Mpox (monkeypox) - Symptoms, Causes, Treatment and Prevention
PACE Hospitals
As we almost approach the end of the COVID-19 pandemic, a new viral threat called mpox (formerly monkeypox) has emerged. This zoonotic viral illness has primarily been active in the African continent, with occasional, yet epidemiologically significant, cases reported in other parts of the world.
The World Health Organization (WHO) has reported a multi-country outbreak of human monkeypox, caused by the monkeypox virus (MPXV). Mpox (monkeypox) is currently regarded as a public health emergency of international significance due to its rapid spread and considerable impact, which has sparked concerns of the outbreak of another virus pandemic.
The treatment of mpox is primarily the responsibility of
general physician, who provides supportive care aimed at relieving symptoms and preventing complications. Specialized care may be needed to deal with challenging cases effectively, depending on the severity of the disease.
Definition of mpox (Monkeypox)
Mpox, formerly known as monkeypox, is a rare viral illness caused by the monkeypox virus, which is part of the Orthopoxvirus genus. This genus also includes the variola virus (the cause of smallpox) and the vaccinia virus (used in the smallpox vaccine). Although mpox is less severe than smallpox, it exhibits some similarities in symptoms and transmission.
Mpox (monekypox) meaning
"Monkeypox" combines "monkey," indicating the animal where the virus was first discovered, with "pox," referring to the disease's characteristic pustular skin lesions.
History & Background
It was in the year 1958 when the monkeypox virus was first diagnosed in Denmark, where it was identified in monkeys used for research. The first human case of monkeypox was reported in 1970, involving a nine-month-old boy in the Democratic Republic of the Congo. After the eradication of smallpox in 1980 and the widespread availability of the smallpox vaccine, monkeypox began to emerge more frequently in Central, East, and West African countries. A significant global outbreak occurred in 2022–2023, with cases being reported worldwide despite monkeypox previously being rare outside of Africa.
Globally reported cases
Based on the information released by the World Health Organization, as of June 30, 2024, there were a total of 99,176 confirmed cases of the mpox outbreak, with 208 deaths reported across 116 countries from January 01, 2022. Following the spread of the disease beyond its continent and into neighboring countries, the World Health Organization declared mpox a global public health emergency.
Mpox (monkeypox) cases in India
India has recorded it's first mpox (Monkeypox) case on 09-september-2024 in a 26- year old male from Haryana state. This is the first ever confirmed case of mpox after WHO declaring international health emergency on 14-Aug-2024. The doctors has confirmed it as mpox clade-II variant, which is less fatal and infectious than other variants of mpox.
Mpox (monkeypox) causes
Understanding the causes of mpox involves exploring several aspects, including the virus's origin, transmission pathways, and factors that contribute to its spread. The causes of mpox are segregated into:
- Animal to human (Animal reservoir)
- Human to Human
- Bodily fluids
- Sexual transmission
Animal reservoir: Mpox is a zoonotic virus that is spread from animals to humans. These animals are primarily found in African regions where mpox was previously widely reported. The animal reservoir for mpox includes:
- Squirrels
- Rats
- Monkeys
- Primates
- Pigs
- Mice
Human-to-human: The current epidemic is mainly driven by human-to-human transmission. Transmission occurs through:
-Respiratory droplets
-Fomites (contaminated surfaces)
-Physical contact with infected individual's lesions
- Bodily fluids: Recent analyses indicate high viral loads in bodily fluids as mentioned below:
- Urine
- Saliva
- Semen
- Faeces
- Swabs from the oropharynx and rectum
- Sexual transmission: Sexual transmission is identified as a major driver of transmission in the ongoing epidemic of mpox virus.
Pathophysiology of mpox (monkeypox)
The fate of mpox virus once it enters the human body is as mentioned here:
- Viral entry and replication
- Incubation period
- Symptom onset
- Lesion development
Viral entry and replication
- Viral entry into humans can occur through multiple routes like oropharynx, nasopharynx and intradermal routes.
- The mpox virus then replicates at the site of inoculation.
- The virus then spreads to local lymph nodes.
Incubation period
- Initial viremia occurs, leading to viral spread and seeding of other organs.
- The incubation phase can last up to 21 days, but it usually lasts seven to fourteen days.
Symptom onset
- Secondary viremia leads to the onset of symptoms.
- Prodromal symptoms like fever and lymphadenopathy appear 1 to 2 days before lesions.
- Patients may be contagious during this period.
Lesion Development
- Lesions initially appear in the oropharynx.
- Skin lesions subsequently develop.
- By the time lesions manifest, serum antibodies tend to be apparent.
Mpox (monkeypox) symptoms
The symptoms of mpox are significantly discussed, including the common symptoms and symptoms related to the characteristics of rashes in mpox as mentioned below:
Common Symptoms: Some of the common symptoms found in patients with mpox virus are as mentioned below, and that can appear several days to a few weeks after exposure:
- Fever
- Rashes
- Enlarged lymph nodes
- Chills/tremors
- Headache
- Muscle pain
- Backache
- Fatigue
- Joints pain
Rashes of mpox virus: It is very important to distinguish the rashes due to mpox virus from other rashes. The characteristics of rashes could be:
- A skin rash or mucosal lesions
- Typically lasts 2–4 weeks
- Lesions are often fluid-filled
- Commonly concentrated on the face, mouth or extremities like hands or legs
- During the 2022 outbreaks, more oral and anogenital lesions were reported
Transmission of mpox virus: Understanding the transmission of mpox virus is crucial in preventing or controlling the transmission of the virus further:
- Routes of Transmission
- Physical contact with an infected person
- Contact with contaminated materials or objects
- Communicability
- Mpox is not communicable until symptoms appear
- Easier to control the spread by isolating symptomatic individuals
Phases of mpox (monkeypox)
The mpox (monkeypox) infection has four stages to understand the virulence property of the disease and its impact on patient’s health:
- Incubation phase
- Prodromal phase
- Eruptive Phase
Incubation Phase
People are not contagious during the incubation period. However, healthcare professionals may suggest that people who have been exposed to mpox get vaccinated.
- Duration: Mean of 13 days (range: 3 to 34 days) after primary infection.
- Context: Typically occurs following zoonotic transmission.
Prodromal Phase
Symptom onset is associated with a secondary viremia, resulting in 1 to 4 days of prodromal symptoms like fever and lymphadenopathy before the appearance of lesions. Patients may be contagious during this phase. Lesions initially develop in the oropharynx and subsequently appear on the skin.
- Duration: 1 to 4 days.
- Clinical signs: Some of the key clinical signs of mpox virus that are present in a patient while infected with the disease are:
- High fever
- Headache
- Fatigue
- Lymphadenopathy, particularly in cervical and maxillary regions.
- Lymphadenopathy helps differentiate mpox from chickenpox
Eruptive Phase
The rash typically starts on the face and can spread to other parts of the body, including the palms of the hands and soles of the feet. The rash goes through five stages:
- Duration: 14 to 28 days.
- Lesion Characteristics: Centrifugal (spreading outward from the centre).
- Macules: Flat spots.
- Papules: Raised bumps.
- Vesicles: Fluid-filled blisters.
- Pustules: Pus-filled lesions.
- Scabs: Hard crusts of blood over the sores
Mpox (monkeypox) diagnosis
Due to many similarities between the mpox virus with other viral diseases like smallpox, sexually transmitted diseases, chickenpox etc., proper diagnosis is crucial for early treatment and to prevent further spread.
Real-time polymerase chain reaction
- Rt-PCR, also called real-time polymerase chain reaction, is the preferred method for laboratory testing and is widely used to detect MPXV. PCR testing is highly efficient and sensitive in detecting the presence of viral DNA in patient specimens.
- Specimens can be collected from lesion exudate or scabs. Additional techniques like electron microscopy, immunohistochemistry, IgG and IgM enzyme-linked immunosorbent assays (ELISA), and virus isolation might be helpful as well in diagnosing mpox
- The best diagnostic specimens are collected directly from the rash, including skin, fluid, or crusts, by vigorous swabbing.
- In case skin lesions are not present, the diagnostic process can be performed using oropharyngeal, anal, or rectal swabs.
- Testing blood for mpox is not recommended.
- Antibody detection methods are generally not useful, as they cannot distinguish between different orthopox viruses.
Differential diagnosis
Differential diagnosis of mpox (monkeypox) involves distinguishing it from other diseases with similar symptoms. Here’s a detailed look at the conditions that need to be considered:
Smallpox
Similarities: Both the smallpox and mpox viruses causes fever, rashes, and swollen lymph nodes with similar rash distribution
Differences: Smallpox lesions are uniform in size and umbilication, unlike mpox lesions. Moreover, Smallpox rash often progresses in a synchronous manner (all lesions are at the same stage).
Chickenpox (Varicella)
Similarities:
- Both can present with fever and a vesicular rash.
- Lesions can be found on the face and trunk.
Differences:
- Chickenpox lesions appear in crops, with new lesions appearing as older ones crust over, resulting in different stages coexisting.
- Lesions in chickenpox are more superficial and less uniform, whereas they are deeper and randomized in mpox.
- Lymphadenopathy is not a common feature in chickenpox, but most commonly seen in mpox.
- Chickenpox is more common in children, whereas mpox can affect all age groups.
Herpes Simplex Virus (HSV)
Similarities:
- Vesicular rash, especially on or around the mouth or genital areas.
- May present with fever and localized lymphadenopathy.
Differences:
- HSV lesions are typically grouped vesicles on an erythematous base.
- Recurrent infections are common with HSV, which is not typical for mpox.
- HSV usually affects localized areas, whereas mpox has a more widespread rash.
Syphilis
Similarities:
- Can present with a generalized maculopapular or pustular rash.
- Rash can involve palms and soles, similar to mpox.
Differences:
- Syphilis rash is more diffused and not vesicular.
- Syphilis presents with other symptoms like mucosal lesions (e.g., condyloma lata), systemic symptoms, and lymphadenopathy, but not as pronounced as in mpox.
- A history of exposure to Treponema pallidum (causative agent of syphilis) through sexual contact not observed in mpox
Coxsackievirus (Hand, Foot, and Mouth Disease)
Similarities:
- Both mpox and coxsackievirus causes rashes and can involve mucosal lesions.
Differences:
- Coxsackievirus often causes rash on the hands, feet, and mouth, with a distinctive pattern. Lesions are usually not as fluid-filled or widespread as in mpox.
Rickettsial Infections
Similarities:
- Can present with fever and a maculopapular or petechial rash.
- Rash can include palms and soles.
Differences:
- Rash in rickettsial infections is not vesicular or pustular as in mpox.
- Associated with tick exposure, history of outdoor activities, and other symptoms like severe headache and myalgia unlike mpox
HIV/AIDS
Similarities:
- Early HIV infection can present with fever and rash similar to the mpox virus.
Differences:
- HIV rash is typically less vesicular and may be associated with other systemic symptoms like weight loss or opportunistic infections. History of high-risk behaviours or exposure to HIV.
Impetigo
Similarities:
- Can cause vesicular lesions, particularly in children.
Differences:
- Lesions are usually honey-crusted and localized around the nose and mouth unlike mpox
- Impetigo is caused by bacterial infection (Staphylococcus or Streptococcus) and does not cause systemic symptoms, whereas mpox is a viral infection.
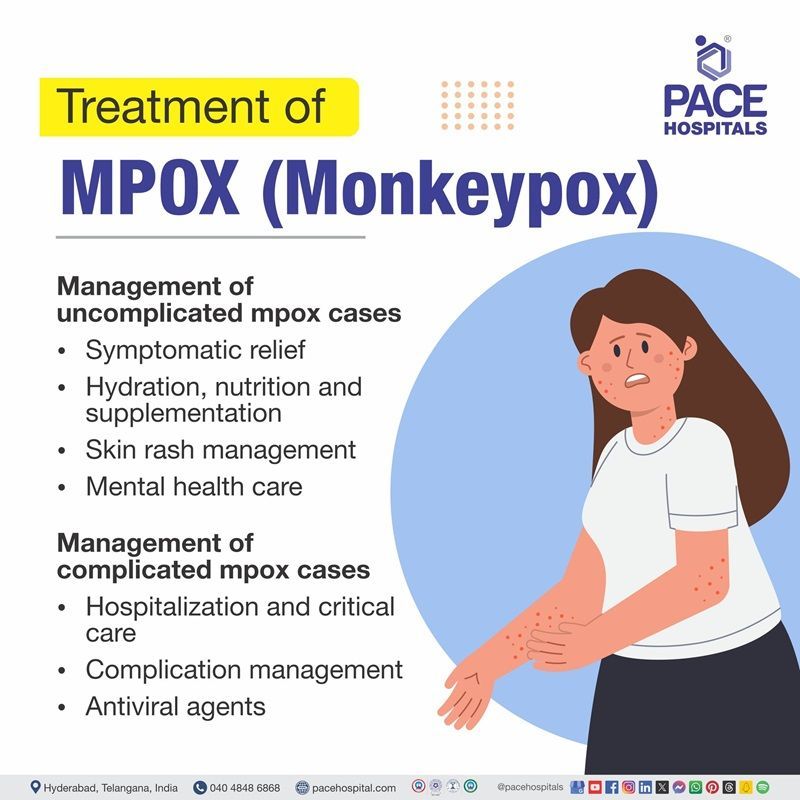
Mpox (monkeypox) treatment
Mpox (monkeypox) infections are often self-limiting, and supportive care is typically recommended. Individuals at low risk for severe symptoms can isolate themselves at home. Healthcare personnel should assess each case individually to make sure that prevention of disease prevention and related control measures can be adequately implemented in the home environment.
Management of uncomplicated mpox cases
The management of uncomplicated or low-risk mpox patients should be:
- Symptomatic relief
- Hydration, nutrition and supplementation
- Skin rash management
- Mental health care
Symptomatic Relief: Symptomatic medications can be prescribed based on the patient's condition, such as antipyretics, analgesics, or antiemetics.
Hydration, Nutrition, and Supplementation: Adequate hydration, a review of vaccinations, and a nutritional assessment should be prioritized, especially for pediatric patients. Vitamin A supplementation may benefit patients with deficiencies due to its role in wound healing.
Skin rash management: Mild skin rashes can be treated with supportive care to reduce irritation and promote healing. If a secondary bacterial infection is suspected, antimicrobial agents targeting Streptococcus pyogenes or Staphylococcus aureus are recommended. Complications like cellulitis, necrotizing soft tissue infections, or abscesses should be closely monitored and treated.
Mental health care: Psychological support is essential for patients with monkeypox, as long-term isolation can lead to anxiety and depression.
Management of complicated mpox patients
High-risk groups include children (especially those under eight years old), pregnant women, immunocompromised individuals, and those with poor skin integrity, such as atopic dermatitis. Management in them should be done as mentioned below:
- Hospitalization and critical care
- Complication management
- Antiviral agents
Hospitalization and critical care: High-risk patients should be hospitalized for monitoring and may require antiviral treatment. Confluent rashes or more than a hundred skin lesions are indicators of severe disease and may warrant hospitalization.
Complication management: Patients with progressive illness or complications should be treated aggressively. Potential complications include severe dehydration from gastrointestinal loss, pneumonia, encephalitis, sight-threatening ocular lesions, and sepsis. These complications may require the use of antiviral agents and targeted treatments.
Antiviral agents: Currently, there is no specific treatment for monkeypox. However, several antiviral drugs approved for treating smallpox or other orthopoxviruses have been repurposed for managing monkeypox infections.
- VP37 Envelope Wrapping Protein Inhibitor: This antiviral drug class can treat smallpox, monkeypox, and cowpox, which are all caused by viruses in the orthopox virus family. It works by preventing the virus from being transmitted between cells, which stops the disease. However, this orthopox virus VP37 envelope wrapping protein inhibitor drug class is currently available for the treatment of mpox under specific circumstances, especially during outbreaks or in cases where traditional therapies may not be effective or available.
Complications of mpox (monkeypox)
People with mpox can become very sick. Realizing the complications of monkeypox virus is important in managing the disease better. Some of the majorly seen complications associated with monkeypox virus are as mentioned below:
- Dermal infection
- Lifelong Scarring of the Skin
- Insufficient or excessive pigmentation
- Chronic damage to the cornea, leading to vision loss
- Respiratory tract infections like pneumonia
- Fatigue and dehydration (due to vomiting, diarrhea, painful oral sores reducing oral intake, and insensible fluid loss from disturbance of the skin all over the body.)
- Sepsis
- Death in extreme cases
- Encephalitis
Mpox (monkeypox) Prevention
Mpox can be transmitted through contact with respiratory secretions, open wounds, or contaminated objects. It can also spread through prolonged exposure to aerosols from an infected person. Here are some ways to prevent the spread of mpox, also known as mpox:
- Get vaccinated: Some countries recommend mpox vaccines for people at risk, though they are currently in limited supply. The patients can check with their general physician to see if the vaccine is recommendable to them.
- Avoid close contact: Should not touch people with a rash that looks like mpox, or touch items that have been used by an infected person or animal. This includes blankets, bedding, and clothing.
- Wash your hands: People should wash their hands with soap water or can use an alcohol-based hand sanitizer after getting in touch with an infected person or animal, before eating and after using the bathroom.
- Avoid contact with animals: It is recommended to stay away from animals that may be infected, such as rodents and primates.
- Precautions during sex: People should be aware of precautions to lower the risk of mpox during intercourse as the recent outbreak has evidence of sexual contact as one of the causes of Mpox.
Frequently Asked Questions (FAQs) on Mpox (Monkeypox)
How does mpox (monkeypox) spread?
Mpox (formerly monkeypox) is primarily transmitted through direct contact with infected secretions, lesions, or bodily fluids from infected individuals or animals. It can also spread via contaminated objects and possibly through respiratory droplets.
What are the common symptoms of mpox (monkeypox)?
Common symptoms of mpox (monkeypox) include fever, rash, swollen lymph nodes, headache, muscle aches, and backache. The rash usually progresses from flat spots to raised bumps and then to pus-filled blisters before scabbing over.
How is mpox (monkeypox) diagnosed?
Mpox (monkeypox) is diagnosed through polymerase chain reaction (PCR) testing of samples from skin lesions, fluid, or scabs. PCR testing is the most reliable method for confirming the presence of viral DNA.
Is there a vaccine available for mpox (monkeypox)?
While there is no specific vaccine for mpox (monkeypox), smallpox vaccines may offer some protection due to the similarity between the two viruses. However, availability and recommendations can vary by region.
What treatments are available for mpox (monkeypox)?
There is no specific antiviral treatment for mpox (monkeypox). Supportive care, such as hydration, pain management, and wound care, is recommended. Antiviral drugs used for smallpox may be repurposed in severe cases.
What is mpox and how does it differ from smallpox?
Mpox (monkeypox) is a zoonotic viral disease caused by the monkeypox virus, which is related to the smallpox virus but generally less severe. Unlike smallpox, monkeypox has a lower mortality rate and is less transmissible between humans.
How long is the incubation period for mpox?
The incubation period for mpox (monkeypox) typically ranges from 5 to 21 days after exposure to the virus. This period is the time between exposure to the virus and the appearance of symptoms.
Can mpox be sexually transmitted?
Recent evidence suggests that mpox (monkeypox) may be transmitted sexually, particularly as seen in recent outbreaks among men who have sex with men (MSM). However, more research is needed to fully understand this mode of transmission.
What preventive measures should be taken to avoid mpox?
Preventive measures include avoiding contact with infected individuals or animals, practising good hygiene, using personal protective equipment if necessary, and following public health advisories.
How long should a person with mpox isolate themselves?
Isolation should continue until symptoms have resolved and there is no longer a risk of transmitting the virus to others. The duration of isolation may vary based on guidance from medical experts.
What are the potential complications of mpox?
Potential complications of mpox include secondary bacterial infections, severe dehydration, pneumonia, encephalitis, and sight-threatening ocular lesions. Severe cases require prompt medical intervention and management.
How is mpox managed in high-risk populations?
High-risk populations, such as young children, pregnant women, and immunocompromised individuals, should be closely monitored. Hospitalization and specialized care may be necessary for severe cases in these groups .
What role does vitamin A play in mpox treatment?
Vitamin A supplementation may aid in wound healing, especially in patients with vitamin A deficiencies. Its use should be guided by medical experts based on individual patient needs.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles