Black Fungus Infection - Mucormycosis Disease: Causes, Symptoms, Diagnosis and Treatment
PACE Hospitals
Black fungus infection or Mucormycosis is a serious disease but rare fungal infection, it can become fatal. 50-80% of patients could die with it if not diagnosed and treated quickly at early stages. This usually occur in people when the immune system has been affected by Coronavirus (COVID-19), viral diseases, immunodeficiency disorders, cancers, chronic diseases, other medical conditions or people take medicines that suppress the immune system to fight illness.
Mucormycosis caused by fungi mucormycetes and molds belonging to the order mucorales are present in air throughout the environment, particularly in soil, decaying organic substrates, compost piles, animal dung, rotting wood and plant material. This can be easily observed as black colored growth on rotting fruits and old bread. Fungi play a very important role on Earth and required for healthy ecosystem, fungi evolved 400 million years ago. Fungi decompose organic litter and recycle the nutrients locked up in the leaves and wood.
Mucormycosis is a non-contagious disease, and it cannot transmit by direct or indirect contact between people or between people and animals. As per recent reports, 70% of the cases documented around the world related to mucormycosis (black fungus infections) associated with COVID-19 are in INDIA.
Fungi that are otherwise harmless but can take advantage of people with weakened immune system and invade tissues. This is why black fungus infections are also called as opportunistic Infections.
Mucor fungi produce millions of spores (dark-hued, microscopic spherical structures) that are disseminated in air. These spores when land on moist surfaces, like plant material, compost piles, animal dung or soil, they begin to germinate and produce thread like structures called mycelia. The mycelia branch out and feed on sugars in their surroundings and grow.
Fungal spores generally higher in summer than monsoon in INDIA. Outdoor around 800 to 4800 spores per cubic meter present compared to 80 to 280 spores per cubic meter inside house. Around 5 to 10 fungi species dispersed in the air.
What are the causes of Mucormycosis?
People get mucormycosis after inhaling fungal spores from the air through environment; cause lungs, brain or sinus infection whereas fungus enters through the damaged skin due to any type of skin injury to cause a skin infection.
Most of the people every day come in contact with microscopic fungal spores, so it’s highly impossible to keep ourselves away from mucormycetes. Generally these fungi aren’t harmful to most of the people. However, for people who have weakened immune systems, breathing in mucormycete fungi spores can cause an infection which can spread to other parts of the body and organs.
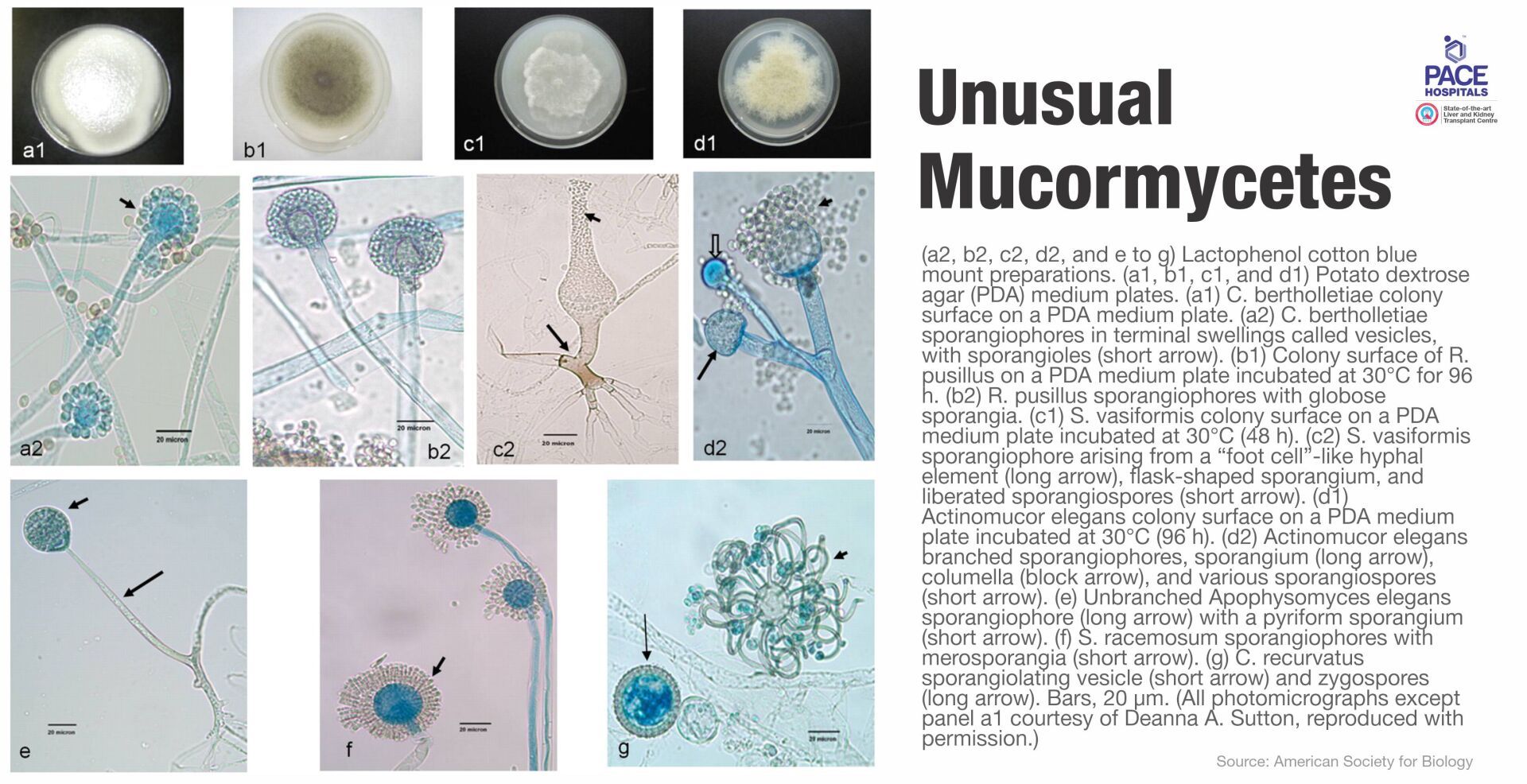
Rhizomucor, Mucor, Rhizopus, Cunninghamella bertholletiae, Saksenaea, Syncephalastrum, Apophysomyces, and Absidia fungi species commonly cause the infection.
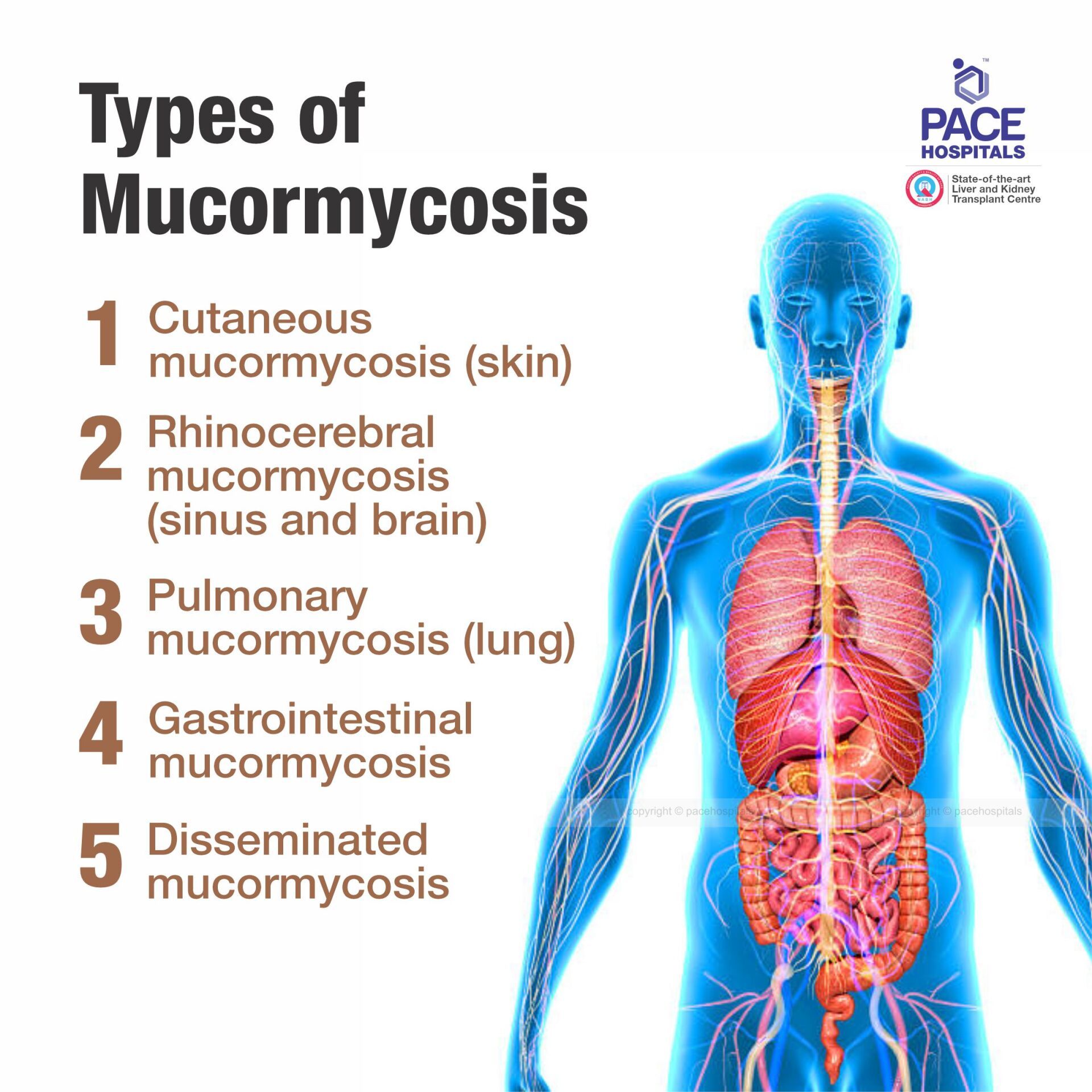
What are the types of Mucormycosis?
As per the research black fungal infection can spread in a body through bloodstream, infect body parts and organs.
- Pulmonary mucormycosis (lung) - It is the most common in patients with cancer and in patients who have had a stem cell transplant or an organ transplant.
- Rhinocerebral mucormycosis (sinus and brain) - It is the sinus's infection that can spread to the brain. This is most common in patients with uncontrolled diabetes and in patients who have had a kidney transplant.
- Cutaneous mucormycosis (skin) – It is the skin infection when fungi enter the body through damaged skin (due to surgery, severe burn or any type of skin injury). This is the most common among people who do not have weakened immune systems.
- Gastrointestinal mucormycosis - It is common among young children especially low birth weight and premature infants age less than 1 month, who have had surgery or on medications that lower the body’s ability to fight illness.
- Disseminated mucormycosis – It is the infection commonly affects the brain but when infection spreads through the bloodstream and can affect other body parts and organs such as heart, spleen and skin.
What are the symptoms of Mucormycosis?
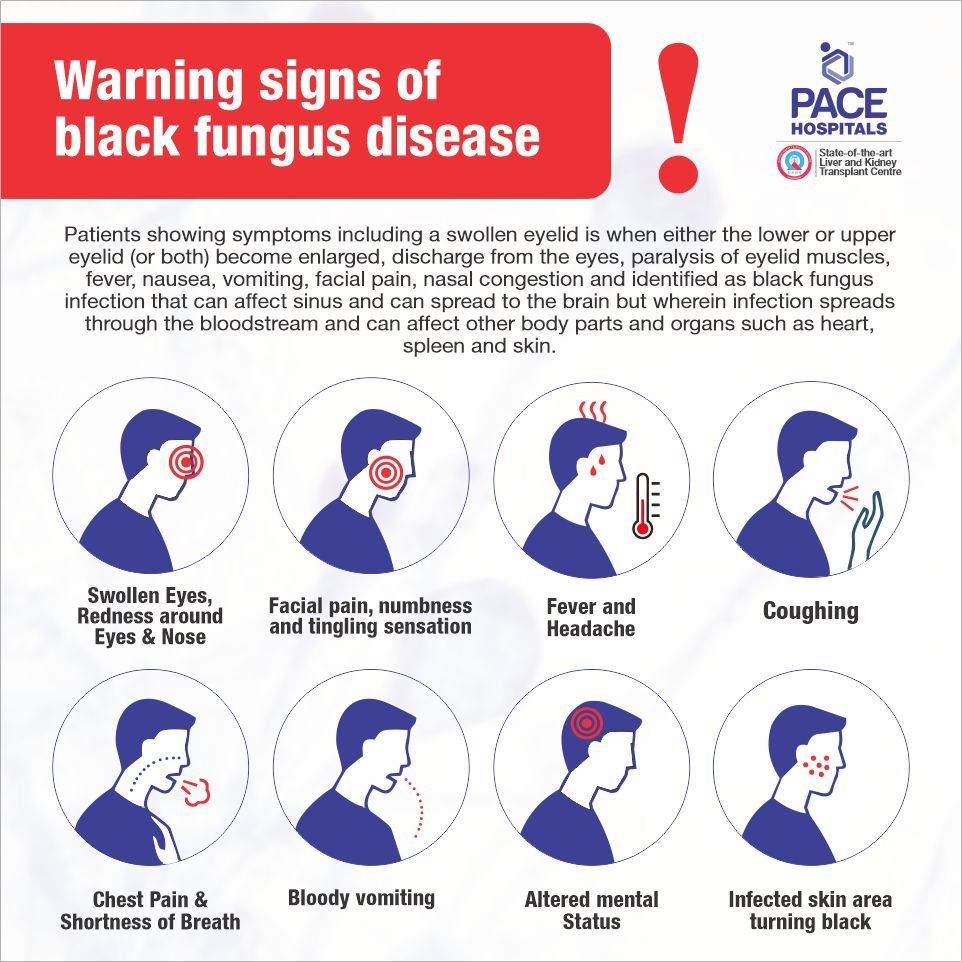
Mucormycosis disease can affect multiple organs and body parts. It can lead to blackening or discoloration over the nose, blurred or double vision, chest pain, breathing difficulties and coughing of blood. Symptoms depend upon the infection where the fungus growing in the body.
Pulmonary mucormycosis (lung) related symptoms –
- Difficulty breathing or shortness of breath
- Chest pain
- Fever (a temperature above 100 °F)
- Coughing that produce bloody or dark fluids
Rhinocerebral mucormycosis (sinus and brain) related symptoms –
- Fever
- Headache
- Sinus or nasal congestion
- Facial swelling one side
- Black lesions in upper inside of mouth or on nasal bridge
Cutaneous mucormycosis (skin) related symptoms –
- Facial pain
- A small bubble on the skin filled with serum
- Skin ulcers or skin infection in the air pockets located behind our forehead, nose, cheekbones, and in between the eyes and teeth
- Infected skin area turning black
- Warmth and excessive reddening
- Swelling around infection
Gastrointestinal mucormycosis related symptoms –
- Nausea and vomiting
- Abdominal or stomach pain
- Gastrointestinal bleeding
Disseminated mucormycosis related symptoms –
- It happens in the patients who are already suffering from other illness or chronic disease and difficult to distinguish the symptoms because patients already having other symptoms as well. Disseminated infection most commonly affects the brain, central nervous system and create situation like coma or other mental stage.
- A swollen eyelid is when either the lower or upper eyelid (or both) become enlarged and discharge from the eyes
- Paralysis of eyelid muscles
Who are at risk of Black Fungal Infection - Mucormycosis?
People those who suffering from these diseases or medical conditions are prone to develop mucormycosis due to reduced immunity caused by medical conditions or take medicines that suppress the immune system to fight germs and sickness.
- Coronavirus and other severe acute respiratory syndrome (SARS)
- Viral diseases like adenovirus infection, parainfluenza virus infection, flu (influenza), common cold, human immunodeficiency virus (HIV/AIDS), herpes, human papillomavirus (HPV), chickenpox, respiratory syncytial virus infection, infectious mononucleosis, mumps, measles and rubella, shingles, viral gastroenteritis (stomach flu), viral hepatitis, viral meningitis, viral pneumonia,
- Immunodeficiency disorders and other diseases such as ataxia-telangiectasia, chediak-higashi syndrome, combined immunodeficiency disease, complement deficiencies, diGeorge syndrome, hypogammaglobulinemia, job syndrome, leukocyte adhesion defects, panhypogammaglobulinemia, bruton’s disease, congenital agammaglobulinemia, selective deficiency of IgA, wiskott-aldrich syndrome, congenital bone marrow disease, hemochromatosis, severe burns, chronic kidney disease, chronic liver disease, liver cirrhosis, neutropenia, cancers and uncontrolled diabetes.
- During COVID-19 treatment patients who have prescribed for steroids treatment are particularly at risk because steroids suppress the immune system. Also, patients who have gone through organ transplant, stem cell transplant, depend on immunosuppressant drugs are at the risk of black fungal infection.
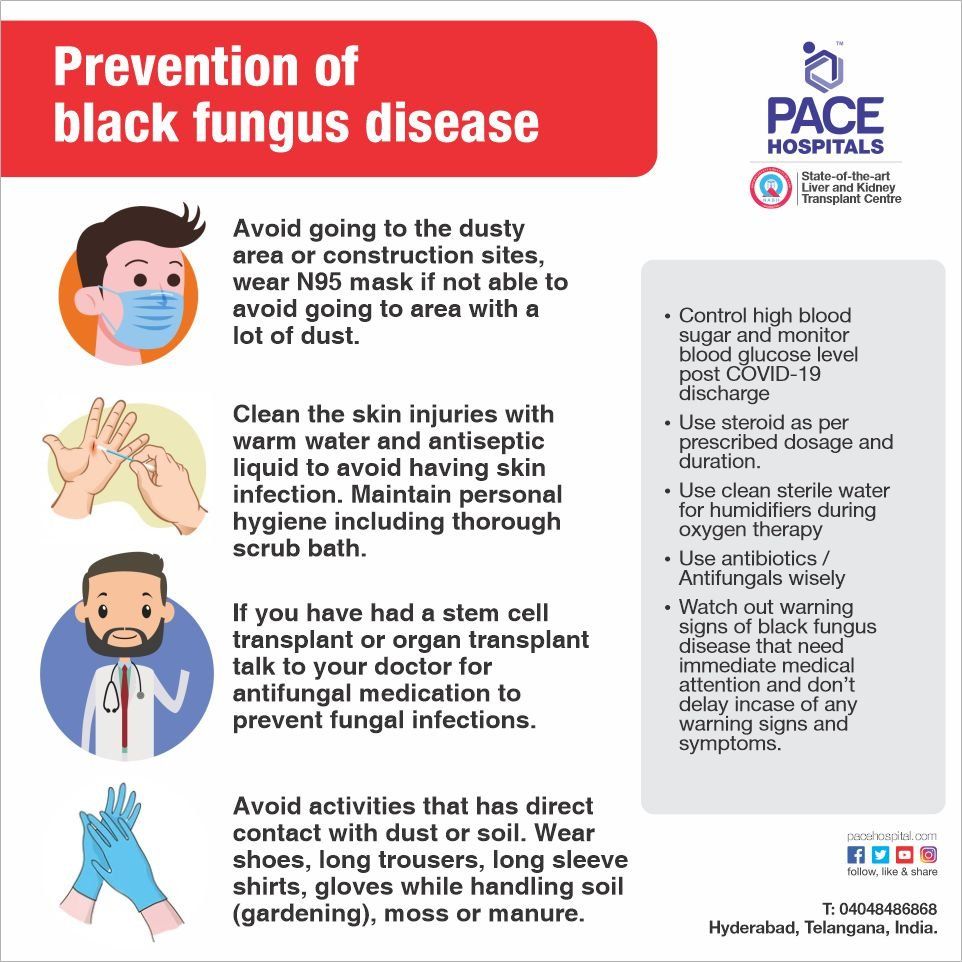
What are prevention and precautions to lower the risk of Mucormycosis?
It is impossible to stop breathing fungal spores because they are dispersed in the environment. Currently, there is no vaccine to stop mucormycosis and people who have weakened immune system should follow these guidelines to prevent the risk.
- Maintain personal hygiene including thorough scrub bath
- Avoid going to the dusty area or construction sites, wear N95 mask if not able to avoid going to area with a lot of dust.
- Avoid activities that has direct contact with dust or soil. Wear gloves, long shoes if doing any of the activity related to soil.
- Clean the skin injuries with warm water and antiseptic liquid to avoid having skin infection.
- If you have had a stem cell transplant or organ transplant talk to your doctor for antifungal medication to prevent mucormycosis or other fungal infections.
Testing and diagnosis for Mucormycosis
Based on medical history, physical examination, symptoms and infections areas, doctor may advise laboratory and imaging test to identify the evidence of mucormycosis. Following tests can help in identification of fungal infection -
- Laboratory test of fluid sample from respiratory system
- Tissue sample collection for biopsy
- Imaging tests - CT scan of your sinuses, lungs or other parts of body, depending on the suspected infection location.
What are treatment options of Mucormycosis?
Mucormycosis is a serious infectious disease, it can become fatal if not treated quickly. In cases where the infection identified at early sinus stage, mostly patients completely recover from it.
- Antifungal medicines (Liposomal Amphotericin B, Posaconazole and Isavuconazole) are given through a vein or by mouth.
- Often require a surgery to cut the infected tissue or parts.
Amphotericin B is an effective antifungal agent used to treat serious, life-threatening fungal infections but having strong side effects like blood in your stools, neurological issues such as seizure (convulsions), kidney dysfunction (such as little or no urination; painful or difficult urination, swelling in your feet or ankles), fluid build-up in your lungs, jaundice and stroke.
Patients might require an intravenous anti-fungal procedure up to 28 to 42 days.
Due to second wave of Coronavirus (COVID-19), twin cities Hyderabad and Secundrabad in Telangana recorded a new highest-ever surge in daily average cases that reported new serious and life-threatening disease i.e. Black fungal infection (mucormycosis). Government of Telangana health department declared it a notifiable disease under the Epidemic Diseases Act 1897. Director of Public Health made it mandatory for all government and list of hospitals treating black fungus in Hyderabad to report all suspected and confirmed cases to the Health Department. Department of Health, Medical & Family Welfare, Telangana under supervision of Greater Hyderabad Municipal Corporation (GHMC) in Hyderabad assigned the task to Govt hospitals to overcome from the pandemic situation and treat the patients.
Home Care Treatment support for suspected or diagnosed COVID-19 patient to recover while in home quarantine
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868