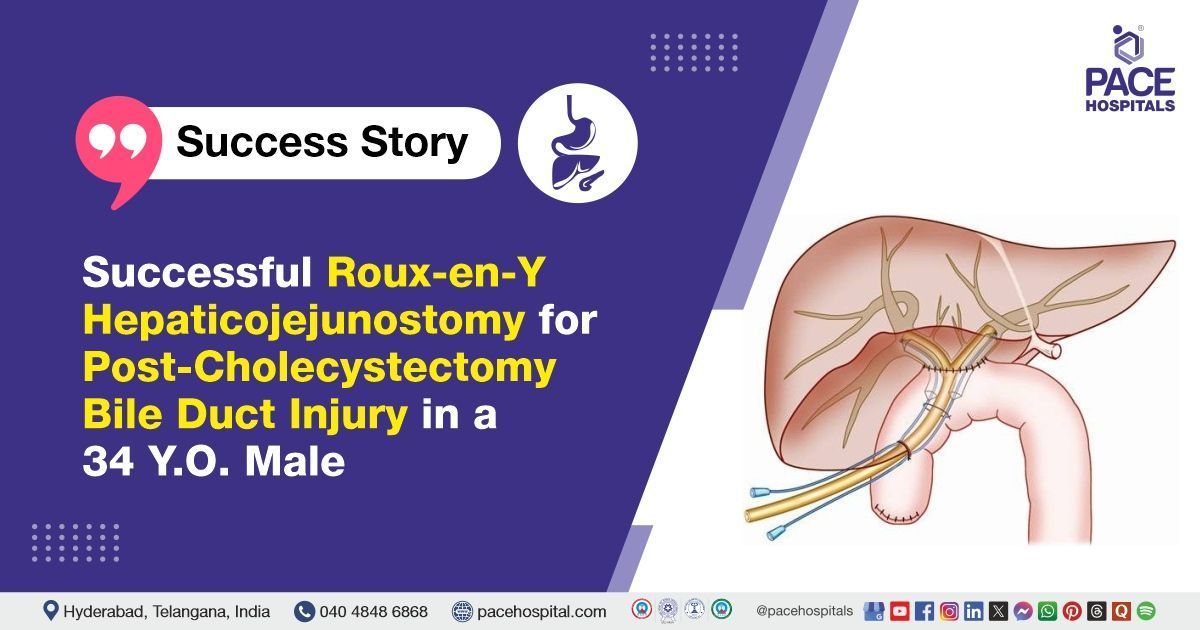
Successful Roux-en-Y Hepaticojejunostomy for Post-Cholecystectomy Bile Duct Injury in a 34 Y.O. Male
PACE Hospitals
PACE Hospitals’ expert Surgical Gastroenterology team successfully performed a Roux-en-Y Hepaticojejunostomy with Jejunojejunostomy (JJ) on a 34-year-old male patient diagnosed with a Type 2 benign biliary stricture following a post-cholecystectomy bile duct injury. The aim of the procedure was to restore normal bile flow by connecting the hepatic duct to the jejunum, bypassing the stricture site. This standard surgical approach helps relieve symptoms, prevent infections, and preserve long-term liver function.
Chief Complaints
A 34-year-old male with a body mass index (BMI) of 20 presented to the Surgical Gastroenterology Department at PACE Hospitals, Hitech City, Hyderabad, with a chief complaint of jaundice persisting for one month.
Past Medical History
The patient had a history of a
laparoscopic cholecystectomy in the past, following which he developed a postoperative collection that required percutaneous catheter drainage (PCD). He had no prior history of similar complaints. A Magnetic Resonance Cholangiopancreatography (MRCP) was performed, which was suggestive of a Type 2 benign biliary stricture.
On Examination
On physical examination, the patient was conscious, coherent, and oriented with stable vital signs. A systemic examination, including an abdominal assessment, revealed mild tenderness in the right upper quadrant with a healed surgical scar. The abdomen was soft, with no palpable masses, guarding, or rigidity. Bowel sounds were present and normal. There were no signs of acute gastrointestinal distress, and the findings were consistent with his overall clinical stability.
Diagnosis
Upon admission to PACE Hospitals, the patient was thoroughly evaluated by the Surgical Gastroenterology team, which included a clinical examination and a one-month history of progressive jaundice following laparoscopic cholecystectomy. There was a strong clinical suspicion of a post-cholecystectomy bile duct injury leading to a benign biliary stricture.
The patient underwent a comprehensive diagnostic evaluation for jaundice. Magnetic Resonance Cholangiopancreatography (MRCP) revealed a Type 2 benign biliary stricture. The clinical history also included a postoperative bile collection, for which percutaneous catheter drainage (PCD) had been performed. Routine blood investigations showed abnormal liver function tests suggestive of cholestasis. Chest X-ray findings were normal, and fluid culture from the drain showed no bacterial growth.
Based on the confirmed diagnosis, the patient was advised to undergo
Benign Biliary Stricture (Type-2) Treatment in Hyderabad, India, under the expert care of the Surgical Gastroenterology Department.
Medical Decision-Making (MDM)
After a detailed consultation with Dr. Suresh Kumar S, Surgical Gastroenterologist, and cross consultations with Dr. Pradeep Kiran Panchadi, Consultant Interventional Pulmonologist, a thorough evaluation was conducted considering the patient’s complaints of jaundice, history of laparoscopic cholecystectomy complicated by bile duct injury, and subsequent biliary stricture confirmed on MRCP.
Given the patient’s clinical condition and anatomical findings, it was determined that Roux-en-Y hepaticojejunostomy with jejunojejunostomy was identified as the most appropriate surgical intervention to restore biliary drainage and prevent further complications.
The patient and his family members were counselled regarding the diagnosis, the planned surgical procedure, its associated risks, and its potential to relieve symptoms and improve quality of life.
Surgical Procedure
Following the decision, the patient was scheduled to undergo Roux-en-Y Hepaticojejunostomy with jejunojejunostomy surgery in Hyderabad at PACE Hospitals, under the expert supervision of the Surgical Gastroenterology Department.
The following steps were carried out during the procedure:
- Incision and Exposure: A right subcostal incision was made to gain access to the operative field. Dense omental adhesions were identified and carefully dissected between the liver, omentum, stomach, and colon to provide adequate exposure.
- Identification of Bile Duct and Hilar Dissection: The bile duct was located close to the hepatic hilum. The hilar plate was carefully lowered to facilitate access to the biliary structures.
- Resection of Segment 4 Base: The hanging part of the base of segment 4 of the liver was removed to improve exposure and allow for a tension-free anastomosis.
- Choledochotomy: A choledochotomy approximately 2.5 cm in length was performed, extending proximally to the left hepatic duct (LHD) to prepare the bile duct for anastomosis.
- Creation of Roux Limb and Hepaticojejunostomy: A Roux limb of jejunum was created and brought up to the hepatic duct. A hepaticojejunostomy was then performed in an interrupted suture manner, ensuring a secure biliary-enteric anastomosis.
Postoperative Care
The procedure was uneventful, and the patient’s postoperative recovery was satisfactory. During the hospital stay, he received treatment with intravenous fluids, intravenous antibiotics, and other supportive medications. At the time of discharge, the patient was hemodynamically stable and provided with the following advice.
Discharge Medications
Upon discharge, the patient was prescribed a course of proton pump inhibitors to reduce gastric acid secretion and promote gastrointestinal healing. Extended-release prokinetic agents were given to improve gastrointestinal motility. For pain management, nonsteroidal anti-inflammatory drugs (NSAIDs) were administered to control postoperative discomfort. A bulk-forming laxative was provided to facilitate regular bowel movements and prevent constipation. Additionally, hepatoprotective medication was prescribed to support liver function during recovery.
Advice on Discharge
Upon discharge, the patient was advised to follow a liquid diet with occasional soft foods to ensure ease of digestion and minimize strain on the surgical site. Instructions regarding drain care were provided, emphasizing proper hygiene and monitoring for any signs of infection or complications.
Emergency Care
The patient was informed to contact the emergency ward at PACE Hospitals in case of any emergency or development of symptoms such as fever, abdominal pain and vomiting.
Review and Follow-up Notes
The patient was advised to return for a follow-up visit with the Surgical Gastroenterologist in Hyderabad at PACE Hospitals, after 5 days, for further evaluation.
Conclusion
This case highlights the successful management of a benign biliary stricture following a post-cholecystectomy bile duct injury. The patient underwent Roux-en-Y hepaticojejunostomy with a favourable postoperative recovery. Early surgical intervention and multidisciplinary care were crucial in restoring biliary drainage and improving the patient’s quality of life.
Importance of Early Surgical Intervention in Post-Cholecystectomy Bile Duct Injuries
Timely diagnosis and surgical management are crucial in patients with benign biliary strictures resulting from bile duct injuries sustained during cholecystectomy. Early recognition and appropriate reconstructive procedures, such as Roux-en-Y hepaticojejunostomy, help prevent serious long-term complications like cholangitis, biliary cirrhosis, and liver failure. A multidisciplinary approach involving a surgical Gastroenterologist / Surgical gastroenterology doctor, radiologists, and critical care teams ensures comprehensive and patient-specific care.
Meticulous surgical technique during cholecystectomy is essential to minimize the risk of bile duct injury. Postoperative monitoring and supportive therapy play a vital role in optimizing recovery and outcomes. Additionally, patient education and regular follow-up are important to promptly identify and manage any potential complications.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles