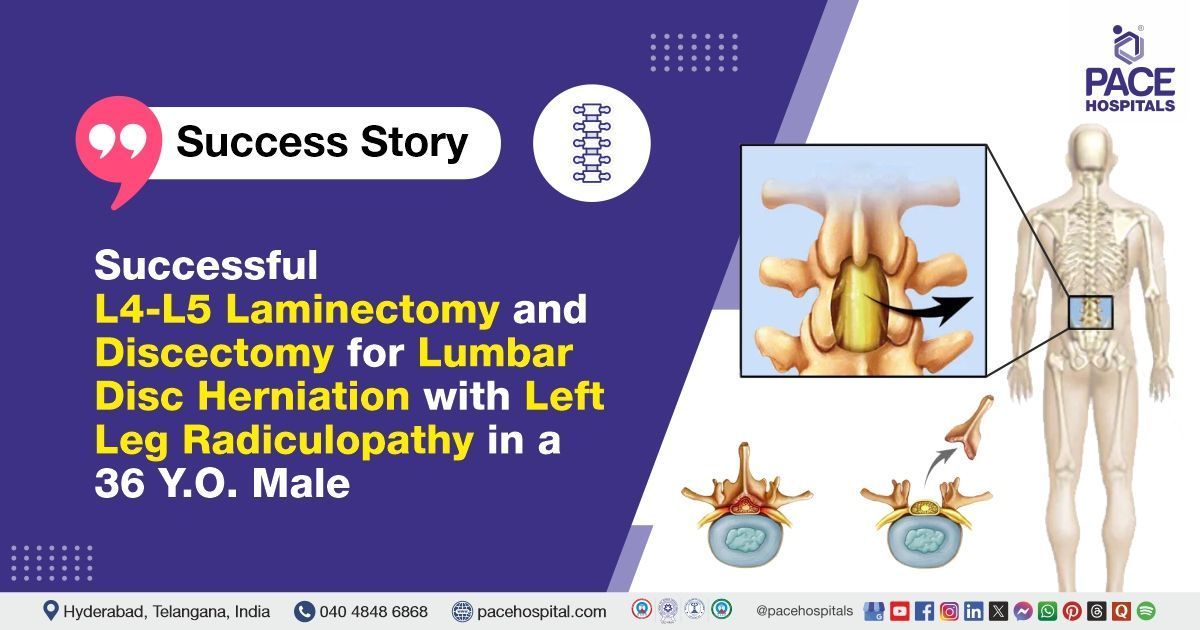
Successful L4-L5 Laminectomy and Discectomy for Lumbar Disc Herniation with Left Leg Radiculopathy in a 36 Y.O. Male
PACE Hospitals
PACE Hospitals’ expert Neurosurgery team successfully performed a Minimally Invasive L4-L5 Laminectomy and Discectomy on a 36-year-old male patient diagnosed with an L4-L5 prolapsed intervertebral disc associated with left lower limb (LT LL) radiculopathy. The procedure aimed to relieve nerve compression, reduce radiating leg pain and neurological symptoms, and restore mobility. Using a precise, minimally invasive approach, the team successfully treated the disc prolapse with a positive outcome.
Chief Complaints
A 36-year-old male patient with a body mass index (BMI) of 22 presented to the Neurosurgery Department at PACE Hospitals, Hitech City, Hyderabad, with complaints of lower back pain and left lower limb radiculopathy persisting for the past six months.
Past Medical History
The patient had no known history of
hypertension or
diabetes. The absence of these comorbid conditions was considered clinically favorable, as it had minimized the risk of intraoperative and postoperative complications and had supported a smoother, more stable recovery in this case.
On Examination
On examination, the patient appeared moderately built and nourished. Vital signs were found to be within normal limits. Systemic examination revealed normal muscle power in all limbs, with bilateral flexor plantar reflexes. The Straight Leg Raise Test (SLRT) was positive on the left side, indicating an abnormal finding suggestive of nerve root irritation corresponding to the patient’s left lower limb radiculopathy.
Diagnosis
Upon admission to PACE Hospitals, the patient underwent a detailed clinical evaluation by the Neurosurgery team, including a comprehensive physical examination and review of symptoms. He presented with persistent low back pain radiating to the left lower limb for the past six months, raising clinical suspicion of lumbar disc pathology with associated radiculopathy.
MRI of the lumbar spine revealed diffuse disc bulge at the L4-L5 level with a peripheral annular tear indenting the thecal sac, causing moderate bilateral lateral recess stenosis and indentation of the traversing nerve roots. Moderate to severe spinal canal stenosis was also noted at this level, with no evidence of neural foramen compromise. X-ray of the lumbar spine showed normal alignment and disc spaces. Routine chest X-ray, 2D ECHO, and preoperative assessments indicated normal cardiac, pulmonary, and systemic status.
Laboratory investigations, including complete blood count (CBC), coagulation profile, liver function test and renal function tests, serum electrolytes, and viral screening, were all within normal limits. No signs of infection or systemic illness were observed. Urine examination was unremarkable.
Based on the confirmed findings, the patient was advised to undergo
L4-L5 Prolapsed Intervertebral Disc With LT LL
Radiculopathy Treatment in Hyderabad, India, under the expert care of the Neurosurgery Department.
Medical Decision Making (MDM)
After a detailed consultation with Dr. U.L. Sandeep Varma, Consultant Neurosurgeon, a comprehensive evaluation was conducted to determine the most appropriate diagnostic and therapeutic approach for the patient, presenting with low back ache and left lower limb radiculopathy for six months. Based on detailed clinical evaluation and imaging studies, including MRI of the lumbar spine, surgical intervention was deemed necessary.
It was determined that the patient had an L4-L5 prolapsed intervertebral disc causing nerve root compression and radiculopathy. Minimally invasive L4-L5 laminectomy and discectomy were identified as the most effective intervention to relieve nerve compression, alleviate symptoms, and restore functional mobility.
The patient and his family members were informed about his condition, the planned procedure, associated risks, and the potential to alleviate symptoms and improve his quality of life.
Surgical Procedure
Following the decision, the patient was scheduled to undergo L4-L5 Minimal Invasive Laminectomy and Discectomy Surgery in Hyderabad at PACE Hospitals, under the expert supervision of the Neurosurgery Department.
The procedure involved the following steps:
- Preparation and Anesthesia: The patient was positioned prone on the operating table under general anesthesia. Strict aseptic precautions were followed. The surgical site at the L4-L5 level was identified and marked using fluoroscopic guidance to ensure accurate localization.
- Incision and Exposure: A small vertical midline incision was made over the L4-L5 interlaminar space. Soft tissues and muscles were gently dissected and retracted to expose the lamina without excessive tissue damage, maintaining the minimally invasive approach.
- Laminectomy and Ligamentum Flavum Removal: The L4 lamina was partially removed (laminotomy) using high-speed burrs and fine surgical instruments to create adequate space. The ligamentum flavum was excised carefully to expose the dura mater and the underlying nerve roots.
- Discectomy and Nerve Root Decompression: The herniated portion of the L4-L5 intervertebral disc was visualized. The prolapsed disc material was removed piecemeal with micro-instruments to decompress the left L5 nerve root. Adequate decompression was confirmed by ensuring the nerve root was lax and pulsatile.
- Hemostasis and Closure: Meticulous hemostasis was secured to prevent postoperative bleeding. The surgical wound was closed in layers with sutures. A sterile dressing was applied, and the patient was shifted to recovery for postoperative observation.
Postoperative Care
The postoperative period was uneventful. The patient was observed overnight in the Intensive Care Unit (ICU) before being shifted to the general ward. Vital signs remained stable, and the patient reported reduced pain with full muscle strength in both lower limbs. Postoperative treatment included continued administration of antibiotics, analgesics, gastric protectants, and nutritional supplements as prescribed. The patient was discharged on postoperative day 2 with instructions to adhere strictly to the prescribed medications and attend regular follow-up appointments for ongoing evaluation and rehabilitation.
Discharge Medications
Upon discharge, the patient was prescribed a course of antibiotics to prevent postoperative infections, neuropathic pain medications for managing nerve-related discomfort, and analgesics to control pain and inflammation. Gastroprotective agents were included to safeguard the stomach from irritation, alongside anti-inflammatory drugs to reduce swelling and promote healing. Nutritional supplements were also provided to support tissue repair and overall recovery. For local wound care, a topical antibiotic ointment was recommended to prevent infection, and a soft cervical collar was advised to provide cervical spine support during the healing process.
Advice on Discharge
The patient was advised to take baths and gradually resume walking and climbing stairs. He was instructed to avoid strenuous physical activities and limit prolonged sitting to less than one hour.
Emergency Care
The patient was informed to contact the emergency ward at PACE Hospitals in case of any emergency or development of symptoms such as fever, weakness, discharge from wound, severe pain.
Review and Follow-Up Notes
The patient was advised to follow up with the Neurosurgeon in Hyderabad at PACE Hospitals 1 month after discharge.
Conclusion
This case highlights the successful management of L4-L5 prolapsed intervertebral disc with left lower limb radiculopathy through minimally invasive laminectomy and discectomy. The patient showed significant improvement in pain and neurological function postoperatively. Careful perioperative monitoring and appropriate rehabilitation contributed to a stable recovery and favorable outcome.
Advancements in Minimally Invasive Spine Surgery
Minimally invasive spine surgery has revolutionized the management of lumbar disc herniation and radiculopathy by reducing surgical trauma and promoting faster recovery. These techniques allow precise decompression of affected nerve roots while preserving surrounding tissues, leading to decreased postoperative pain and shorter hospital stays. Early surgical intervention is often beneficial when conservative treatments fail, preventing long-term neurological complications.
Comprehensive postoperative care, including pain control and rehabilitation, is vital to ensure optimal functional outcomes. The role of the
neurosurgeon / neurosurgery doctor is pivotal in evaluating and performing these advanced procedures, which represent a significant advancement in spine surgery, ultimately improving patient satisfaction and quality of life.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles