Successful Total Knee Replacement (TKR) for Osteoarthritis in a 57-Year-Old Woman
PACE Hospitals
PACE Hospitals' expert Orthopaedic team successfully performed a total left knee replacement (TKR) surgery on a 57-year-old female patient who presented with pain and swelling in the left knee for the past few months. Surgery was performed to relieve the symptoms of pain and swelling in the left knee, prevent further complications and enhance the patient’s mobility and quality of life.
Chief Complaints
A 57-year-old female patient with a
body mass index (BMI) of 22 presented to the Orthopaedics Department at
PACE Hospitals, Hitech City, Hyderabad, with the chief complaints of pain and swelling in the left knee for a few months, which had started to interfere with her daily activities and mobility.
Past Medical History
The patient had no known history of drug allergies or chronic illnesses. The absence of comorbid conditions was considered clinically favourable, as it minimized the risk of intraoperative and postoperative complications and supported a smoother, more stable recovery.
On Examination
Upon admission to PACE Hospitals, the patient was hemodynamically stable. The respiratory system showed bilateral air entry, the cardiovascular system had audible S1 and S2 heart sounds, the abdomen was soft and non-tender, and the central nervous system examination indicated that the patient was alert, conscious, and oriented to time, place, and person.
Systemic examination revealed the evidence of effusion and tenderness along the medial joint line. A fixed flexion deformity of 15 degrees was noted. The range of motion of the left knee was painfully restricted. No distal neurovascular deficit (DNVD) was observed.
Diagnosis
Following the examination, the Orthopaedic team performed a comprehensive assessment, which included a thorough review of the patient’s medical history and clinical findings. Based on characteristic symptoms such as pain and swelling in the left knee persisting over the past few months, a provisional diagnosis of osteoarthritis of the left knee was made.
To support the clinical findings, laboratory tests and imaging studies were undertaken. X-rays of the left knee, including anteroposterior (AP), lateral, and oblique views, revealed changes consistent with osteoarthritis. These radiographic findings correlated with the patient’s symptoms and confirmed the provisional diagnosis, guiding the team toward planning an appropriate surgical intervention.
Based on the confirmed diagnosis, she was advised to undergo osteoarthritis treatment in Hyderabad, India, under the care of the Orthopaedic Department, ensuring comprehensive management.
Medical Decision Making (MDM)
Following a detailed discussion with the patient and her guardians, Dr. Raghuram, Consultant Orthopaedic Surgeon, recommended total knee replacement as the most appropriate and effective treatment to achieve optimal stabilization and promote recovery.
Given the patient’s symptoms, functional limitations in daily activities, and the confirmed diagnosis of osteoarthritis of the left knee, surgical intervention was considered essential.
The patient and her family were thoroughly counseled regarding the nature of the condition, the surgical procedure, potential risks, and the necessity of total knee replacement to restore function and stabilize the left knee.
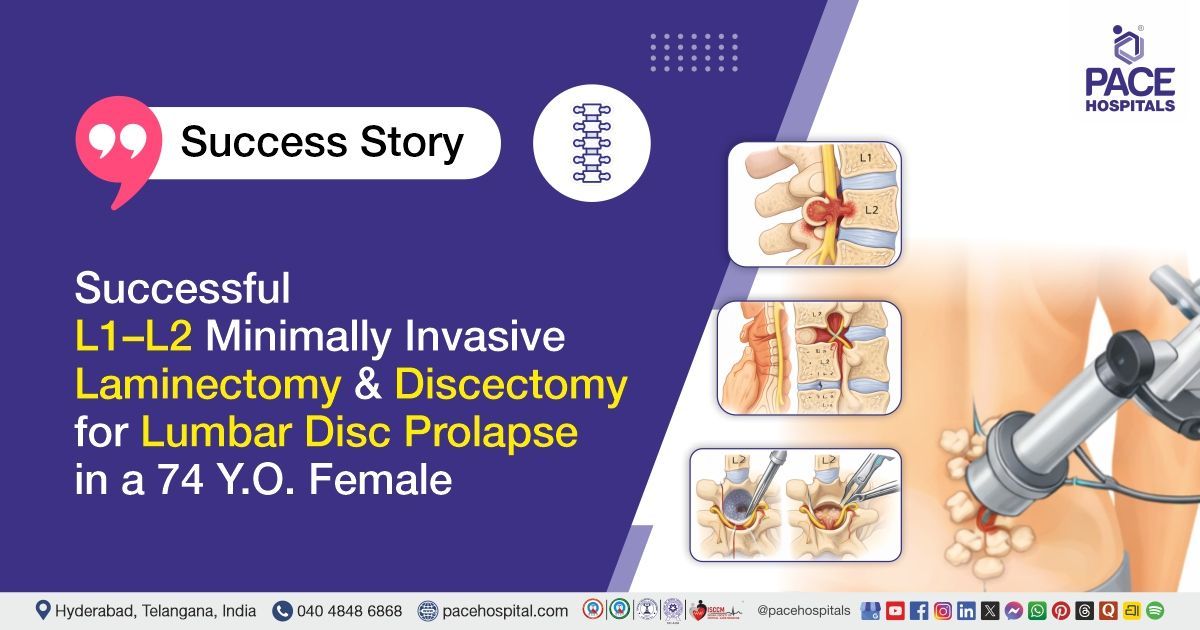
Surgical Procedure
Following the decision, the patient was scheduled to undergo Left-Sided Total Knee Replacement Surgery in Hyderabad at PACE Hospitals, under the supervision of the expert orthopaedic Department.
The following steps were carried out during the procedure:
- Preoperative Preparation and Anesthesia: The patient underwent preoperative evaluation and was cleared for surgery. Spinal anesthesia was administered, and the patient was positioned appropriately with a tourniquet applied.
- Surgical Exposure: A midline incision was made over the left knee, followed by a medial parapatellar arthrotomy to expose the joint surfaces.
- Resection of Damaged Tissue: The diseased cartilage and underlying bone from the femur, tibia, and patella were removed. The bone surfaces were shaped to accommodate the prosthetic components.
- Implantation of Prosthetic Components: Trial components were used to confirm alignment and function. Once satisfactory, the final components were implanted using bone cement. Patellar resurfacing was performed as needed.
- Closure and Postoperative Care: Hemostasis was achieved, the joint was irrigated, and the wound was closed in layers over a drain. A sterile dressing was applied, and the patient was transferred to recovery in stable condition.
Postoperative Care
The postoperative period was uneventful. The patient was mobilized early and encouraged to walk with support during the hospital stay under supervision. She had received intravenous antibiotics, analgesics, and supportive treatment. Wound dressings were performed regularly and had remained clean and dry, with no signs of infection. At the time of discharge, the patient was hemodynamically stable without pain, and the surgical site had appeared healthy.
Discharge Medication
Upon discharge, the patient was prescribed a comprehensive medication regimen tailored to support postoperative recovery and prevent complications. This included a course of antibiotics to reduce the risk of surgical site infection, analgesics for effective pain management, and proton pump inhibitors (PPIs) to prevent gastrointestinal irritation associated with analgesic use.
In addition, antiplatelet agents were prescribed to reduce the risk of thromboembolic events during the postoperative period. Multivitamin supplements were included to support overall healing and recovery. Additional supportive treatments, including physiotherapy and limb elevation, were also advised as part of the post-discharge care plan.
Advice on Discharge
The patient was advised to follow a normal & balanced diet. Physiotherapy included walking and staircase training for one week to improve mobility, strength, and functional independence following total knee replacement.
Emergency Care
The patient was informed to contact the Emergency ward at PACE Hospitals in case of any emergency or development of symptoms such as fever, abdominal pain, and vomiting.
Review and Follow-Up
The patient was advised to return for a follow-up visit with the Orthopaedic Department at PACE Hospitals after one week for a dressing change and further evaluation.
Conclusion
This case highlights the effectiveness of total knee replacement (TKR) surgery in restoring knee alignment and function, reducing pain, and improving quality of life in patients with severe osteoarthritis, enabling a return to daily activities after recovery.
Significance of X ray (plain Radiographs) in diagnosing and management of Osteoarthritis
The predominant test done in osteoarthritis is a plain X-ray (radiograph). Plain radiographs are the most widely used by orthopaedic doctor / orthopaedic surgeon in imaging modality because they are widely available, low-cost, and can detect key features of osteoarthritis, such as joint space narrowing, osteophytes (bone spurs), subchondral cysts, and sclerosis. Although X-rays may not be sensitive to early disease and do not assess soft tissues, they remain the standard for confirming and evaluating the severity of osteoarthritis in clinical practice.
However, some guidelines recommend that osteoarthritis should be diagnosed clinically whenever possible, and routine imaging is not always necessary, especially in early or uncomplicated cases. Despite this, plain X-rays are still widely used for initial evaluation and assessment of disease severity.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868