Mastectomy Surgery - Types, Procedure Indications, Recovery & Cost
At Pace Hospitals, state-of-the-art advanced operation theatre is equipped with world-class robotic surgery and 3D HD laparoscopic equipment to perform minimally invasive major and supra-major breast cancer surgery.
Our team of the surgical oncologist, one of the best breast cancer surgeons in Hyderabad are having more than 35 years of extensive experience in performing mastectomy surgery for breast cancer treatment.
Request an appointment for Mastectomy Surgery
Mastectomy Surgery - appointment
- Why choose us -
250+ Mastectomy Surgery Performed
Advanced 3D HD Laparoscopy Unit
Team of the Best Breast Cancer Surgeon
All insurance and TPAs accepted
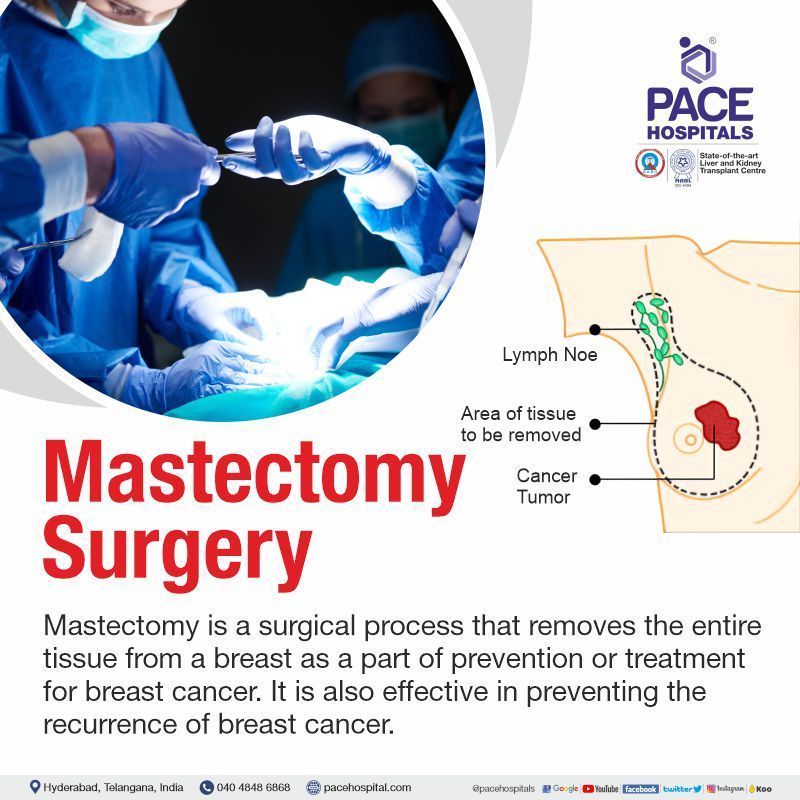
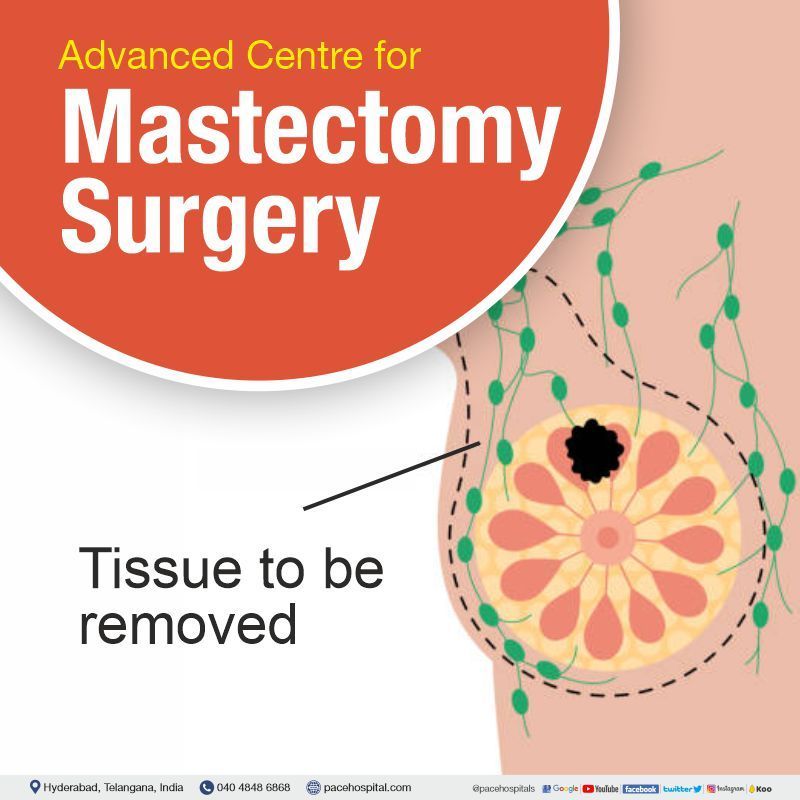
What is Mastectomy Surgery and its purpose?
Mastectomy meaning
Mastectomy is a surgical process that removes the entire tissue from a breast as a part of prevention or treatment for breast cancer. It is also effective in preventing the recurrence of breast cancer.
Initially, the standard treatment for breast cancer was a radical mastectomy, which included the removal of the entire breast, lymph nodes in the underarm, and portions of the chest muscles behind the breast. The selection of the type of mastectomy depends on age, general health, size, grade, and stage of the tumour, the tumour’s hormone receptor status, and involvement of lymph nodes.
However, medical innovation has increased patients' alternatives more than ever. Many patients now have access to breast conserving surgery (BCS or lumpectomy) which require less surgical intervention over Mastectomy procedure.
Types of Mastectomy Surgery
Depending on the surgical technique used and the amount of breast tissue removed, mastectomy surgery can be classified into:
- Total mastectomy (simple mastectomy)
- Double mastectomy (bilateral mastectomy)
- Skin-sparing mastectomy
- Nipple-sparing mastectomy
- Modified radical mastectomy
- Radical mastectomy
- Extended radical mastectomy
1. Total mastectomy or Simple mastectomy
In this procedure, the breast cancer surgeon removes the entire breast, including the nipple, areola, fascia (covering) of the pectoralis major muscle and skin. A few underarm lymph nodes might be removed as part of a sentinel lymph node biopsy, depending on the patient’s situation.
2. Double mastectomy or Bilateral mastectomy
A double mastectomy, or bilateral mastectomy, is one in which both breasts are removed. Women with a BRCA (BRCA1 and BRCA2) gene mutation, who have an extremely high risk of developing breast cancer, may undergo a double mastectomy as a preventative measure.
3. Skin sparing mastectomy
The skin of the breasts is not removed during a skin-sparing mastectomy, but the breast tissue (same as in terms of the amount of breast tissue that is removed during a simple mastectomy), nipple and areola are removed. It is also possible to perform a sentinel lymph node biopsy. After a mastectomy, breast reconstruction can be done the same day using implants or donor tissue from other parts of the body. Skin-sparing mastectomy can be an effective treatment option when the tumour is small or moderate in size and close to the skin's surface.
4. Nipple sparing mastectomy
It is similar to skin-sparing mastectomy, but only the breast tissue is removed (and not the skin, nipple, or areola).
5. Modified radical mastectomy
The entire breast is removed, similar to a total mastectomy. Some of the lymph nodes under the arm (axillary lymph nodes) are also removed as breast cancer often spreads to these lymph nodes and then it spreads to other parts of the body.
6. Radical mastectomy
In Radical mastectomy, the pectoral (chest wall) muscles under the breast, along with the axillary (underarm) lymph nodes, nipple, areola, and the overlying skin will be removed in this process. If the tumour has spread into the pectoral muscles, this procedure may be necessary. This procedure used to be quite common, but now that less invasive procedures (modified radical mastectomy) have proven to be effective with fewer side effects, they are being preferred.
7. Extended radical mastectomy
Extended radical mastectomy was the most extensive procedure used to treat breast cancer as a primary treatment. It is the combination of full-thickness parasternal chest wall excision and removal of internal mammary nodes with a classic radical mastectomy. By eliminating all lymphatic drainage channels in the breast region, this procedure aims to eradicate the cancer and prevent its spread.
What to expect before a mastectomy surgery?
The primary care physician or nurse will inform the patient regarding when the patient needs to check into the hospital. The surgeon will be explaining the procedure to the patient and an inform consent form will be provided to sign, allowing the surgeon to proceed with the surgery. The patient should make sure to read the form thoroughly and clarify any questions before signing.
The surgeon will be asking a few basic questions about the patient’s health condition. A physical examination, blood tests and other surgery related tests will also be performed. This is done so that the surgeon knows the patient is in good or favourable condition before performing the operation.
As a part of surgery preparation, the patient will be informed to abstain from eating and drinking for a specified period of time (8 to 12 hours) and to follow the specific instructions of the surgeon.
The patient needs to inform the surgeon related to:
- Pregnancy status (pregnant or expecting to be).
- Any known allergies to drugs, latex, tape, or anaesthesia (local and general).
- Family history of bleeding disorders.
- Intake of medications, including over-the-counter, vitamins, herbs, and other dietary supplements. If the patient is currently on hormone replacement therapy and/or blood thinning agents, or anticoagulants, or any other medications (prescribed), that could affect the patient’s blood clotting procedure. These medications should be stopped before surgery or as per the surgeon’s or concerned physician’s (who prescribed) advice.
- If it is planned to have reconstructive surgery along with mastectomy, it should be discussed with the surgeon and plastic surgeon prior to mastectomy surgery.
If the patient had planned for radiation therapy after surgery, the patient should schedule an appointment with a radiation oncologist before the surgery to weigh the pros and cons of radiation therapy and find out how it will affect the patient’s breast reconstruction options after undergoing surgery.
Depending on the patient’s specific health situation, the surgeon might give other specific instructions to follow.
What happens during a mastectomy surgery?
A mastectomy procedure typically requires a hospital stay and usually carried out while the patient is under general anaesthesia and completely unconscious.
When no reconstruction is involved, a mastectomy can be performed in one to three hours. A double mastectomy will require more time in surgery and may necessitate an extra day stay in the hospital. After a mastectomy, if the patient (women) opts for breast reconstruction surgery, which is a long procedure, it can add a few more days to the patient’s recovery time in the hospital.
Generally, a mastectomy follows this process:
- The patient will be provided with a gown to change the dress.
- The patient will be inserting with an intravenous line into the arm or hand, through which medications and sedative will be administered.
- The patient will be made to lie on their back on the operating table. During surgery, the patient’s vital signs (heart rate, blood pressure, breathing rate, and blood oxygen level) will be monitored.
- A sterile solution will be used to clean the area of the operated skin.
- The surgeon starts the procedure by making an elliptical incision around the patient’s breast. Depending on the type of mastectomy, a specific incision type may be used.
- Breast tissue and other breast features will be removed as well, depending on the surgical method chosen. After the breast or breast tissue has been removed, the lymph nodes may also be taken out.
- The removed tissue and lymph nodes will be sent for laboratory analysis for the examination. The plastic surgeon will be coordinating with the breast surgeon, if the patient’s breast reconstruction has been scheduled along with mastectomy.
- Temporary tissue expanders are one of the breast reconstructions options where it will form a new breast mound. Temporary tissue expanders may be placed in the chest to support the breast skin for women who will undergo radiation therapy after surgery.
- The surgeon will be inserting one or more tiny plastic tubes (mastectomy drains) at the site of breast removal. Any fluids that build up after surgery can be drained away through these tubes, where they are stitched into place and the ends are connected to a drainage bag.
- The surgical area will be closed with stitches or adhesive strips and the area will be covered with a sterile bandage or dressing.
What to expect after a mastectomy surgery??
After having a mastectomy, depending on the type of mastectomy surgery and the involvement of the breast reconstruction process, the patient needs to stay for a few more days in the hospital. In some cases, chemotherapy or radiation therapy may be required after a mastectomy, which is further advised by the physician.
After the surgery, the patient can expect to:
- The patient will be taken into a recovery room once their vital signs (heart rate, respiration rate, and blood pressure) are stabilised.
- The patient might feel pain, a pinching sensation, and numbness at the underarm location after the removal of sedation.
- Depending on the type of surgery and the patient's condition, the patient has to stay in the hospital. The patient will have a scar at the mastectomy site and also have a pulling feeling near or under the arm after surgery.
The physician will provide specific instructions related to incision, drain care, signs of infection, and dressing at the time of discharge such as:
- When there is an infection at the site of the procedure, what should be done or to whom should be contacted?
- How to replace a wet dressing with a clean one after having a bath?
- When and how often must the drain be emptied per day, and how to do so?
- When to start using the arm again and how to do arm exercises to prevent stiffness?
- When to begin wearing inner garments (mastectomy bra) and the type of prosthesis to be used?
- When to resume the old medication, which was stopped because of surgery and usage of medications for pain management and infection control?
- Follow-up visits.
Breast Reconstruction after Mastectomy Procedure
Breast reconstruction surgery is an option for many women who undergo a mastectomy surgery (the surgical removal of a breast for the purpose of treating or preventing breast cancer). It can be done along with the mastectomy surgery (post-surgery) or later (delayed reconstruction) after the breast cancer treatment is over and the incisions from the mastectomy have healed. The breast reconstruction is majorly performed with nipple-sparing mastectomy, as the patient’s breast skin is saved in this process.
Many different approaches exist for women who want to undergo breast reconstruction. Saline or silicone implants can be used to reconstruct the breasts. Autologous tissue reconstruction is another option where tissue is taken from another place in the patient’s body to form a breast shape. The tissue-based approaches include transverse rectus abdominis myocutaneous flap (TRAM), latissimus dorsi flap, and the deep inferior epigastric perforator flap (DIEP). When reconstructing the breast, the physician might sometimes use both implants and the patient's own tissue.
If the nipple and areola were removed during the mastectomy, they may be re-created on the reconstructed breast as a final step in breast reconstruction. In order to achieve symmetry between the breasts, breast reconstruction procedures may also be performed on the opposite breast.
The implants are placed in a two staged process:
Stage 1: After a mastectomy, the surgeon will insert a tissue expander under the patient's skin or directly into the chest muscle to help the patient regain breast volume. At periodic doctor's visits after the surgery, the expander is gradually filled with saline.
Stage 2: After 2 to 6 months of mastectomy, as soon as the chest tissue has healed and softened, the expander is taken out and an implant is replaced. In some cases, the implant will be placed while the patient is having mastectomy surgery without placing a tissue expander.
Arm care after lymph node removal
Radiation therapy for breast cancer frequently involves the removal of nearby axillary lymph nodes (either some or all). This disrupts the flow of lymph, which can lead to swelling. Injury to the patient's arm may put them at greater risk for infection. Having surgery near the armpit also increases the risk of developing a blood clot in the armpit veins.
After the removal of lymph nodes, there are ongoing precautions the patient must take for the rest of their life, such as:
- No injections or intravenous lines were inserted into the patient’s arm.
- Patients should pay close attention to the guidance given regarding arm exercises.
- When carrying heavy luggage, the patient should not strain their weaker arm or shoulder; instead, use both hands.
- For lymphatic drainage, raise the affected arm so that the hand is above the elbow.
- The patient should not step outside under the hot sun.
- No blood pressure readings should be taken from the affected arms.
- The patient should keep the affected arm free from harm, such as cuts and splinters and should also wear gloves before doing any work that could cause a cut, such as working with harsh chemicals like detergents or household cleaners.
- The patient should avoid wearing tight clothing on the injured arm, such as elastic wristbands, tight watches, and other jewellery.
- Patients should shave their armpits with a clean razor.
- The physician might give the patients other instructions, depending on their situation.
Complications of mastectomy surgery
Possible complications of mastectomy surgery include:
- Temporary breast swelling
- Pain in the breasts
- Wound infection or bleeding
- Formation of scar tissue at the wound site (incision)
- Arm swelling (lymphedema) after lymph node removal
- Shoulder stiffness and pain
- Surgical site blood clot formation (hematoma)
- After modified radical mastectomy or breast conserving surgery, the breast may contain clear fluid (seroma) in the dead space of the post-mastectomy skin flap, axilla, or breast.
- Suffering from depression and a feeling of loss of sexual identity.
- Risk of local recurrence (5-10%), incisional dog ears and mastectomy skin flap necrosis for total mastectomy.
Mastectomy vs Lumpectomy | Difference between lumpectomy and mastectomy
A lumpectomy, followed by radiation therapy, is an option for breast cancer patients who don't want to have both breasts amputated (mastectomy).
| Elements | Mastectomy | Lumpectomy |
|---|---|---|
| Definition | The surgeon removes the entire breast tissue and possibly a few lymph nodes under the arm. Mastectomy is more invasive. | The only part of the breast that has cancer and a small amount of healthy tissue around it are removed by the surgeon. When compared to mastectomy, lumpectomy is less invasive. |
| Local recurrence | Low chances of local reoccurrences. | Higher risk of developing a local recurrence of the cancer after surgery. |
| Radiation therapy | Radiation therapy is not mandatory following mastectomy surgery. | Patient need to have radiation therapy (5 or 6 weeks) post lumpectomy for five days a week. In the event of a recurrence (same cancer, or of a new cancer) in the same breast after lumpectomy, further radiation would be harmful. |
| Safety | Presence of post-surgery side effects and a longer recovery time. | Compared to mastectomy, it has a short recovery time with fewer post-surgery side effects. |
| Indication | Early-stage breast cancer (Stage I and II), Locally advanced (Stage III) and inflammatory breast cancer after chemotherapy, Ductal carcinoma in situ (DCIS), or non-invasive breast cancer and Paget's disease | Benign breast lumps, such as fibroadenoma or phyllodes, Depending on the size of the lesion, ductal carcinoma in situ or invasive breast cancer that can be treated without removing the breast. |
Explore the mastectomy cost as per the types
How much does a mastectomy cost in India?
The average cost of mastectomy surgery in India is approximately Rs. 1,78,000 (one lakh seventy-eight thousand only). However, mastectomy cost in India may vary depending upon the different hospitals in different cities.
A mastectomy surgery cost in Hyderabad ranges vary from Rs. 1,25,000 to Rs. 1,58,000 (one lakh twenty-five thousand to one lakh fifty-eight thousand). However, cost of mastectomy surgery depends upon the multiple factors such as type of the breast cancer, selection of room for hospital stay and corporate, Central Government Health Scheme (CGHS), ESI, Employee And Journalist Health Scheme by Telangana State Government, EHS or insurance approval for cashless facility.