Craniotomy Procedure | Surgery and Cost
PACE Hospitals is recognized as the best craniotomy surgery hospital in Hyderabad, India, known for its excellence in neurosurgical care. Our highly experienced neurosurgeons specialize in complex brain procedures that require removing a portion of the skull to access the affected area. With modern ICUs, advanced post-operative care units, and a strong patient-focused approach, PACE Hospitals ensures comprehensive recovery and continues to stand out as the leading choice for craniotomy in Hyderabad.
Request an Appointment for Craniotomy Procedure
Craniotomy Surgery appointment
Why Choose PACE Hospitals for Craniotomy Surgery?

4600+ Patients treated for Trauma and Tumor
Team of the Best Neurosurgeon in Hyderabad
Precision Treatment with 99.9% success rate
All insurance accepted with No-cost EMI option
PACE Hospitals is renowned as the best hospital for craniotomy surgery in Hyderabad, India. The hospital's Department of Neurosurgery is staffed with a team of highly skilled and experienced neurosurgeons who are dedicated to providing the highest level of care to patients requiring craniotomy surgery. The hospital is equipped with advanced technology and facilities, including state-of-the-art operating theaters, imaging equipment, and intensive care units.
PACE Hospitals' approach to craniotomy surgery is comprehensive and personalized, involving a team of specialists working together to provide a precise diagnosis and develop an effective treatment plan. The hospital's medical team uses the latest surgical techniques and technologies, such as image-guided surgery and minimally invasive approaches, to ensure the best possible outcomes for patients. These techniques result in reduced risk of complications, less post-procedure discomfort, and faster recovery times for patients.
PACE Hospitals is known for its patient-centered care, with a strong emphasis on patient comfort and satisfaction. The hospital's staff is committed to providing compassionate care, ensuring that patients and their families are well-informed about their condition and treatment options, and addressing any concerns or questions they may have. Whether it's for tumor removal, trauma management, or other neurological disorders, PACE Hospitals consistently delivers exceptional results, solidifying its position as one of the best craniotomy surgery hospital in Hyderabad.
Craniotomy meaning
A craniotomy is a surgical procedure in which a tiny hole is created in the skull, or a part of the bone is temporarily removed to expose the brain for performing an intracranial procedure by a neurosurgeon. It may be performed to remove a tumour of the brain or a sample of brain tissue, remove blood or blood clots from the brain, repair a skull fracture or brain aneurysm (bulge or swelling of a blood vessel wall), relieve pressure in the brain after a stroke or injury or treat other brain conditions.
In craniotomy, the surgeon removes a piece of the skull (bone flap) to access the brain and then immediately replaces and attaches to the surrounding bone using specialized tools such as tiny titanium plates and screws.

Types of Craniotomies
The following are some of the types of craniotomies, divided based on the specific location and nature of the brain tissue being treated, includes:
- Extended Bifrontal Craniotomy
- Minimally Invasive Supra-Orbital Craniotomy
- Retro-Sigmoid “Keyhole” Craniotomy
- Orbitozygomatic Craniotomy
- Translabyrinthine Craniotomy
Extended Bifrontal Craniotomy
- The extended bifrontal craniotomy is a traditional skull-based surgical technique used to reach tumours located at the front of the brain.
- It involves making an incision in the scalp just behind the hairline and removing a section of bone that forms the contour of the orbits (eye sockets) and the forehead (shape of the forehead).
- This removed bone is replaced at the end of surgery. Removing this bone for a short time allows the surgeon to work in the space between and right behind the patient's eyes without unnecessarily manipulating the brain.
- This approach is preferred because it allows surgeons to access the tumour without having to manipulate the brain excessively, thereby reducing potential risks associated with brain tissue manipulation.
- Typically, this craniotomy approach is chosen for tumours that cannot be removed through less invasive methods due to the tumour's location, type, or specific surgical goals.
- Types of tumours treated with this craniotomy include esthesioneuroblastomas, meningiomas, and malignant skull base tumours.
Minimally Invasive Supra-Orbital Craniotomy
- A supra-orbital craniotomy, also called an "eyebrow" craniotomy, is a minimally invasive approach that is performed to remove brain tumours.
- During this procedure, neurosurgeons make a small incision within the eyebrow to access tumours around the pituitary gland or in the front of the brain, which is more in-depth in the brain behind the eyes and nose.
- It is recommended when a tumour is large or close to the vital arteries or optic nerves and used instead of endonasal endoscopic surgery.
- This procedure has a lot of benefits, such as minimal scarring, faster recovery and less pain than open craniotomy.
- This craniotomy may be considered as part of the treatment for Rathke’s cleft cysts, and some pituitary and skull base tumours.
Retro-Sigmoid “Keyhole” Craniotomy
- Retro-sigmoid craniotomy is a minimally invasive (keyhole" craniotomy) procedure used to remove brain tumours. It allows the neurosurgeon to remove the skull base tumours through a tiny incision made behind the ear, providing access to the brainstem and cerebellum. This approach will be used to reach specific tumours, including skull base tumours, meningiomas, metastatic brain tumours and acoustic neuromas (vestibular schwannomas).
Orbitozygomatic Craniotomy
- The orbitozygomatic craniotomy is also one of the traditional skull base approaches, which is performed to target difficult tumours that are too complex for removal by minimally invasive approaches and aneurysms.
- This approach is preferred, like extended bifrontal craniotomy, because it allows surgeons to access the tumour without having to manipulate the brain overly.
- Similar to extended bifrontal craniotomy, in this procedure, the neurosurgeon makes an incision (cut) in the scalp behind the hairline and temporarily removes a section of bone that forms the contour of the orbits (eye sockets) and the forehead (shape of the forehead) and replaces at the end of surgery. Orbitozygomatic craniotomy is used to treat brain tumours, including craniopharyngiomas, meningiomas and pituitary tumours
Translabyrinthine Craniotomy
- A translabyrinthine craniotomy is a surgical approach used to access and remove tumours located in the inner auditory canal and cerebellopontine angle through the inner ear.
- It removes benign ear tumours that develop near the hearing and balance nerves in the ear, such as vestibular schwannomas or acoustic neuromas.
- During the removal of acoustic neuromas, neurosurgeons remove the semicircular canals of the ear in order to access the tumour by using translabyrinthine craniotomy, where complete hearing loss can occur, which is performed when hearing is not functional or when sacrificing hearing is acceptable by the patient.
- Although hearing is lost in patients who have undergone translabyrinthine craniotomy, the risk of facial nerve injury may be reduced.
- It involves making an incision in the scalp behind the ear and then removing the mastoid bone and some part of the inner ear bone (specifically, the semicircular canals that contain receptors for balance) to reach the tumour and remove the tumour or as much of the tumour as possible without disturbing critical nerves and without the risk of severe damage to the brain.
- By accessing the tumour through the labyrinthine region, neurosurgeons reduce damage to surrounding brain tissue, as mentioned above and nerves crucial for hearing and balance functions.

Craniotomy procedure is indicated in persons who are suffering from tumours, trauma, vascular, infectious, miscellaneous conditions and parasitic lesions. The following are the detailed conditions that can come under the indications of craniotomy:
Trauma
- Acute extradural hematoma: It is a collection of blood that forms between the outside of the dura mater (the outer protective layer of the brain) and the inner surface of the skull.
- Acute subdural hematoma: It is an abnormal collection of blood between the inside of the dura mater and the inner surface of the skull.
- Brain contusions: These are also called cerebral contusions, characterized by scattered areas of bleeding (bruises) on the surface of the brain.
- Depressed skull fractures: A break in the skull bone (cranial bone or crushed portion of skull) causes part of the skull to sink in toward (being folded inward into) the brain.
- Cerebrospinal fluid (CSF) leak repair: A small leak of CSF may resolve itself, while larger leaks may require surgical intervention.
- Intracranial foreign bodies: These include the objects that have penetrated the skull and entered the brain or its surrounding structures through trauma or iatrogenic injuries.
Tumour
- Meningioma: It is a tumour that develops on layers of tissue called meninges that cover the brain and spinal cord just inside the skull.
- High-grade and low-grade glioma: High-grade and low-grade glioma: Gliomas are four types of brain tumours, including grades 1, 2, 3, and 4. Low-grade gliomas are slower-growing tumours with lower malignancy, including grades 1 and 2, while high-grade gliomas are grades 3 and 4, which are aggressive brain tumours with fast growth and higher malignancy.
- Epidermoid: These tumours are congenital, benign, and slow-growing and originate from skin cells trapped in the brain and spinal cord during development.
- Ependymoma: It is a slow-growing tumour that develops in the brain or spinal cord, and it is called a primary central nervous system (CNS) tumour.
- Oligodendroglioma: A rare type of primary brain tumour that originates from glial cells (oligodendrocytes) from the brain.
- Metastases (Metastatic cancer): These are called brain metastases, also called as metastatic brain cancer, are the tumours that arise (begins) when cancer cells from another part of the body spread to the brain.
- Orbital tumours: These are abnormal tumours (benign or cancerous) of tissues originating from the structures surrounding the eye.
- Cerebellopontine angle tumours: CPA tumours are slow-growing masses, mostly benign with low potential for malignancy, that grow in the posterior fossa (small space in the brain) of the brain.
Vascular problems
- Intracerebral haemorrhage: It is a type of stroke which is a neurological emergency that can be characterized by bleeding caused by a rupturing of a blood vessel within the brain.
- Malignant Middle cerebral artery (MCA) territory infarction: Malignant middle cerebral artery (MCA) infarcts represent the most severe type of acute stroke and occur in approximately 8% of ischemic strokes.
- Cortical venous thrombosis (CVT) with haemorrhagic infarction: It is a rare subtype of cerebral venous thrombosis (CVT) that can cause a stroke (which is a blood clot in the cortical veins of the brain), leading to brain tissue damage, bleeding and other neurological deficits.
- Aneurysm: Abnormal swelling or bulging in a weak area of a blood vessel within the brain.
- Vascular malformations (arterio-venous malformation, cavernous angioma, arterio-venous fistula): These are abnormal connections between blood vessels in the brain that disrupt normal blood flow, causing bleeding and other problems.
- Microvascular decompression: Surgical relief of nerve compression
Infections
- Abscess: Localized infection with pocket of pus
- Subdural empyema: Collection of pus between the dura mater and the arachnoid mater
Parasitic lesions
- Hydatid cyst: Parasitic cyst caused by Echinococcus
- Racemose neurocysticercosis (NCC): Common parasitic infection
Miscellaneous
- Epilepsy: Seizure disorder
- Functional surgery: Targeted brain stimulation for symptom relief
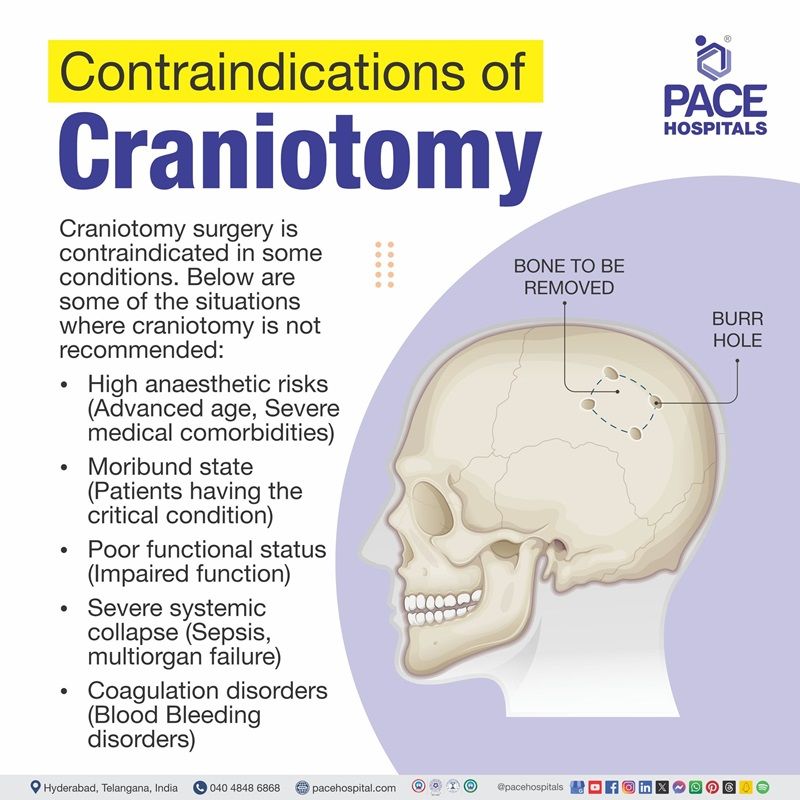
Craniotomy contraindications
Craniotomy is contraindicated in the following conditions: such as:
- High anaesthetic risks: Advanced age, Severe medical comorbidities
- Moribund state: Patients having the critical condition
- Poor functional status: Impaired function
- High frailty index:
- Severe systemic collapse (sepsis, multiorgan failure)
- Coagulation disorders: Blood Bleeding disorders
Absolute contraindication for awake craniotomy:
- Patient refusal
- Non-complaint patient
Relative contraindication for awake craniotomy:
- Obese patients
- Obstructive sleep apnoea: Condition where the airway becomes blocked during sleep
- Difficult airways
- Chronic refractory cough: Persistent cough
- Highly vascular lesions: Brain lesions with a lot of blood vessels
- Posterior fossa lesions: Brain lesions in the back part of the brain
Considerations of neurosurgeons before planning craniotomy
Before performing a craniotomy, neurosurgeons carefully assess several factors to ensure the procedure is safe and effective for the patient, including:
- Patient age
- Patient medical and medication history
- Neurological examination
- Imaging tests
- Benefit and risk assessment
- Anaesthesia-associated risks
- Surgical factors such as elective vs emergency
- Purpose of surgery (relieve pressure, tumour removal, manage bleeding, severe head injury, etc.)
Craniotomy procedure steps
Before the procedure
In many patients, a craniotomy is done urgently. However, in case a craniotomy is planned, check with the neurosurgeon about preparation (what to do to get ready) for the procedure. Below-mentioned is a list of common steps that may be asked to patients before performing the procedure:
- The patient will be asked to sign a consent form permitting the surgery, and a separate form will need to be signed to receive anaesthesia.
- In addition to a complete medical history, medication history, and family history, a surgeon will perform a physical exam, blood tests, and other certain diagnostic tests to confirm that the patient is in good health before surgery.
- Before surgery, a neurological exam will be performed to compare with one done after surgery.
- Generally, the patient will be asked to fast before the procedure. The surgeon will discuss with the patient if the patient is allergic to any medicine used in the procedure and has a history of bleeding disorders.
- If the patient has a smoking habit, it is advised to stop smoking as soon as possible before the procedure to improve the chance of successful recovery.
- Before the surgery, patients may be asked to wash their hair with a special antiseptic shampoo at night, and the areas around the surgical site will be shaved.
- Based on individual medical conditions, the health care team may request other specific preparations.
During the procedure
- The operation is carried out under general anaesthetic and may take approximately 4-6 hours. The patient may fall asleep and not feel anything during the procedure.
- During the procedure, the healthcare team removes clothes, jewellery, or other objects that may interfere with the craniotomy.
- A hospital gown is provided to wear and an IV line will be put in the patient's arm or hand to send the fluids and medicines.
- A catheter (urinary tube) will be inserted in the patient's bladder to drain the urine.
- Patient will be placed on the operating table during surgery to provide the neurosurgeon with the finest access to the side of the brain to be operated on.
- The anaesthesiologist monitors the blood pressure, heart rate, blood oxygen level and breathing throughout the operation.
- The healthcare team will rest the patient's head on a cushion or hold the patient in position with a specific device removed at the end of the surgery. The skin over the surgical site will be cleaned using an antiseptic solution.
- Depending on the affected area of the brain, the surgeon may use different types of incisions (open (large incision) or minimally invasive (smaller incisions) and the place, shape and size of the incision (skin cut) vary according to the type of craniotomy.
- Usually, a skin cut is placed behind the hairline to hide the incision scar. However, this is not always possible for all patients.
- The scar may fade to a pale, thin line within a few (usually 3 to 6) months, and the hair typically grows back where it has been shaved.
- Afterward, the scalp is pulled, and skin clips are used to control bleeding.
- A small part of the skull will be temporarily removed to reach the brain. However, the exact location of the opening or cutting is decided after careful consideration of brain scans and other investigations carried out before the surgery.
- The medical drill is used to drill the bone and make burr holes (Burr holes are small holes that a neurosurgeon makes in the patient skull. They’re the first step in a craniotomy before removing a flap of bone and are sometimes performed alone to relieve pressure within the brain) in the skull, or may use a special saw to cut the bone carefully, and the bone flap will be removed and reserved.
- The surgeon starts to separate the thick outer covering of the brain, called the durometer, directly underneath the bone from the bone and carefully cuts it open to expose the brain.
- If required, extra fluid will be allowed to flow out of the brain, and the neurosurgeon uses microsurgical tools to magnify the area being treated to get a better view of the brain.
- Once the opening has been made the neurosurgeon treats some medical issues based on the purpose of craniotomy indicated such as the abnormal tissue or growth (lesion), the blood clot, aneurysm (closing the connection between a blood vessel and an aneurysm) using a small clip and relieving the pressure on the brain.
- After the surgery, the bone is replaced to its position with small metal screws to cover the hole that has been made to avoid movement and promote better healing.
- The type of craniotomy approach, hospital stay, recovery time, and success rate may vary from patient to patient, depending on the individual's condition and the healthcare team's practices.
After the procedure
In the hospital
- Immediately after the procedure, to monitor the craniotomy patient closely, the patient may be taken from the operating room directly to the ICU or a recovery room for observation before being taken to the intensive care unit (ICU).
- Certain medications will be given to the patient to reduce brain swelling once the blood pressure, breathing, and pulse are stable. If the patient is alert, the healthcare team shifts the patient to a hospital room where they have to stay for a few days to fully recover.
- After surgery, oxygen is needed for the patient for some time. Before discharging the patient, the oxygen will be discontinued.
- Patient will be taught deep breathing exercises to help re-expand the lungs and avoid pneumonia.
- Medical staff will perform frequent neurological checks to test brain function and ensure body systems function properly after surgery.
- To assess brain function, patient will be asked to follow different basic commands, including moving arms and legs. The strength of the legs and arms will also be tested. The Pupils will be examined with a flashlight and asked questions to assess their orientation (such as name, date, and where they are).
- The patient is encouraged to move around in bed as tolerated (endured). After some time, the patient is also be asked to get out of bed and walk around, with assistance at first or on their own, as their strength improves.
- A physical therapist (PT) suggests exercises in the hospital and at home to improve strength, balance, and mobility.
- Depending on the patient's situation, the healthcare team advises drinking liquids a few hours after surgery and gradually changing liquids to a solid diet as the patient adjusts.
- As mentioned, the catheter is inserted into the bladder to drain urine until the patient get out of bed and move around. The patient must report any painful urination or other urinary symptoms that may occur after the catheter is removed, as these may be signs of an infection.
- Depending on the status, the patient may be transferred to a rehabilitation facility to regain strength over a period of time.
- Before discharging the patient from the hospital, health care team gives instructions for home care and makes arrangements for a follow-up visit with the neurosurgeon.
At home (craniotomy post operative care)
- Post-craniotomy, the patient is advised to keep the incision clean and dry.
- Depending on the type of stitches that are to be removed during the follow-up.
- The patient is suggested to wear a loose hat or turban (headwear) until the incision is completely healed.
- Take medicines without skipping as prescribed by healthcare team.
- Continue the breathing exercises performed in the hospital to avoid lung infection. The healthcare team advises the patient to avoid exposure to upper respiratory tract infections (such as colds and flu) and irritants, including smoke, fumes, and environmental pollution.
- The patient may gradually increase their physical activity as they can handle them, and it may take several weeks to return to their previous level of energy and strength.
Patients may instructed to:
- Avoid driving until the neurosurgeon gives permission.
- Avoid lifting heavy objects for a few weeks to avoid strain on their surgical incision.
Contact the healthcare professional to report any of the following:
- Vision changes
- Increased pain around the incision site
- Fever or chills
- Confusion or excessive sleepiness
- Redness, swelling, drainage, bleeding or other drainage from the incision site or face
- Trouble with speech
- Weakness of arms or legs
- Green, yellow, or blood-tinged sputum (phlegm)
- Trouble breathing, chest pain, anxiety, or change in mental status
- Seizure activity
Life expectancy after craniotomy
Many patients, after craniotomy, make a full recovery and can live a normal life with minimal side effects or complications.
However, some studies have found that survival rates may vary depending on the type of craniotomy and other factors such as patient age, overall health condition, incision size and location.
In the study, 80% of patients had complete remission (their disease was cured fully), 11.4% had partial remission (saw some improvement), and 8.6% had progressive disease (whose condition got worse) .Excluding two patients who were lost to follow-up, 81.8% were still alive with an average of 72 months. The overall survival rate at five years was 80.4%.
Craniotomy complications
A craniotomy is a safe and effective surgery that can treat many brain conditions. However, it can also have some complications, such as:
- Skull fractures: Breaks of skull bones.
- Cosmetic deformity: Changes in the appearance of the face or head
- Cerebrospinal fluid (CSF) leak: Leakage of CSF fluid from the spinal cord or brain.
- Post-craniotomy headache: Headache in the head following the surgery.
- Extraxial hematomas: Bleeding of blood outside the brain but within the skull.
- Seizures: Convulsions
- Tension pneumocephalus: Pressure due to presence of air in the brain cavity
- Hydrocephalus: Excess fluid buildup in the brain's ventricles.
- Intracranial haemorrhage (ICH): Bleeding within the brain tissue.
- Cerebral oedema: Swelling of the brain tissue.
- Cerebral ischemia: Reduced blood flow to the brain.
- Postoperative infection
- Electrolyte abnormalities
Questions that the patients can ask the healthcare team about craniotomy surgery?
- What are the wound care instructions for my incision site?
- How soon should I contact the healthcare team if I notice any unusual symptoms or issues after the procedure?
- What signs of complications or infections should I watch at the surgical site?
- When can I go back to my normal activities?
- Are there any specific activities I should avoid during my recovery period?
- What dietary restrictions should I follow for recovery?
- When should I schedule follow-up appointments?
- Will any tests or evaluations be required after the surgery?
Difference between Craniotomy and Craniectomy
Craniotomy vs Craniectomy
Craniotomy and craniectomy are both crucial brain surgeries that involve removing part of the skull; however, they differ in how the bone is handled after the surgery, which includes:
| Elements | Craniotomy | Craniectomy |
|---|---|---|
| Why it is performed | It is a general brain surgery which is performed to access the brain for treating various conditions such as tumour removal or aneurysm repair. | It is performed to relieve pressure from severe brain swelling or injury |
| Procedure | Temporarily removes skull portion to access the brain | Removal of skull portion to relieve pressure |
| Bone replacement | Immediately replaces the removed skull portion after the surgery | Skull portion (bone fragment) is not immediately replaced |
| Indications | Tumours, vascular malformations, aneurysms, epilepsy treatments | Emergency situations with significant brain swelling |
| Follow-up Surgery | May not needed | May require future surgery |
Craniotomy Surgery Cost in Hyderabad, India
The
cost of Craniotomy Surgery in Hyderabad generally ranges from ₹1,60,000 to ₹5,50,000 (approximately US $1,930 – US $6,630). The exact craniotomy surgery cost varies depending on factors such as the type of surgery performed (tumor removal, trauma, hematoma evacuation, brain abscess), size and location of the lesion, use of navigation technology, duration of ICU care, surgeon expertise, and the hospital facilities chosen — including cashless treatment options, TPA corporate tie-ups, and assistance with medical insurance approvals wherever applicable.
Cost Breakdown According to Type of Procedure
- Simple Craniotomy (Non-Complex Tumor / Biopsy) – ₹1,60,000 – ₹2,50,000 (US $1,930 – US $3,020)
- Craniotomy for Brain Tumor Removal (Standard) – ₹2,20,000 – ₹3,80,000 (US $2,650 – US $4,570)
- Craniotomy for Hematoma Evacuation (SDH/EDH) – ₹1,80,000 – ₹3,20,000 (US $2,170 – US $3,850)
- Complex Craniotomy (Deep-Seated Tumor, AVM, Aneurysm-Related) – ₹3,50,000 – ₹5,50,000 (US $4,210 – US $6,630)
Note: The cost of craniotomy in India varies widely depending on the complexity of the procedure, hospital setup, and surgical expertise involved.
Frequently asked questions (FAQs) on Craniotomy procedure
What is the survival rate of craniotomy?
Survival rates of craniotomy may vary depending on multiple factors such as patient age, overall health condition, type of approach, incision size and location.
Generally, the survival rate is high. However, outcomes can range from excellent to poor based on the specific case and any complications that arise. Risks are higher when craniotomy is performed in emergency, and if the patient has multiple comorbidities, including heart failure.
What are the risk factors for craniotomy?
Risk factors can increase the risk of complications or side effects and affect the outcomes during or after the craniotomy. Patient-specific risk factors include age, anaesthesia-associated risks, neurological status, frailty index, and medical comorbidities. Surgical risk factors include the size, location, and type of the lesion, duration of surgery, nature of procedures (elective vs. emergency), surgical type and approach and perioperative complications.
Which Is the Best Hospital for Craniotomy in Hyderabad, Telangana, India?
PACE Hospitals, Hyderabad, is regarded as one of the leading centres for neurosurgery, providing advanced care for brain tumors, traumatic brain injuries, hemorrhages, infections, and neurological emergencies.
Our team of highly experienced neurosurgeons performs life-saving brain surgeries using advanced neuro-navigation systems, intraoperative monitoring, high-precision microsurgical tools, and dedicated neuro-ICU care, ensuring safer outcomes and faster recovery.
With state-of-the-art operating theatres, round-the-clock neuro-critical care, advanced imaging support, and structured rehabilitation, PACE Hospitals ensures optimal results for both elective and emergency neurosurgical cases — supported by cashless facilities, TPA corporate tie-ups, and assistance with medical insurance processing for eligible patients.
How many times one can have craniotomy?
As per some studies, it was stated that patients could have a re-do craniotomy (second or third craniotomy up to 3 times as long as there is a need (indication) for it. However, having second and third re-do craniotomies tends to lead to poor outcomes, such as slow recovery and side effects, as compared to the first. A neurosurgeon decides whether the patients can have craniotomy multiple times if required by measuring the risk and benefit ratio.
How long will it take to get over a craniotomy?
Recovery after craniotomy depends on the type of surgical approach (open or minimally invasive procedure), the patient's health before the surgery, whether the patient had any neurological problems before or after the surgery, any complications from either the disease or the operation, the patient's age, the effects of any post-operative treatments, including recovery or radiotherapy, and other medical conditions.
How much does Craniotomy Surgery Cost in Hyderabad, at PACE Hospitals?
At PACE Hospitals, Hyderabad, the craniotomy procedure cost typically ranges from ₹1,50,000 to ₹5,00,000 and above (approximately US $1,810 – US $6,030), depending on:
- Type of procedure (craniotomy vs craniectomy)
- Reason for surgery (trauma, tumor, hematoma, infection, aneurysm, etc.)
- Complexity & location of the lesion
- Need for neuro-ICU admission & duration of hospital stay
- Surgeon expertise & use of neuro-navigation/monitoring
- Additional imaging, lab work, or rehabilitation care
For straightforward craniotomies, the cost falls toward the lower end, whereas complex, deep-seated lesions or emergency trauma cases requiring prolonged ICU care fall toward the higher end.
After a detailed neurosurgical evaluation and review of imaging (CT/MRI), our team provides a personalized treatment plan and a transparent cost estimate based on your condition.
Who might need a craniotomy?
Neurosurgeons may perform a craniotomy for a variety of reasons, such as to diagnose, remove, or treat brain tumours, relieve pressure within the brain, repair skull fractures or a tear in the membrane lining the brain, remove blood clots or blood leaking from blood vessels, remove an abnormal mass of blood vessels, drain an infected pus-filled pocket called an abscess, and to treat epilepsy.
What is the difference between craniotomy and craniectomy?
Craniotomy and craniectomy are both crucial brain surgeries that involve removing part of the skull; however, they differ in how the bone is handled after the surgery. In craniotomy, the surgeon removes a piece of the skull (bone flap) to access the brain and then immediately replaces it with screws or plates. In craniectomy, the surgeon removes the piece of the skull but doesn't replace it immediately, performing follow-up surgery (cranioplasty) weeks or months later to replace that removed part of the skull.
What is decompressive craniectomy?
A decompressive craniectomy is a surgical procedure in which a neurosurgeon removes the portion of the skull and opens the dura to relieve increased pressure that is unresponsive to other treatments, often due to severe swelling or traumatic injury. During this procedure, the surgeon removes a large section of the skull to allow the brain to expand, reduce pressure and improve blood flow to the brain, preventing further damage. The removed bone is typically preserved and may be replaced later.
What will happen to hair after craniotomy procedure?
Usually, only a small area of hair is shaved, and the extent of hair removal depends on the location and size of the incision. Typically, the neurosurgeon will shave only the area directly around the incision site to ensure a clean and sterile environment. After the craniotomy, within a few days, the patient's hair will grow back to where it was shaved. Once the wound on the patient's head has healed and clips or stitches have been removed, it is suggested to get a hair wash and use hair products as usual, as well as dye or treat their hair once the wound heals.
Will a patient have a scar after craniotomy surgery?
If the patient has any surgery, there will always be a scar at the incision site. However, craniotomy scar size may differ based on the surgical approach (including incision size and location) and the extent of the procedure. Neurosurgeons minimize the size of the incision and scarring with an attempt to place the incision in discreet areas wherever possible so that the scar is not obvious.
The scar might be visible immediately after craniotomy or not become noticeable until the patient observes progression of genetic hair loss process. Fortunately, the scalp heals very well, so scars tend not to be that visible. It is very unusual to have an incision on your face, so your facial features should not be affected.
Who performs a craniotomy?
A craniotomy is the common surgical removal of a small portion of the skull bone temporarily to access the brain in order to treat many conditions. A neurosurgeon who specializes in brain and spine surgery performs a craniotomy.
What is an emergency craniectomy?
An emergency craniectomy is a life-saving brain surgery performed by a neurosurgeon to remove part of the skull temporarily to relieve pressure on the brain, which is usually done for a patient who is in critical condition and has experienced a stroke or severe brain damage that could lead to brain death. Other conditions such as swelling, bleeding, aneurysms, high blood pressure, brain tumours, brain infections and excess cerebrospinal fluid will cause pressure on the brain.
What is craniectomy syndrome?
Craniectomy syndrome, also known as the syndrome of the trephined or sinking skin flap syndrome, is an uncommon complication that occurs in patients who have undergone large craniectomies. This syndrome results when atmospheric pressure exceeds intracranial pressure at the site of the craniectomy, leading to displacement of the brain across various intracranial boundaries.
It tends to develop several weeks to several months after surgery. It consists of a sunken scalp above the bone defect with neurological symptoms. If left untreated, this condition can cause neurological deterioration, permanent brain damage, or even be fatal.
What is pterional craniotomy?
The pterional craniotomy, also called frontotemporal craniotomy (ftp craniotomy), is one of the most frequently performed unique surgery that gives wide access to the skull base. It is named after the pterion, where the four bones such as frontal, temporal, greater wing of sphenoid, parietal meets within the skull. This is considered as essential tool for neurosurgeons to access and treat various brain conditions.
What is CSF leak after craniotomy?
A cerebrospinal fluid (CSF) leak is a dangerous complication that may occur after a craniotomy in which CSF escapes through a tear or hole in the dura (the outermost layer that surrounds the brain) due to the injury or puncture during head injury or surgical technique involving the spine, brain or sinuses. If the leakage happens immediately after surgery, the neurosurgeon places a lumbar drain into the spinal fluid space in the lower back to remove extra fluid slowly.
Is craniotomy a major surgery?
Yes, a craniotomy is a major surgery, as it involves brain making an opening in the skull temporarily to access and treat various conditions and replacing an opening with the skull bone.
Craniotomies are performed for many reasons, including removing brain tumours or blood clots, repairing aneurysms, draining brain abscesses, repairing skull fractures and tears in the membrane lining and treating epilepsy.
What is awake craniotomy?
Awake craniotomy, also called awake brain surgery, is a type of technique that allows the neurosurgeon to access the brain while the patient is awake and able to talk in the operative theatre. Initially, it was used for the surgical treatment of epilepsy, but it is commonly performed for the resection of tumours close to regions of the brain that control sensation, language, cognition, and boy movement. This surgery is possible because there are no pain receptors in the brain itself. However, the patient's scalp will be anaesthetized so as not to feel any pain.
How to get an appointment for Craniotomy surgery?
Hyderabad residents seeking 'Craniotomy Procedure near me' can easily schedule an appointment at PACE Hospitals. Simply fill out the 'Request an Appointment for Craniotomy procedure' form above or contact our appointment desk at 04048486868.
Please bring your previous medical records to your appointment. This helps our neurosurgeons thoroughly review your medical history, ensuring you receive the highest standard of care during your craniotomy surgery.




