Anal fistula - Fistula in ano: Symptoms, Causes, Types, Complications, Prevention
Pace Hospitals
Fistula in ano or Anal fistula meaning
The term fistula often refers to an abnormal connection between two parts, which may be an organ or blood vessel to another structure.
An abnormal tube or passage that often develops from the anus to the skin on the outer anal region is known as an anal fistula or fistula in ano or anorectal fistula. The anal glands, which are in the top portion of the anus (butthole), are where it often develops. When the glands are infected, the infection can develop a fistula due to drainage. A perianal abscess is the medical term for this infection. (An anal fistula may also be known as a perianal fistula. "Perianal" refers to the area around your anus).
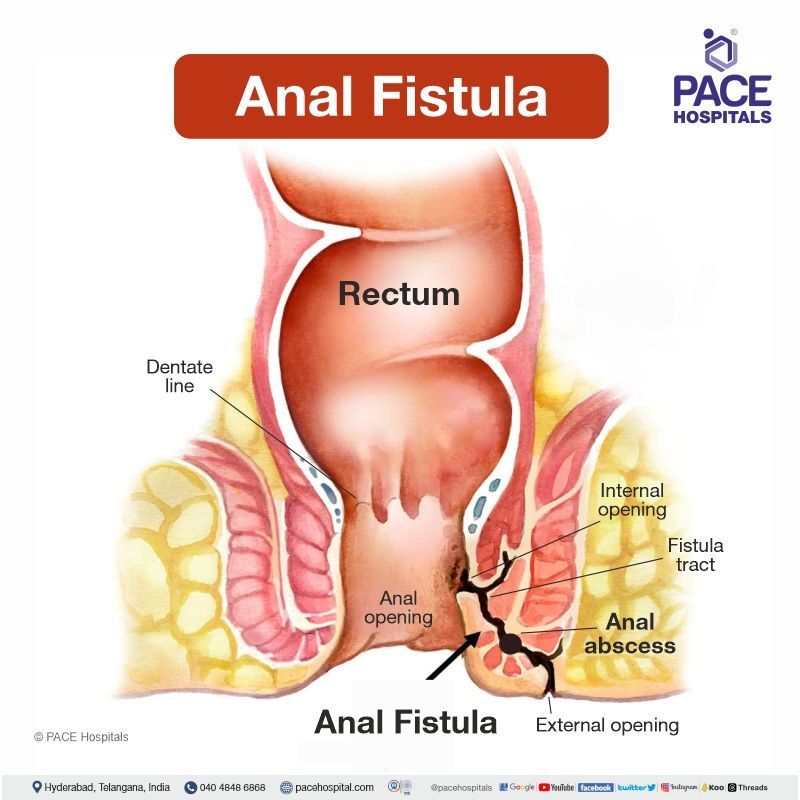
Anal fistula definition
The anal canal in the colon and the skin of the buttocks are connected by an abnormal tunnel called an anal fistula. The majority of anal fistulas or fistulas in ano arise in response to an anal gland that has been infected with pus (abscess).
Incidence of anal fistula (fistula in ano)
An anal fistula or fistula in ano is common in men when compared to that of women. It is usually developed in 12.3 cases per 100,000 men and 5.6 cases per 100,000 women. It is most commonly seen in the age group between 20-40 years.
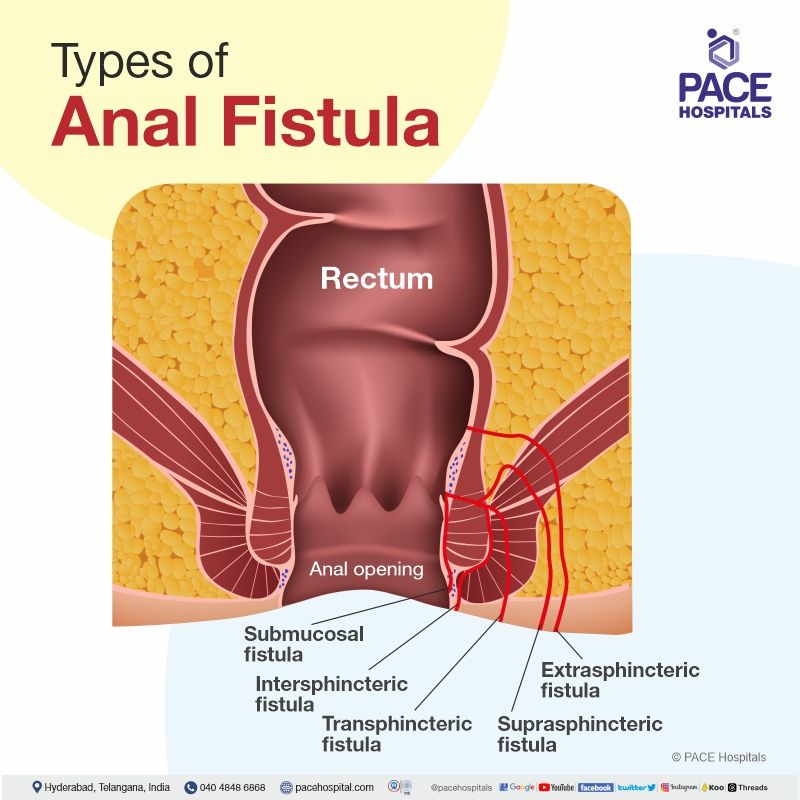
Anal fistula types
Usually, anal fistulas are classified based on the anatomy in relation to the sphincter complex. The types of anal fistula or fistula in ano are as follows:
- Intersphincteric fistula: This is the common type of anal fistula and occurs in 45% of all fistula cases; in this condition, the fistula infiltrates through the internal sphincter but leaves the external.
- Transphincteric fistula: Comprises 30% of total fistula cases; fistula passes through internal and external sphincters in this condition.
- Suprasphincteric fistula: Comprises 20% of total fistula cases; here, in this type, the fistula penetrates through the internal sphincter and extends superior in the planes between sphincters and passes above the external sphincter before to perineum. This condition includes a horseshoe abscess.
- Extrasphincteric fistula: This condition is very rare and comprises 5% of total cases; it forms a connection between the rectum and perineum that extends laterally to both the external and internal sphincters. This condition is very hard to treat because this condition needs the preservation of the sphincter complex.
- Subcutaneous or submucosal fistula: In this condition a perianal fistula can be superficial and short, without affecting the anal sphincter.
Anal fistula symptoms
The symptoms of anal fistula or fistula in ano are as follows:
- Swelling and pain around the anal region
- Fever and Chills
- Feeling sick and tired
- Soreness, redness or itching at the anal opening
- Drainage associated with pus at the anal opening
Anal fistula causes
The causes of anal fistula or fistula in ano include:
- Peri anal abscess
- Inflammatory conditions such as Crohn’s disease, diverticulitis
- Radiation therapy
- Anal STIs (sexually transmitted infections)
- Hidradenitis suppurativa (chronic inflammatory skin disease)
- Anus affected by tuberculosis
- Surgical complication near the anus
Anal fistula risk factors
The risk factors for anal fistula or fistula in ano are as follows:
- Anal gland obstruction: obstruction in the anal gland allows the bacteria that lead to infection, resulting in the perianal abscess (formation of pus in the anal region).
- History of surgery or radiation therapy at the site of the anal region: Radiation proctitis requires surgical intervention, and it is a common complication of developing a fistula.
- Obesity: Obese patients are more possibly to experience failure or recurrence following surgery for complex anal fistulas.
- Diabetes: Poor glycaemic control has the risk of developing perianal abscess in diabetic patients and may lead to fistula formation.
- Smoking: Anal abscess or fistula is influenced by inflammatory conditions associated with smoking.
- Sedentary lifestyle: Hyperlipidaemia and a diet that lacks fibre and deep-fried foods may lead to anal fistula.
- History of perianal abscess: Infections to the glands due to obstruction lead to perianal abscess. These glands are located at the level of the dentate line.
- Inflammatory bowel diseases: When inflammation causes sores or ulcers to grow on the inside wall of the gut or adjacent organs, fistulas arise. Ulcers can grow through the entire gut wall thickness, forming a tunnel to drain pus from the infected area.
- Chronic STIs: Sexually transmitted infections cause anal itching due to viruses, thereby developing the Anorectal diseases.
Anal fistula complications
If the anal fistulas or fistulas in ano are untreated, they may cause some possible complications such as:
- Persistent infection: The fistulas due to an abscess or infection may feel like they had gone away from the site where it originated, but recurring infection may occur by forming a new abscess in some cases.
- Fistula extension: This condition of chronic fistulas extends to new directions and forms new branches, resulting in complex fistulas. These complex fistulas are hard to treat.
- Anal cancer: Chronic or long-lasting fistulas lead to anal cancer due to the risk of inflammation and erosion.
- Fistula recurrence and faecal incontinence: This condition occurs due to the removal of the sphincter.
- Anorectal infections and sepsis: These are the conditions initiated by Crohn's disease, which is caused due to fistula, abscess, ulcers and skin tags.
Anal fistula diagnosis
The diagnosis of anal fistula or fistula in ano includes:
- Physical rectal examination
- Digital rectal examination
- Fistula probe
- Anoscopy
Imaging techniques such as:
- CT pelvis
- CT fistulography
- MRI of pelvis
Laboratory findings such as:
- CBC (Complete blood picture count)
- CRP (C-reactive protein)
Anal fistula treatment
Treatment for an anal fistula or fistula in ano typically depends on its severity, location, and the underlying cause. Here are some common approaches to anal fistula or fistula in ano treatment:
- Conservative Management: For simple and superficial fistulas, especially those that don't cause significant symptoms, your doctor might recommend conservative management. This involves keeping the area clean, using warm water soaks or sitz baths, and ensuring proper hygiene.
- Medical management
- Fibrin plug and glue (anal fistula plug)
- LIFT (ligation of intersphincteric fistula tract)
- Seton placement
- Endorectal advancement flap
- Fistulotomy
- Fistulectomy
- VAAFT (video-assisted anal fistula treatment)
Anal fistula prevention
The following lifestyle modifications can do anal fistula or fistula in ano prevention. This includes anal fistula diet, anal fistula medicine, and anal fistula home treatment.
Anal fistula diet:
- Fibre-rich foods for fistula, such as cereals, fruits, vegetables, and whole grain bread, makes the stool pass easier.
- Drinking plenty of water and fluids keeps the patient hydrated, preventing hard stools.
- Taking fibre supplements such as ispaghula, methylcellulose, bran, or sterculia helps to prevent constipation.
- Avoid too much alcohol and caffeine.
Anal fistula medicine:
- OTC (over-to-counter) medications, such as topical ointments with analgesics and corticosteroids, and antibiotics are used to treat the symptoms of anal fistula.
- Avoid painkillers that may cause constipation.
- Taking stool softener or bulk laxative when needed.
Anal fistula home remedies:
- Soaking the anal region in warm water 3 to 4 times a day.
- Wearing the pad over the anal region until the fissure heals.
- Taking a sitz bath (a warm or shallow bath) once a day gives the smoothening effect near the anal site and promotes healing.
- Application of dressings at the site of wounds that collects the drain and also the patient should keep hygiene and change the dressings regularly.
- Maintain a healthy weight and do some regular exercises to get relief.
Anal fistula vs Piles | Difference between anal fistula and piles
An anal fistula or anorectal fistula is an abnormal passage or tunnel that usually arises from the inside of the anal canal to the skin outside of the anus. In contrast, piles are the vascular spaces (fleshy, swelling-like structures) that form cushions above or inside the anal canal. Some of the differences between anal fistula and piles are as follows:
| Characteristics | Anal Fistula | Piles/Hemorrhoids |
|---|---|---|
| Symptoms | Swelling, pain, fever, chills, tiredness, feeling sick, redness or itching, soreness, and discharge associated with pus. | Rectal bleeding, pain, bright red stools with blood, anal itching, one or more lumps with tenderness, anal pain on sitting. |
| Causes | Peri anal abscess, inflammatory conditions such as Crohn's disease, diverticulitis, radiation therapy, anal STIs (sexually transmitted infections), hidradenitis suppurativa (chronic inflammatory skin disease), surgical complication near the anus, sedentary lifestyle etc. | Constipation, chronic cough, pregnancy, prolonged sitting, overweight, straining to pass stool, dehydration, eating low fibre diet etc. |
| Complications | Persistent infection, fistula extension, anal cancer, faecal incontinence, anorectal infections etc. | Thrombosed piles, anal skin tags, anal stenosis etc. |
| Prevention | Take a fibre-rich diet, plenty of liquids, sitz baths, and fibre supplements. | Take a fibre-rich diet, drink a lot of water and liquids, avoid sitting continuously on toilets and hard surfaces, take fibre supplements, maintain a healthy weight, exercise, etc. |
| Treatment | Medical management and surgeries like fistulectomy, fistulotomy etc. | Medical management and various treatment procedures like rubber band ligation, injection sclerotherapy, haemorrhoidectomy, stapled haemorrhoidopexy etc. |
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868











