Piles Operation - Types & Cost
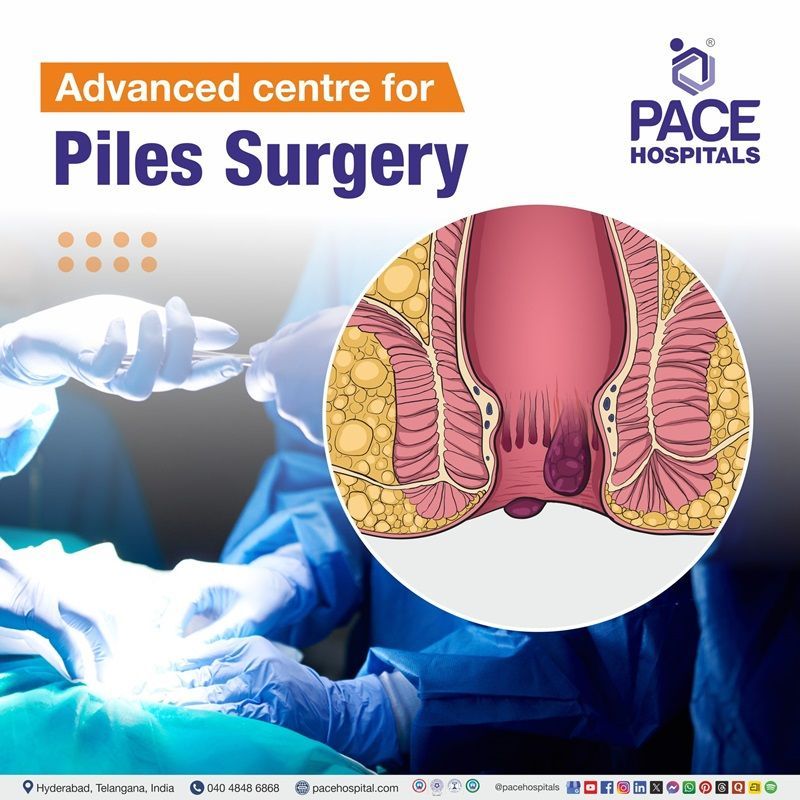
PACE Hospitals is one of the best hospital for piles surgery in Hyderabad, India. With state-of-the-art OT, 3D HD Laparoscopic and laser system, latest technology that ensures the surgery is performed safely and effectively.
Department of Proctology has a team of experienced piles specialist doctors – surgical gastroenterologist, proctologist to perform wide range of piles surgery, including:
- Hemorrhoidectomy
- Stapled hemorrhoidopexy
- Laser hemorrhoidectomy
Request an Appointment for Piles Surgery
piles surgery appointment
What is Piles Surgery?
Hemorrhoids or Piles Surgery / operation is a procedure to remove hemorrhoids (swollen blood vessels in the anus and rectum). They can be caused by several factors, including constipation, straining during bowel movements, pregnancy, and obesity.
There are several types of piles surgery, each with its own advantages and disadvantages. The most common types of piles surgery are Open hemorrhoidectomy, Closed hemorrhoidectomy, Rubber band ligation, Stapled hemorrhoidopexy, Laser hemorrhoidectomy.
The success rate of piles surgery is high. Most people experience relief from their symptoms after surgery. However, there are some risks associated with the procedure, such as infection, bleeding, and pain.
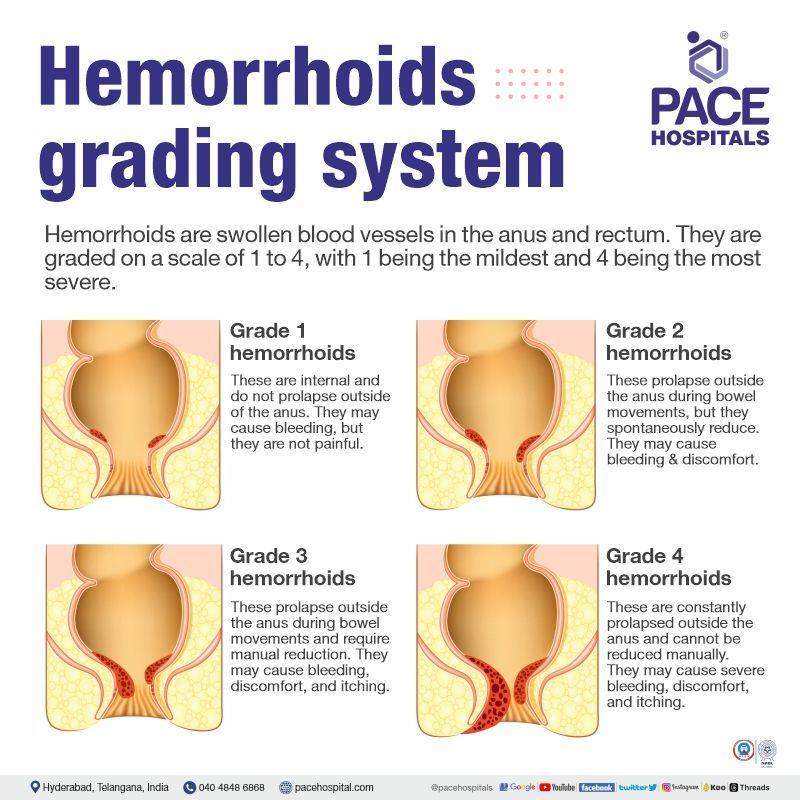
Hemorrhoid Grades
Hemorrhoids are swollen blood vessels in the anus and rectum. They are graded on a scale of 1 to 4, with 1 being the mildest and 4 being the most severe.
- Grade 1 hemorrhoids - These hemorrhoids are internal and do not prolapse outside of the anus. They may cause bleeding, but they are not painful.
- Grade 2 hemorrhoids - These hemorrhoids prolapse outside the anus during bowel movements, but they spontaneously reduce (go back inside the anus). They may cause bleeding and discomfort.
- Grade 3 hemorrhoids - These hemorrhoids prolapse outside the anus during bowel movements and require manual reduction. They may cause bleeding, discomfort, and itching.
- Grade 4 hemorrhoids - These hemorrhoids are constantly prolapsed outside the anus and cannot be reduced manually. They may cause severe bleeding, discomfort, and itching.
The grading of hemorrhoids is important because it helps the gastroenterologist to select the best treatment option. Grade-1 to Grade-2 hemorrhoids can often be treated with conservative measures, such as over-the-counter pain relievers, stool softeners, and sitz baths. Grade-3 to Grade-4 hemorrhoids are severe conditions require surgery.
Piles Surgery Types
In the initial stages of piles/hemorrhoids, the patient is suggested for conservative management. In the patients with grade- 3 and grade- 4 piles/hemorrhoids, gastroenterologist often recommend surgery. The various piles operation procedures are categorised into:
- Non-surgical procedures - Rubber band ligation, Injection scleropathy, Infrared photocoagulation, Electrocoagulation, Lord's procedure
- Surgical procedures -
Haemorrhoidal laser procedure (HeLP), Laser haemorrhoidoplasty (LHP), Hemorrhoidectomy, Stapled haemorrhoidopexy, Haemorrhoidal artery ligation (HALO)
1. Non-surgical procedures for Piles / Hemorrhoids
2. Surgical Procedures for Piles
Preparation for the Piles Surgical Procedure
- The patient should fast for a few hours before piles surgery, as per the surgical gastroenterologist's recommendations.
- The patient will be administered a fleet enema several hours before surgery.
During the Piles Surgical Procedure
- During the hemorrhoidectomy, the surgeon will open the anus and cuts the haemorrhoids gently by using surgical scissors and remove the piles. After removing the piles, the surgeon closes the wounds with stitches or leaves open (open or closed hemorrhoidectomy) based on the patient's condition.
- Based on the patient’s condition, the surgical gastroenterologist would like to prefer various procedures such as stapled hemorrhoidopexy, hemorrhoidal artery ligation, HALO-RAR etc.
- During the hemorrhoidal stapling, the surgeon will perform this process by using a staple device to staple the piles into a normal position within the anal canal. This procedure restricts the blood supply to the piles and causes them to reduce size .
- A proctoscope with a micro-Doppler probe is inserted into the anus during HALO. The haemorrhoidal artery close to the hemorrhoidal tissue is identified. Then the vessel is strangulated using a window (gap) on the proctoscope in the exact location.
- The Doppler probe is taken out of the anal canal during RAR. The prolapsed haemorrhoidal cushion is stitched over its whole length using plication sutures. The prolapsed haemorrhoidal tissue is then drawn up by tightening these running stitches.
After the Piles Surgical Procedure
- Hospitalisation is needed for a few days following the surgery, as the gastro-surgeon advises.
- The surgeon usually suggests some post-operative medications to treat post-operative symptoms.
- The surgeon will suggest the preventive measures after the surgery before discharge.
Piles Surgery Recovery Period or Time
Recovery time after piles surgery varies from person to person based on the severity of the piles and the type of surgical procedure underwent.
- Recovery time for rubber band ligation procedure: Usually, piles will drop off in between 3-10 days, and the patient may resume their normal activities.
- Recovery time for injection sclerotherapy procedure: This procedure usually takes 1-2 weeks to treat the hemorrhoids; the patient may engage in their daily activities after the procedure whenever they feel comfortable (maybe the day after or after a few days).
- Recovery time for infrared coagulation procedure: The patient may return to normal activities within a few days, followed by the procedure.
- Recovery time for the electrocoagulation procedure: Patients might be cleared of the condition after a single treatment and may resume normal activities on the same day.
- Recovery time for the lord’s procedure: Patients are discharged after two days, followed by the procedure, and will be recovered in a few days.
- Piles laser surgery recovery time: LHP is a less painful outpatient surgery with a shorter recovery period. The patient can restart their daily activities within a few hours of the surgery. Recovery time for piles laser surgery is very less when compared to other procedures.
- Recovery from the surgical pile's procedure: This includes invasive procedures such as surgical hemorrhoidectomy, stapled hemorrhoidopexy and hemorrhoidal artery ligation. The piles stapler surgery recovery time, surgical hemorrhoidectomy and stapler surgery recovery time are almost nearer with few days of variation:
- The procedures that restrict the blood supply to the piles require several days afterwards the surgery for hemorrhoids to fall off.
- The wound can heal within 1-2 weeks after the surgery.
- The recovery time for surgical procedures is 1 to 3 weeks from the day of surgery.
Preventive Measures for Piles
After surgery, there are some preventive measures for piles that must be taken into account:
- As the surgeon may advise, hospitalisation is required for a few days.
- To alleviate post-operative problems, the doctor typically recommends several post-operative drugs.
- The doctor will advise accomplishing the following actions before discharging:
- Refraining from straining while going to the toilet
- Staying away from frequent or strenuous lifting
- Staying away from prolonged sitting
- Consuming a diet high in fibre
- Avoiding prolonged hours of sitting
- Consuming lots of water
- Taking a sitz bath
Advantages of Piles Operation
There are a lot of advantages regarding the pile’s surgical procedures. The advantages of piles surgery vary from procedure to procedure due to differences in their principles. Advantages for various piles treatment procedures are as follows:
- Rubber band ligation: Rubber band ligation is very effective and safe procedure with less severe complications and quick recovery.
- Injection sclerotherapy: It doesn’t require hospitalisation. It is the best and safe technique when compared to other conventional procedures in terms of cost, recovery and side effects.
- Infrared photocoagulation: Due to its less invasive nature, absence of serious consequences, and secondary bleeding, infrared photocoagulation is stated as a safer procedure than standard surgery with a quick recovery. There are no recurring costs other than the initial cost of the instrument.
- Lord’s procedure: This is the manual procedure with less cost and low complications.
- Laser surgery or laser haemorrhoidoplasty: This is the best treatment for patients who are unresponsive to surgical procedures. The patient may engage in daily activities within a few days after the procedure. The patient might be suggested for discharge on the surgery day itself. There will be no postoperative complications such as severe bleeding and pain.
- Invasive procedures: The invasive procedures such as surgical hemorrhoidectomy, stapled hemorrhoidopexy and hemorrhoidal artery ligation are the standard treatment procedures for piles due to the less recurrence. This procedure helps to remove hemorrhoidal tissue completely. These procedures are indicated to treat the piles with severe grades as well as prolapsed.
Disadvantages of Piles Operation
The disadvantages of piles surgical procedures are as follows:
- Rubber band ligation: Few minor complications such as pain, bleeding, and urinary retention are seen.
- Injection sclerotherapy: Minor complications such as bleeding and clotting are seen. It is not recommended for the patients with inflammatory bowel disease, thrombosed hemorrhoids, and allergic patients.
- Infrared photocoagulation: Except for minor complications such as mild bleeding, pain, itchy anus, etc., there are no major complications. Recurrence of piles may occur in some cases.
- Lord’s procedure: Incontinence and pain are often seen after this procedure. It might not be apt in all cases.
- Laser surgery or laser haemorrhoidoplasty: Laser surgery is expensive when compared to other traditional and conventional methods. It requires trained surgeons to operate the laser beam. There might be a chance of a recurrence of piles in the future.
- Invasive procedures: Invasive procedures such as surgical hemorrhoidectomy, stapled hemorrhoidopexy, and hemorrhoidal artery ligation require a hospital stay of a few days when compared to non-invasive outpatient procedures. Major complications, such as severe pain, bleeding, infections, etc., are seen at the surgical site. The recovery time is longer (nearly 3 weeks) when compared to non-invasive procedures.
Piles Operation Cost in Hyderabad, India
Piles Surgery Cost in Hyderabad generally ranges from ₹24,000 to ₹78,000 (approx. US $290 – US $940).
The exact piles surgery cost varies depending on factors such as the grade of hemorrhoids, type of procedure performed (open, closed, stapler, laser), number of hemorrhoids involved, need for anesthesia, surgeon expertise, hospital stay duration, and hospital facilities — including cashless treatment options, TPA corporate tie-ups, and assistance with medical insurance wherever applicable.
Cost Breakdown According to Type of Piles Surgery
- Open Hemorrhoidectomy – ₹24,000 – ₹40,000 (US $290 – US $480)
- Closed Hemorrhoidectomy – ₹28,000 – ₹45,000 (US $340 – US $540)
- Stapler Hemorrhoidectomy (PPH Procedure) – ₹45,000 – ₹70,000 (US $540 – US $845)
- Laser Hemorrhoidoplasty / Laser Piles Surgery – ₹35,000 – ₹78,000 (US $420 – US $940)
- Piles Surgery with Fissure / Fistula Repair (If Required) – ₹38,000 – ₹78,000 (US $455 – US $940)
Frequently Asked Questions (FAQs) on Piles Surgery
How much does piles surgery cost in India?
Piles surgery cost in India ranges varies from ₹ 45,000 to ₹ 90,000 (INR forty-five thousand to ninety thousand). However, cost of hemorrhoids or piles surgery in India may vary depending upon the different hospitals in different cities.