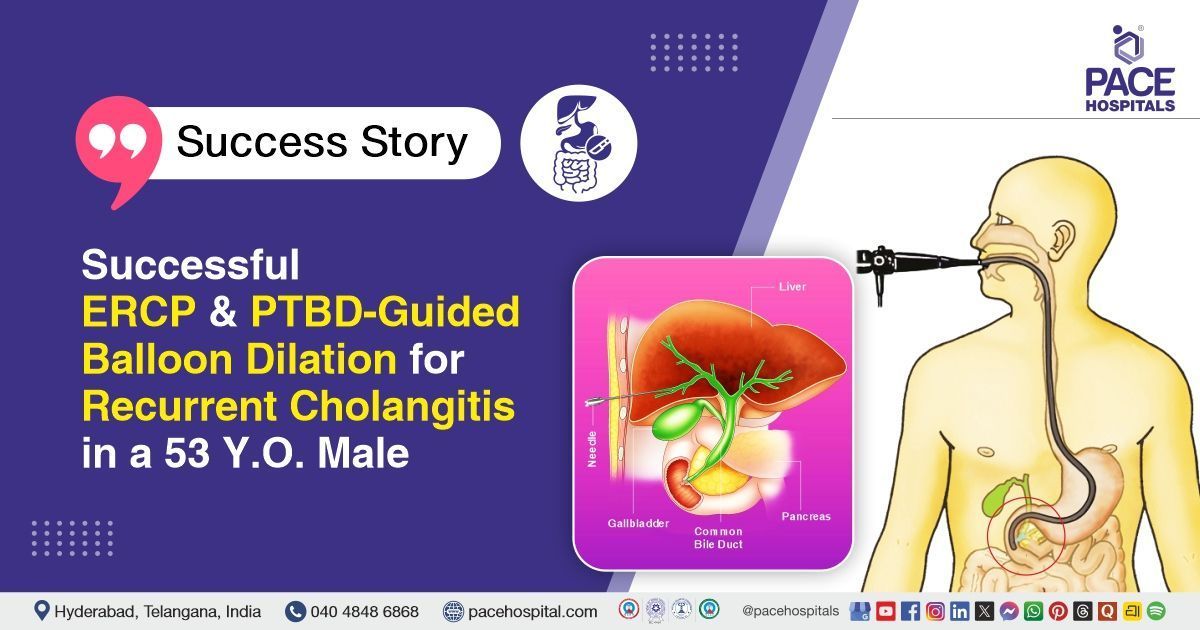
Successful ERCP and PTBD-Guided Balloon Dilation for Recurrent Cholangitis in a 53 Y.O. Male
PACE Hospitals
PACE Hospitals’ expert Surgical Gastroenterology team successfully performed Endoscopic Retrograde Cholangiopancreatography (ERCP) combined with PTBD-guided post-hurricane balloon dilation, bilateral biliary stenting, and subsequent common bile duct (CBD) clearance on a 53-year-old male patient who had previously undergone a deceased-donor liver transplant and was diagnosed with post-transplant biliary stricture and choledocholithiasis, status post prior ERCP stenting. The aim of the procedure was to relieve biliary obstruction, restore adequate bile drainage, and remove biliary stones.
Chief Complaints
A 53-year-old male with a
body mass index (BMI) of 22 presented to the Surgical Gastroenterology Department at
PACE Hospitals, Hitech City, Hyderabad, with a history of recurrent episodes of cholangitis, and he had no history of yellowish discoloration of the eye, nor any history of fever.
Past Medical History
The patient was a known case of
Type 2 Diabetes Mellitus,
Hypertension, and
Chronic Kidney Disease, for which he was on regular medication. He had previously undergone a Deceased Donor Liver Transplantation (DDLT) and had since been maintained on immunosuppression. He was later diagnosed with a post-transplant biliary stricture and had required multiple
ERCP procedures with stricture dilation and stenting over time. He also had a history of recurrent cholangitis, which had necessitated repeated hospital visits and endoscopic interventions.
On Examination
On examination, the patient was conscious, coherent and oriented, with stable vital signs and appeared comfortable without acute distress. There was no icterus, pallor, or dehydration. Abdominal examination revealed a soft, non-distended abdomen with a well-healed transplant scar, no tenderness, guarding, or rebound, and normal bowel sounds. No hepatosplenomegaly or palpable masses were noted. Cardiovascular, respiratory, and neurological examinations were normal, and there was no pedal edema. Overall, the findings indicated a stable post–liver transplant status with features suggestive of biliary obstruction rather than acute systemic illness.
Diagnosis
Upon admission to PACE Hospitals, the patient was thoroughly evaluated by the Surgical Gastroenterology team, which included a clinical examination and a history of recurrent episodes of cholangitis following a deceased donor liver transplant performed eight years ago. There was a strong clinical suspicion of biliary stricture with choledocholithiasis.
The patient underwent a comprehensive diagnostic evaluation for biliary obstruction. Ultrasound abdomen revealed a dilated common bile duct (CBD) with echogenic sludge and calculi. MRCP showed mild to moderate narrowing at the biliary anastomosis with residual upstream dilation. Routine blood investigations, including liver and renal function tests, complete blood picture, electrolytes, and coagulation profile, showed deranged liver enzymes and elevated bilirubin levels, consistent with biliary obstruction.
Based on the confirmed diagnosis, the patient was advised to undergo Post-Transplant Biliary Stricture with Choledocolithiasis Treatment in Hyderabad, India, under the expert care of the Surgical Gastroenterology Department.
Medical Decision Making
After a detailed consultation with consultant Surgical Gastroenterologist, Dr. CH Madhusudan, a thorough evaluation was conducted considering the patient’s history of recurrent cholangitis, previous deceased donor liver transplantation, and multiple prior ERCPs for biliary stricture management. Imaging studies including ultrasound and MRCP confirmed biliary anastomotic stricture with choledocholithiasis and upstream biliary dilation.
Based on these clinical and imaging findings, it was determined that Endoscopic Retrograde Cholangiopancreatography (ERCP) with PTBD-guided Hurricane balloon dilation, bilateral biliary stenting, and subsequent CBD clearance was identified as the most appropriate intervention to relieve the stricture, remove calculi, restore biliary drainage, and prevent further episodes of cholangitis.
The patient and family members were counselled regarding the diagnosis, the planned endoscopic procedures, potential risks including bleeding, infection, or stent-related complications, and the anticipated benefits in terms of symptomatic relief and long-term graft function.
Surgical Procedure
Following the decision, the patient was scheduled to undergo Endoscopic Retrograde Cholangiopancreatogram (ERCP) Plus PTBD Guided, Post Hurricane Balloon Dilation, Bilateral Stenting followed by CBD Clearance in Hyderabad at PACE Hospitals under the expert supervision of the Surgical Gastroenterology Department.
The following steps were carried out during the procedure:
- Preparation and Scope Insertion: The patient was taken to the endoscopy suite after pre-procedure preparation. A side-viewing duodenoscope was introduced and advanced carefully up to the second part of the duodenum (D2) to access the ampulla of Vater. Proper positioning and visualization of the biliary anatomy were ensured before proceeding.
- Left Hepatic Duct Cannulation and PTBD Guidance: Using the pre-existing PTBD (Percutaneous Transhepatic Biliary Drain) tract, the left hepatic duct was selectively cannulated under guidewire guidance. Contrast injection confirmed ductal anatomy and the presence of stricture and sludge. This step allowed safe access to the intrahepatic biliary system for intervention.
- Hurricane Balloon Dilation of the Left Hepatic Duct: A Hurricane balloon was positioned across the stricture in the left hepatic duct. Controlled balloon inflation was performed to dilate the biliary stricture, restoring ductal patency. Balloon sweeps were performed afterwards, which revealed stones and sludge, confirming the need for further clearance.
- Left and Right Hepatic Duct Stenting: A 7 French, 15 cm single plastic stent was deployed in the left hepatic duct to maintain ductal patency after dilation. The right hepatic duct was then selectively cannulated using the standard guidewire technique. Balloon sweeps were performed, and a similar 7 French, 15 cm stent was placed in the right hepatic duct. Bilateral stenting ensured adequate bile drainage and reduced the risk of recurrent cholangitis.
- Common Bile Duct (CBD) Clearance: After stenting, balloon sweeps of the CBD were performed to remove residual stones and sludge. Complete clearance of the CBD was confirmed with contrast injection under fluoroscopy. The procedure concluded with proper placement of stents and the PTBD catheter, ensuring unobstructed bile flow.
Postoperative Care
The procedure was uneventful, and the patient had a smooth postoperative recovery. He was started on an oral diet the following day and showed symptomatic improvement. On postoperative day 2, USG screening confirmed the biliary stents and segment 3 PTBD were in place, with the CBD measuring 10 mm and mild central bilobar intrahepatic biliary radicle dilation. The patient was subsequently discharged with appropriate follow-up instructions.
Discharge Medications
Upon discharge, the patient was advised to continue medications for immunosuppression, infection prophylaxis, pain management, liver support, nutritional supplementation, and ongoing control of chronic conditions such as diabetes, hypertension, and kidney function.
Advice on Discharge
The patient was advised to continue a regular, balanced diet, ensuring adequate nutrition to support recovery and overall liver health.
Emergency Care
The patient was informed to contact the emergency ward at PACE Hospitals in case of any emergency or development of symptoms such as fever, abdominal pain ,chest pain and vomiting.
Review and Follow-up Notes
The patient was advised to return for a follow-up visit with the Surgical Gastroenterologist in Hyderabad at PACE Hospitals, after 3 days, for further evaluation.
Conclusion
This case highlights a post-liver transplant patient with biliary stricture and choledocholithiasis who underwent ERCP with balloon dilation, bilateral stenting, and CBD clearance. The procedure was uneventful, and the patient recovered well. He was discharged in stable condition with follow-up advised for monitoring biliary stents and liver function.
Managing Late Biliary Complications Post-Liver Transplant
Late biliary complications, such as strictures and stone formation, can occur even years after a successful liver transplantation, highlighting the need for lifelong monitoring. Minimally invasive techniques like PTBD-guided balloon dilation and stenting are effective in managing complex biliary issues while avoiding major surgery. Regular follow-up, timely imaging, and care under a surgical gastroenterologist / surgical gastroenterology doctor are essential to prevent recurrent cholangitis, preserve graft function, and maintain patient quality of life.
Individualized, patient-centered interventions and careful management of transplant therapy and comorbidities are critical for long-term post-transplant success. Early recognition and prompt treatment of complications help reduce morbidity, prevent graft loss, and enhance overall survival in liver transplant recipients.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles