erythematosus (SLE), the autoimmune disease known today.
Prevalence of systemic lupus erythematosus
Prevalence of lupus in the world
As for overall prevalence, about 43.7 people per 100,000 are living with SLE worldwide, roughly 34.1 lakh people. Women are more affected, with a prevalence of 78.73 per 100,000 (approximately 30.4 lakh), while men have a lower prevalence of 9.26 per 100,000 (approximately 360,000 cases). The United Arab Emirates, Barbados, and Brazil have the highest prevalence rates. These differences in SLE statistics are influenced by region, sex, age, and how prevalence is measured.
Prevalence of lupus in India
Systemic lupus erythematosus (SLE) is an autoimmune disease that primarily affects women of reproductive age. In India, the reported prevalence is approximately 3.2 per 100,000 people, although this number may be higher in urban areas and among South Asians living abroad. As India continues to urbanize, more cases are being identified, especially in tertiary care hospitals.
Despite a lower reported prevalence compared to Western countries, India is likely to have over 50,000 SLE patients due to its large and youthful population. Notably, many cases involve juvenile-onset SLE, which tends to be more severe and challenging to treat. However, the limited number of trained rheumatologists in India poses significant challenges for timely diagnosis and effective management of the disease.
Types of Lupus
Lupus is an autoimmune disease with several types. The following are the different types of lupus:
- Systemic lupus erythematosus (SLE)
- Cutaneous lupus erythematosus (CLE)
- Drug-induced lupus erythematosus
- Neonatal lupus erythematosus
Systemic lupus erythematosus (SLE)
The most often mentioned form of lupus is systemic lupus erythematosus (SLE), an autoimmune illness. The immune system of the body mistakenly targets healthy tissues in SLE, causing tissue damage and inflammation. It can impact the kidneys, brain, joints, skin, and other organs. It can cause complications like lupus nephritis (kidney inflammation).
Cutaneous lupus erythematosus (CLE)
This type primarily affects the skin, causing rashes, lesions, and other skin-related issues. There are 3 types of cutaneous lupus erythematosus (CLE)they are:
- Acute cutaneous lupus erythematosus (ACLE)
- Subacute cutaneous lupus erythematosus (SCLE)
- Chronic cutaneous lupus erythematosus (CCLE) or discoid lupus erythematosus (DLE)
Drug-induced lupus erythematosus
It is a form of lupus that is different from systemic lupus erythematosus and is triggered by certain prescription medications. Its symptoms are similar to those of SLE, frequently involving joint pain and inflammation around the lungs. The condition usually improves once the offending drug is discontinued.
Neonatal lupus erythematosus
It is a rare condition that occurs in newborns of mothers who carry anti-Ro and anti-La antibodies. These maternal antibodies can affect the baby's heart conduction system and may lead to symptoms at birth, such as a skin rash, liver abnormalities, or a low blood cell count.
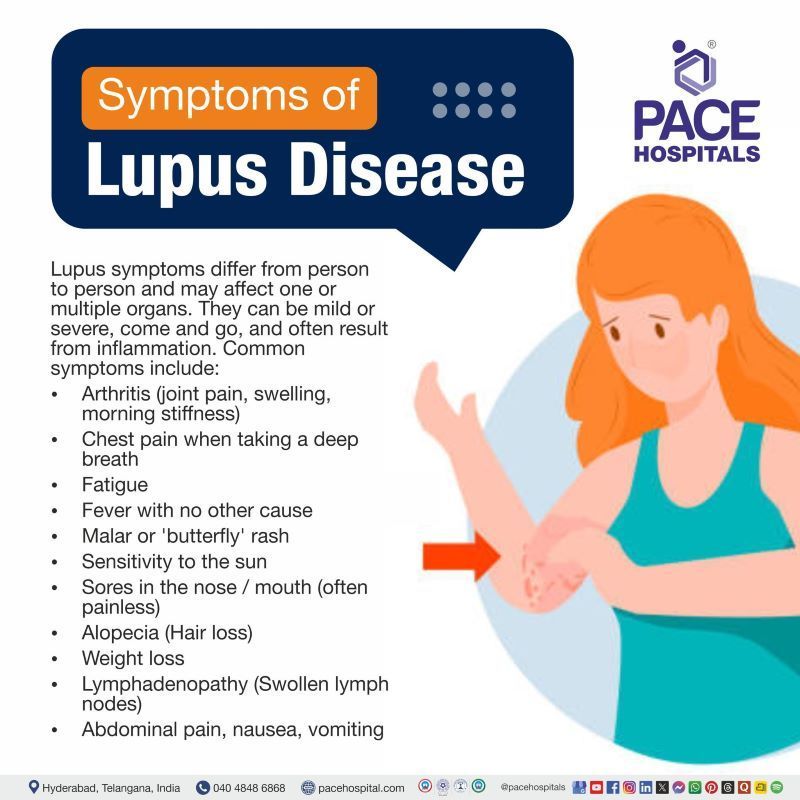
Lupus Symptoms
Signs and symptoms of lupus disease vary from person to person and can range from mild to severe. Some patients may experience only a few symptoms affecting a specific part of the body, while others may have widespread symptoms involving multiple systems. The symptoms can come and go, and new ones may appear over time. Many are caused by inflammation affecting different organs and tissues, including the joints, skin, kidneys, brain, blood cells, and the linings of the heart and lungs. The most common systemic lupus erythematosus symptoms include:
- Arthritis (joint pain, swelling, morning stiffness)
- Chest pain when taking a deep breath
- Fatigue
- Fever with no other cause
- Malar or 'butterfly' rash
- Sensitivity to the sun
- Sores in the nose/mouth (often painless)
- Alopecia (Hair loss)
- Weight loss
- Lymphadenopathy (Swollen lymph nodes)
- Abdominal pain, nausea, vomiting
Arthritis (joint pain, swelling, morning stiffness): Non-erosive arthritis is common in lupus, typically affecting the small joints of the hands and knees. It causes stiffness, especially in the morning, along with pain and visible swelling.
Chest pain when taking a deep breath: This may indicate pleuritis or pericarditis, both are inflammatory complications of lupus affecting the lungs or heart, causing sharp, stabbing pain during deep inspiration.
Fatigue: It is one of the most common and disabling symptoms, fatigue in lupus can occur even when the disease is inactive, significantly impacting daily life and energy levels.
Fever with no other cause: Low-grade fever may result from systemic inflammation during disease flares, even in the absence of infection, and can be an early warning sign of a flare-up.
Malar or 'butterfly' rash: A classic rash of lupus appears across the cheeks and bridge of the nose, often triggered or worsened by sun exposure. It is usually flat or slightly raised and non-itchy.
Sensitivity to the sun: Also called photosensitivity, exposure to ultraviolet (UV) light can trigger rashes or systemic flares in lupus patients, leading to skin irritation, fatigue, and joint pain.
Sores in the nose/mouth (often painless): Painless ulcers in the oral or nasal mucosa are a common feature during lupus flares and may go unnoticed unless carefully examined.
Alopecia (Hair loss): Hair may thin gradually or fall out in patches due to lupus activity or associated stress. Inflammatory scalp lesions may also cause scarring alopecia.
Weight loss: Unintentional weight loss may occur due to chronic inflammation, reduced appetite, nausea, or side effects of medications used to treat lupus.
Lymphadenopathy (Swollen lymph nodes): Enlarged lymph nodes in lupus can indicate immune system activation or inflammation, and they can be generalized or localized.
Abdominal pain, nausea, vomiting: These symptoms may result from gastrointestinal involvement in lupus (e.g., lupus enteritis, mesenteric vasculitis) or medication side effects.
Systemic Lupus Erythematosus Causes
The exact cause of lupus remains unknown. However, it may result from a combination of genetic predisposition, environmental triggers, hormonal influences, and immune system dysfunction. Lupus or systemic lupus erythematosus causes include:
- Genetic Factors
- Environmental Factors
- Hormonal Factors
- Medicines
- Immune system dysfunction
Genetic Factors: Some individuals have genetic variations that increase their risk of developing lupus. While it can run in families, most people inherit only the risk of the disease, not lupus itself.
Environmental Factors: Sunlight (ultraviolet light), infections (viral or bacterial), exposure to certain chemicals like silica dust or pesticides, and smoking can act as triggers for lupus in individuals who are genetically predisposed.
Hormonal Factors: Lupus occurs more frequently in women, particularly during their reproductive years, indicating that hormones may play a role in the development of the disease.
Medicines: Certain drugs, such as some blood pressure medications, anti-seizure drugs, and antibiotics, can cause lupus-like symptoms. This condition is known as drug-induced lupus and typically resolves once the medication is discontinued.
Immune system dysfunction: The impaired removal of dead or damaged cells can provoke an abnormal immune response, causing the immune system to mistakenly attack the body's own tissues.
Systemic Lupus Erythematosus Risk Factors
Lupus is more common in women aged 15–45 and in certain ethnic groups. Family history, infections, sunlight, some medications, and smoking can also increase the risk. The following are the lupus or systemic lupus erythematosus risk factors:
- Family History
- Genes and Gender
- Age
- Race
- Environmental factors
- Medical history
- Hormonal factors
- Psychosocial factors
Family History: People with a family history of lupus are at higher risk of developing the condition. However, the chance of a child developing lupus from a mother with the disease is low, around 2%.
Genes and Gender: Although lupus can affect anyone, it predominantly occurs in women, who are 9 to 10 times more likely to develop the condition than men.
Age: While lupus can affect people of all ages, it most often begins in early adulthood. The majority of individuals are diagnosed between the ages of 20 and 40, when the immune system is most active and functioning optimally.
Race: African American women are two to three times more susceptible than Caucasian women to having lupus. Additionally, Native American, Asian, and Hispanic women are more likely to have it. Women of Hispanic and African American descent are more prone to suffer from severe forms of lupus.
Some other possible lupus risk factors include:
- Environmental factors
- Medical history
- Hormonal factors
- Hormonal factors
- Psychosocial factors
Environmental factors: Exposure to toxins (like pesticides), heavy metals (such as lead and cadmium), smoking, and eating ultra-processed foods may increase the risk of lupus.
Medical history: Having other health conditions that cause inflammation or being infected with certain viruses can raise the risk of developing lupus.
Hormonal factors: Certain hormones present after menopause may increase the risk of lupus.
Psychosocial factors: Depression, lack of sleep, childhood abuse, and post-traumatic stress disorder can also contribute to lupus risk.
Lupus Complications
Complications in patients with lupus can arise either from direct organ damage caused by the disease itself or from the side effects of the medications used in its treatment. The following are the complications of systemic lupus erythematosus:
- Disease-related complications
- Kidney Complications (Lupus Nephritis)
- Hematological Complications
- Cardiovascular Complications
- Pulmonary Complications
- Neurological Complications
- Bone and Musculoskeletal Issues
- Eye Problems
- Pregnancy Complications
- Increased Infection Risk
- Treatment-related complications
- Long-term steroid use
- Immunomodulatory medications
- Immunosuppression
- Infection risk
Disease-related complications
Kidney Complications (Lupus Nephritis): Lupus causes kidney damage, which is one of its most serious outcomes. Immune system attacks on the kidneys induce inflammation, which can lead to renal damage and possibly kidney failure, requiring dialysis or transplantation.
Hematological Complications: Lupus can cause blood abnormalities such as anemia (low red blood cells), leukopenia (low white blood cells), thrombocytopenia (low platelets), and blood clots in arteries or veins, which increase the risk of bleeding or clotting.
Cardiovascular Complications: Inflammation from lupus can affect the heart muscle (myocarditis), the lining around the heart (pericarditis), and heart valves, leading to increased risks for heart disease, atherosclerosis, and heart attacks.
Pulmonary Complications: The lungs and their linings may be inflamed, resulting in pleurisy (painful inflammation of the chest cavity lining), pleural effusion, pulmonary hypertension, lung tissue damage, or acute pneumonitis, which can be life-threatening.
Neurological Complications: Lupus involvement in the nervous system may cause headaches, seizures, strokes, cognitive impairment, and behaviour changes due to inflammation or vascular injury in the brain and central nervous system.
Bone and Musculoskeletal Issues: These include osteoporosis and increased fracture risk, frequently linked to long-term corticosteroid therapy, as well as arthritis and joint inflammation common in lupus patients.
Eye Problems: Many individuals develop dry eyes, retinal vasculitis, optic nerve inflammation, or side effects from drugs such as disease-modifying antirheumatic drug (DMARD), which can cause retinal damage.
Pregnancy Complications: Lupus raises the risk of miscarriage, preterm birth, preeclampsia, and neonatal lupus due to autoantibodies affecting the fetus. Careful management during pregnancy is crucial.
Increased Infection Risk: Lupus patients are more susceptible to infections because of the disease itself and immunosuppressive therapies.
Treatment-related complications
Long-term steroid use: Leads to bone weakening (osteoporosis), fractures, tissue death (avascular necrosis), eye conditions (glaucoma, cataracts), weight gain, worsened diabetes control, increased infection risk, and possible psychiatric effects.
Immunomodulatory medications: May cause rare but serious side effects like irreversible eye damage and increased risk of certain cancers.
Immunosuppression: General increased susceptibility to infections due to weakened immune defenses.
Infection risk: Immunosuppression from both SLE and its treatments significantly raises the risk of infections, a major cause of illness and mortality in these patients.
Systemic Lupus Erythematosus Diagnosis
Lupus can be challenging to diagnose because its symptoms often fluctuate and may resemble those of other conditions. It's important to mention all symptoms, even those that have already been resolved. The following tests are used in the process of lupus or systemic lupus erythematosus diagnosis:
- Clinical assessment
- Medical history and family history
- Physical examination
- Laboratory test
- Antinuclear antibodies (ANA) testing
- Additional antibody testing if ANA is positive includes
- Antiphospholipid antibodies
- Anti-smith antibodies
- Anti-double-strand DNA antibodies
- Complement tests (C3 and C4)
- Complete blood counts(CBC)
- Kidney function tests
- Liver function tests
- Urinalysis
- Urine protein-to-creatinine ratio
- C-reactive protein (CRP)
- Erythrocyte sedimentation rate (ESR)
- Imaging tests
- Computed tomography (CT) or, Magnetic resonance imaging (MRI)
- Chest X-rays
- Tissue Biopsies
- Skin biopsy
- Kidney biopsy
Lupus Treatment
Lupus is a chronic (long-lasting) disease with no cure currently available. However, treatment options have greatly improved, offering more ways to manage the condition. Since symptoms can vary and treatments may cause side effects, a combination of therapies is often recommended to control lupus effectively. The following are systemic lupus erythematosus treatment options:
- Nonpharmacological treatment
- Pharmacological treatment
- Antimalarials
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Corticosteroids
- Immunosuppressive drugs
- Biologic agents
- Other treatments for lupus-related complications
- Drugs for osteoporosis
- Antibiotics for infections
- Antihypertensive drugs for high blood pressure
- Statins for high cholesterol
- Anticonvulsants for seizures
- Vitamin D to help improve kidney function in lupus
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
Lupus Prevention
Although lupus (Systemic lupus erythematosus) cannot be fully prevented, flares can be managed by avoiding triggers like sun exposure, controlling stress, maintaining a healthy lifestyle, and following medical advice. The following measures are recommended for lupus or systemic lupus erythematosus prevention:
- Recognising early warning signs of a flare
- Maintaining a healthy, balanced diet
- Engaging in regular exercise
- Avoiding smoking
- Minimizing sun exposure
- Participating in support groups
- Maintaining open communication with family and friends
- Seeking assistance during increased symptom
- Including leisure activities for relaxation
- Managing stress actively
- Implementing workplace changes
Recognizing early warning signs of a flare: Identifying symptoms like increased fatigue, joint pain, rashes, or fever early helps in seeking prompt treatment to prevent severe complications.
Maintaining a healthy, balanced diet: A nutritious diet supports the immune system, helps manage weight, and reduces inflammation, which is important for controlling lupus symptoms.
Engaging in regular exercise: Moderate physical activity improves joint flexibility, reduces fatigue, and boosts overall well-being without overexerting the body.
Avoiding smoking: Smoking can worsen lupus symptoms, increase cardiovascular risk, and reduce the effectiveness of certain medications.
Minimizing sun exposure: Ultraviolet light often triggers lupus skin rashes and flares, so protecting the skin with sunscreen and clothing is important.
Participating in support groups: Connecting with others who have lupus provides emotional support, practical advice, and helps reduce feelings of isolation.
Maintaining open communication with family and friend: Sharing your experience helps build a support network, making it easier to manage daily challenges and emotional stress.
Seeking assistance during increased symptoms: Seeking prompt medical attention during lupus flare-ups can reduce symptom severity and prevent complications. Early intervention promotes faster recovery and helps protect organ function.
Including leisure activities for relaxation: Participating in hobbies lowers stress levels, which are known to provoke lupus flare-ups. Reducing stress through enjoyable activities can enhance well-being and lessen the impact of symptoms.
Managing stress actively: Stress negatively impacts the immune system and can provoke flares, so techniques like mindfulness, meditation, or counseling are beneficial.
Implementing workplace changes: Adjustments such as flexible hours or ergonomic equipment help manage fatigue and joint pain, enabling continued work despite symptoms.
Frequently Asked Questions (FAQs) on Lupus
Can lupus be cured?
No, lupus cannot be cured. However, it is manageable through a combination of medical treatments and lifestyle adjustments. Treatment strategies focus on controlling inflammation, relieving symptoms, and preventing flares. With regular medical follow-up, adherence to prescribed therapies, and healthy lifestyle practices, most people with lupus can achieve a good quality of life and carry out daily activities with minimal restrictions.
What is usually the first sign of lupus?
The earliest signs of lupus commonly include persistent fatigue, low-grade fever, and joint pain or stiffness. One of the main symptoms is a rash that resembles a butterfly and covers the nose and cheeks. Skin sensitivity to sunlight and Raynaud's phenomenon, in which fingers or toes change color in cold weather, could be additional early warning signs. Early diagnosis is difficult because these symptoms might vary greatly and manifest gradually.
Is lupus hereditary?
Lupus is not directly inherited, but genetic factors can increase susceptibility to the condition. Its development often requires environmental triggers such as infections, stress, or sun exposure. As an autoimmune disorder, lupus causes the immune system to mistakenly attack healthy tissues.
Is lupus contagious?
No, lupus is not a contagious disease and cannot be transmitted from person to person through any form of contact, including sexual interaction or close physical proximity. It is a chronic autoimmune condition in which the body’s immune system mistakenly targets and attacks its healthy tissues. Unlike infectious diseases, lupus is caused by a combination of genetic, environmental, and hormonal factors, not by exposure to a virus or bacteria.
Is lupus cancer?
No, lupus is not cancer. It is a chronic autoimmune illness in which the immune system mistakenly targets the body's healthy tissues and organs. Cancer, on the other hand, is defined by the uncontrolled proliferation and spread of abnormal cells. However, people with lupus may have a slightly higher risk of acquiring certain types of cancer, which is frequently connected to persistent inflammation or the use of immunosuppressive medicines.
How to treat a lupus flare?
Lupus flares are treated with a combination of medications, lifestyle adjustments, and ongoing monitoring. Immunosuppressants, NSAIDs, antimalarials, and corticosteroids are commonly used drugs to treat inflammation. Lifestyle changes, such as getting adequate sleep, reducing stress, and using sunscreen, are essential. Together, these strategies help to lessen the frequency of flares while improving overall health.
Is lupus chronic?
Yes, lupus is a long-term autoimmune disorder that persists over time and requires consistent medical care. It occurs when the immune system unintentionally targets healthy tissues, causing inflammation and discomfort that can spread throughout the body.
How is lupus diagnosed?
Diagnosing lupus is a complex process which involves evaluating a patient's medical history, performing a physical examination, and conducting various laboratory and imaging tests. No single diagnostic test can definitively confirm the condition; a diagnosis is made based on a combination of test results and the observation of symptoms over time.
Does lupus weaken your immune system?
Yes, lupus can weaken the immune system. As an autoimmune condition, it causes the immune system to unintentionally target the body's tissues, resulting in inflammation and potential damage to various organs, including the skin, joints, kidneys, lungs, and heart. Moreover, medications commonly used to treat lupus, including immunosuppressants, are designed to reduce immune activity, which can increase susceptibility to infections.
Is lupus life-threatening?
Yes, lupus can be life-threatening in certain cases, specifically when it involves critical organs such as the kidneys, heart, or brain. However, with early diagnosis, appropriate medical care, and ongoing treatment, many individuals with lupus are able to lead long, active, and fulfilling lives.
What is the difference between lupus and rheumatoid arthritis?
Lupus is a systemic autoimmune illness affecting multiple organs, including the skin, kidneys, and brain. The symptoms are tiredness, a butterfly-shaped rash, and photosensitivity. In contrast, rheumatoid arthritis is largely a joint illness that results in symmetrical pain, swelling, and deformity over time. While both conditions can induce joint discomfort, lupus is more likely to cause non-deforming arthritis, whereas RA causes gradual joint degeneration. Lupus and RA are both autoimmune disorders, although lupus affects many organ systems whereas RA affects only the joints.
How long do lupus mouth sores last?
Although they may last longer during severe flare-ups, mouth sores or ulcers associated with lupus often recover within one to two weeks with proper treatment. An evaluation by a rheumatologist or oral medicine expert is recommended if a sore persists for longer than three weeks in order to ensure appropriate care and to rule out any underlying illnesses or disorders. Often found on the roof of the mouth, inside the cheeks, or along the gums, these ulcers can be either painful or painless, and Lupus flare-ups can sometimes be detected early.
Can one have lupus with a negative ana test?
Yes, it is possible to have antinuclear antibody (ANA) negative lupus, although it is uncommon. While a positive antinuclear antibody (ANA) test is typically associated with systemic lupus erythematosus (SLE), some people may still be diagnosed with lupus despite a negative ANA result, particularly if clinical symptoms and other laboratory findings support the diagnosis.
Does smoking cause lupus flares?
Yes, smoking can exacerbate lupus and increase the frequency of flare-ups. It has been demonstrated to worsen pre-existing symptoms, particularly skin signs and general disease activity, and raise the likelihood of developing lupus. One of the most significant lifestyle adjustments a person with lupus can make to enhance their health and manage their condition is to quit smoking.
When to consult a doctor for lupus?
Consult a doctor for lupus if symptoms persist, worsen, or begin to interfere with daily life. Early diagnosis and treatment are important to prevent long-term damage. Signs that need attention include:
- Persistent fatigue not relieved by rest
- Joint pain or swelling, especially with morning stiffness
- Skin rashes, particularly a butterfly-shaped rash across the cheeks and nose
- Sensitivity to sunlight
- Unexplained fever or weight loss
- Chest pain or shortness of breath
- Hair loss or sores in the mouth or nose
- Swelling in the legs or around the eyes
- Fingers or toes turning white or blue colour in the cold (Raynaud’s phenomenon)
If these symptoms continue, it is important to consult a rheumatologist who can evaluate the cause and recommend the right treatment plan. Seek emergency medical attention if you experience seizures, sudden confusion, severe chest pain, or difficulty breathing, which could suggest serious complications. A rheumatologist, general care physician, or specialist can provide the best lupus treatment to control the disease and prevent complications.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868