Transition from Haemodialysis to Peritoneal Dialysis in an ESRD Patient | Case study
PACE Hospitals
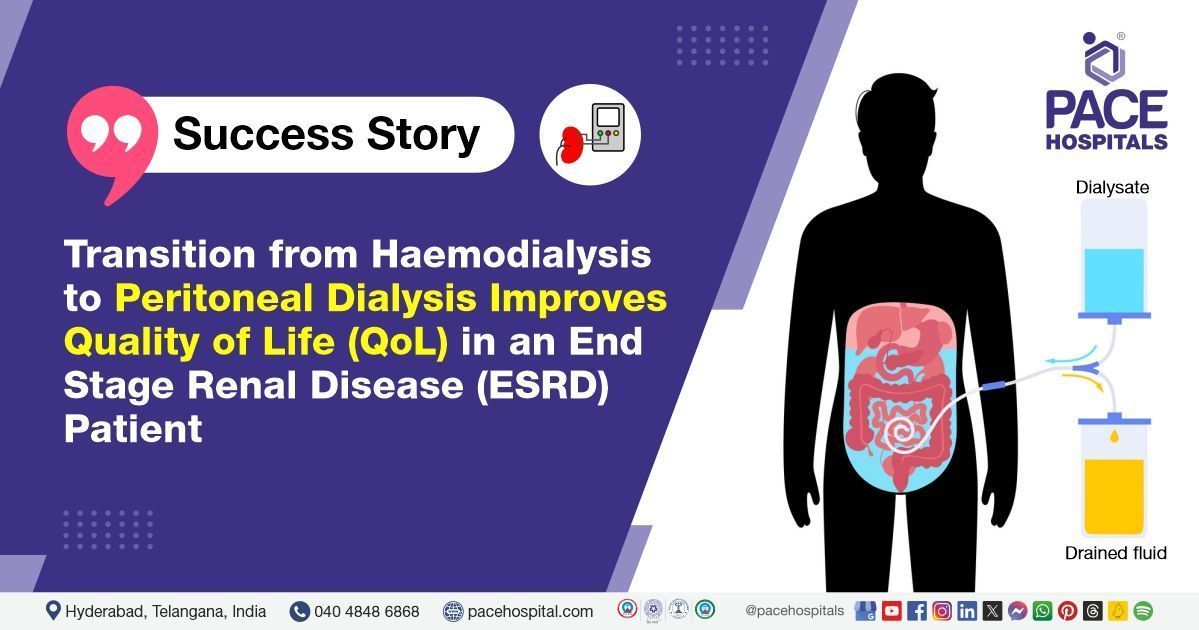
The nephrology and renal transplantation experts’ team from PACE Hospitals successfully performed peritoneal dialysis catheter insertion in a 68-year- old adult male patient with chronic kidney disease, stage-V (End stage renal disease).
Chief Compliant
A 68-year-old adult male (BMI 21.8 kg/m²) with
chronic kidney disease (CKD) stage V, undergoing maintenance haemodialysis (a procedure that cleans the blood using a dialysis machine and a special filter called a dialyzer), was referred to
PACE Hospitals, Hyderabad, for
peritoneal dialysis catheter insertion.
Medical History and Diagnosis
Upon profound examination, it was realized that the patient is a known case of chronic kidney disease stage-V (end-stage chronic kidney disease) along with other co-morbidities like diabetes mellitus type II, hypertension, and coronary artery disease. The patient has been on haemodialysis as a complementary treatment method of renal replacement therapy (kidney transplantation). Delving more into his dialysis plan, it is understood that he has been subjected to haemodialysis weekly once through an internal jugular vein permcath, at a hospital facility specializing in renal care, similar to centers known for Chronic Kidney Cancer Treatment in Hyderabad, India.
After considering the patient related health determinants, and lifestyle, Consultant Nephrologist and Renal Transplant Physician, Dr. A Kishore Kumar, Senior Consultant Urologist & Renal Transplant Surgeon, Dr. Vishwambhar Nath, Consultant Laparoscopic Urologists, Dr. Abhik Debnath and Dr. K Ravichandra from PACE Hospitals have ascertained to switch the patient from haemodialysis-hospital facility to peritoneal dialysis by catheter insertion.
Following the decision, the patient was scheduled for a
Peritoneal Dialysis Catheter Placement in Hyderabad at PACE Hospitals, under the expert supervision of the Nephrology Department.
Preparation for the procedure
The patient was admitted for peritoneal dialysis catheter insertion. Baseline investigations like complete blood picture, serum electrolytes, creatinine,
liver function tests were done.
Ultrasonogram (USG) abdomen is performed to rule out any intra-abdominal mass. The imaging test did not reveal any such mass or adhesions. The patient was given a single dose of glycopeptide antibiotic before performing the procedure.
Procedure
Peritoneal dialysis catheter insertion was done in operation theater under fluoroscopy (a technique used to differentiate between tissues and helps in the accuracy of a procedure) and local anesthesia. The abdomen was draped and cleaned with Betadine, and amino amide class local anesthesia was given 2cm below the umbilicus. A 2 cm incision was made on the skin below the umbilicus and tissues were separated until rectus sheath was exposed. With an intravenous needle, the linea alba was pricked, and the peritoneal cavity was entered. Upon having access to the peritoneal cavity, 500 ml of normal saline was instilled. The position of the needle was confirmed to be in the peritoneum with the help of contrast fluoroscopy. A Guide wire was inserted under guidance and the peritoneal dialysis catheter was inserted with a peel away sheath. Flow was checked, and a tunnel was created for exit on the left side of the abdomen, with the exit facing inferolateral below the belt line. The inner cuff of the peritoneal dialysis catheter was secured to rectus sheath and subcutaneous tissue was closed with absorbable sutures and skin was closed with proline. Dressing was done after achieving hemostasis.
Aftermath
The patient was shifted to the intensive care unit and observed post procedure. He underwent one session of haemodialysis with permcath. Next day the dressing was changed from the peritoneal dialysis catheter as it was soaked up with seepage of blood. He had a temperature of 99.8O F once and no further episodes of fever. Glycopeptide antibiotic was advised but patient developed reactions of tachypnea (rapid breathing) and shortness of breath, Then the antibiotic is discontinued and given antihistamines with steroids to improve the symptoms after injection. Erythropoiesis stimulating agents (helps in red blood cells production) are given to handle anemia of chronic kidney disease. He was discharged in stable condition, with advice to review after 5 days for dialysis and peritoneal dialysis catheter flushing.
Discharge notes
The patient is prescribed with antihypertensive drugs, diuretics, vasodilators, anti-platelets, and antipyretic medications. He was advised not to soak the peritoneal dialysis catheter dressing for 2 weeks. Water intake should be restricted to less than 1000ml per day, whereas salt intake should not be more than 5 grams/ day. Blood glucose levels should be monitored regularly.
The patient was instructed to contact PACE Hospitals in case of any emergency or development of symptoms like fever, abdominal pain, or vomiting. The patient was advised to return for a follow-up appointment with Nephrologists in Hyderabad at PACE Hospitals five days post-procedure. This follow-up aimed to evaluate the healing of the catheter insertion site, assess for any signs of infection or complications, and review the patient's adherence to postoperative care instructions, including fluid and dietary restrictions.
Conclusion
This case highlights how a tailored approach and expert care can lead to a smooth transition between dialysis modalities, resulting in better patient outcomes and improved quality of life.
Switch in dialysis procedure: All you should know about!
Dialysis is a medical procedure used to remove waste products and excess fluids from the blood when the kidneys are no longer able to perform this function effectively. It can be performed using various techniques, including haemodialysis and peritoneal dialysis.
Haemodialysis cleanses the blood using a dialysis machine and a special filter called a dialyzer (often referred to as an artificial kidney). In contrast, peritoneal dialysis filters the blood inside the body, using the lining of the abdomen (peritoneum) as a natural filter. While the goal of both dialysis techniques is similar, each method has its own advantages depending on the patient’s condition and preferences.
Switching from one type of dialysis to another is common among patients with end-stage renal disease (ESRD). This decision is often guided by a nephrologist, a specialist in kidney care, who evaluates the patient’s medical condition, lifestyle, and treatment goals. Some patients may prefer peritoneal dialysis for the convenience of home-based care, while others might opt for haemodialysis in a hospital setting under the supervision of trained medical staff.
In certain situations, a switch may be recommended due to technique failure (such as vascular access issues or infections) or evolving clinical needs. Compared to haemodialysis, peritoneal dialysis has shown benefits such as better haemodynamic stability, improved blood pressure control, enhanced clearance of molecular substances, and preservation of residual kidney function. These factors, when managed under the expert care of a
nephrologist/nephrology doctor, can significantly improve the patient’s overall quality of life.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles