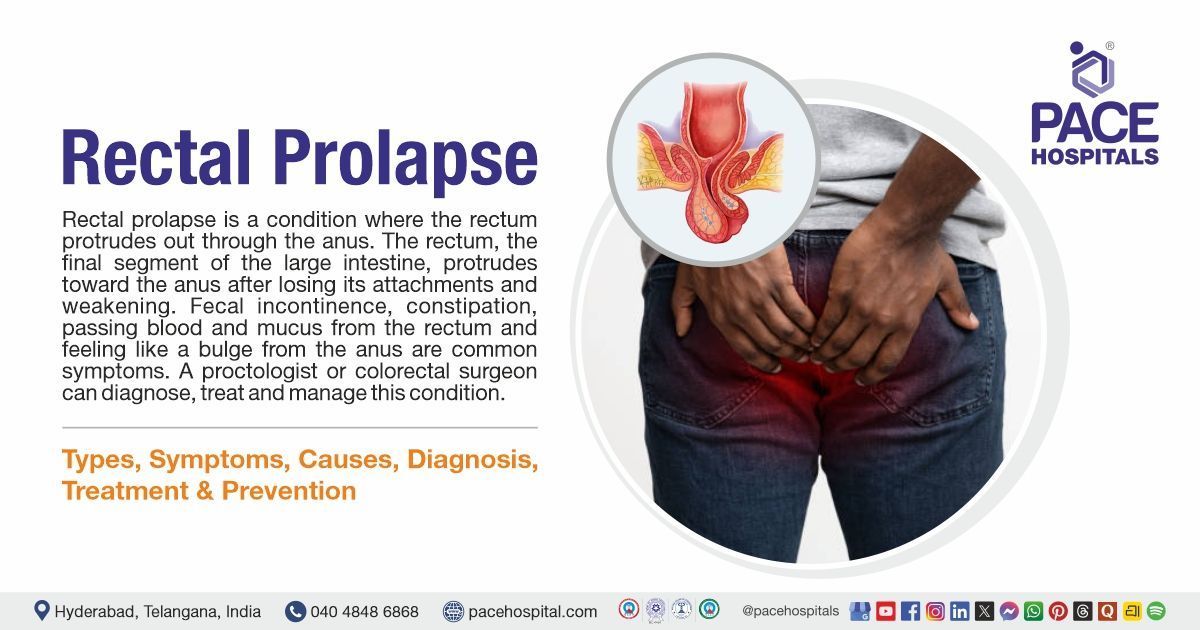
Rectal Prolapse: Symptoms, Causes, Diagnosis, Treatment & Prevention
PACE Hospitals
Written by: Editorial Team
Medically reviewed by: Dr. Padma Priya - Consultant Gastroenterologist and Hepatologist
Overview | Prevalence | Types | Symptoms | Causes | Risk Factors | Complications | Diagnosis | Treatment | Prevention | Rectal prolapse vs Haemorrhoids | FAQs | When to consult a Doctor
Rectal prolapse definition
Rectal prolapse is a condition where the rectum protrudes out through the anus. The rectum, the final part of the large intestine, loses its attachments and becomes weakened, protruding towards the anus. It is more likely to occur in females than in males, especially in older adults. Common symptoms of rectal prolapse include faecal incontinence, constipation, passing blood and mucus from the rectum, and feeling like a bulge from the anus.
The etiology of rectal prolapse is multifactorial; it includes weakened pelvic floor muscles, anal sphincters, long-term constipation or diarrhoea, damage from giving birth, and cystic fibrosis. Complications of rectal prolapse include ulceration or bleeding, incarceration (rectum prolapsed which cannot be pushed back) and strangulation (cut off of blood supply to the prolapsed rectum).
A proctologist or colorectal surgeon specialised in the lower gastrointestinal tract, such as the colon, rectum, and anus, can accurately diagnose and provide appropriate treatment for rectal prolapse.
Rectal prolapse meaning
The word rectal prolapse originates from two Latin words.
- “Rectal”- from the Latin word rectum, meaning straight, pertaining to or connected with the rectum, which is the last part of the large intestine.
- “Prolapse”- from Latin prolapsus, which means slip forward or down.
Thus, the meaning of rectal prolapse is the slipping forward or downward of the rectum through the anus.
Rectal Prolapse Prevalence
Rectal prolapse prevalence worldwide
Rectal prolapse is more common in Western countries, with a prevalence of 2.5 per 100,000 population. Women are more affected than men, especially the elderly, with a 9:1 ratio. This disease is more common in individuals over 50.
Rectal prolapse prevalence in India
Rectal prolapse is a rare condition, and there is limited large-scale data in India; most data come from small hospitals or clinics.
Rectal Prolapse Types
Rectal prolapse types are based on whether one part or all of the rectum protrudes out of the anus. These are classified into three types:
- Complete (or full-thickness) rectal prolapse
- Mucosal (or partial-thickness) rectal prolapse
- Internal rectal prolapse (Intussusception)
Complete (or full-thickness) rectal prolapse
When all layers of the rectal wall protrude out of the anus, it is called complete or full-thickness rectal prolapse. This causes symptoms like blood or mucus in the stools, difficulty defecating, and anal incontinence.
Mucosal (or partial-thickness) rectal prolapse
When the mucosal or inner layer of the rectum protrudes through the anus, it is called partial or mucosal rectal prolapse.
Internal rectal prolapse (Intussusception)
It is also called rectal intussusception, in which the rectum folds in on itself but doesn't protrude out of the anus.
Rectal Prolapse Symptoms
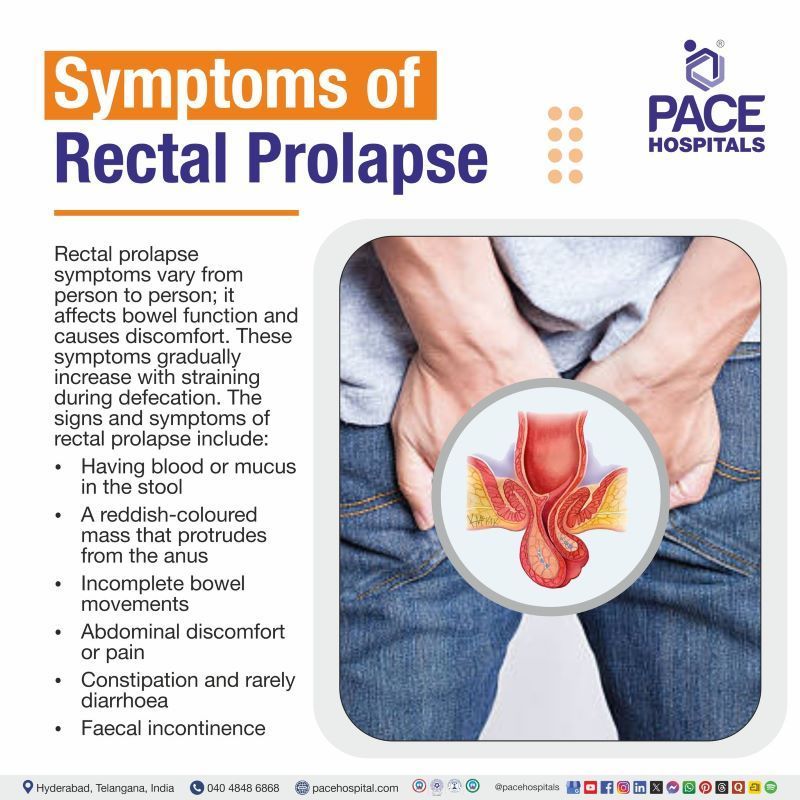
Rectal prolapse symptoms vary from person to person; it affects bowel function and causes discomfort. These symptoms gradually increase with straining during defecation. The signs and symptoms of rectal prolapse include:
- Having blood or mucus in the stool
- A reddish-coloured mass that protrudes from the anus
- Incomplete bowel movements
- Abdominal discomfort or pain
- Constipation and rarely diarrhoea
- Faecal incontinence
Having blood or mucus in the stool: In rectal prolapse, the rectal lining is irritated, leading to inflammation and blood or mucus in the stool. Repeated straining or friction causes the prolapsed tissue to bleed. The rectal mucosa produced excess mucus as a protective response. In prolonged or repeated prolapse, the symptoms may worsen.
A reddish-coloured mass that protrudes from the anus: It is the main symptom of the rectal prolapse, where the reddish coloured mass that sticks out of the anus is the inner lining of the rectum. It causes discomfort, pain and bleeding.
Incomplete bowel movements: Incomplete bowel movements occur when stool remains in the rectum after a bowel movement; they are a common symptom of rectal prolapse. To pass stool, force or strain is needed.
Abdominal discomfort or pain: Rather than direct straining of the rectal muscles, abdominal discomfort is typically caused by severe prolapse that results in a feeling of fullness, incomplete bowel evacuation, or related pelvic floor dysfunction. More often than not, straining is a factor in the onset or severity of prolapse. Instead of the abdomen, pain is usually restricted to the perineal or anal area.
Constipation and rarely diarrhoea: Constipation results from the prolapsed rectum obstructing the passage of stool, and diarrhoea may be brought on by related pelvic floor dysfunction or straining; alternating patterns frequently occur as the condition worsens.
Faecal incontinence: Faecal incontinence often correlates with underlying anal sphincter weakness rather than a single cause in patients with obvious rectal prolapse. The sphincter may become less effective due to ageing, persistent pelvic floor dysfunction, and prior anorectal surgery. Impaired continence is frequently caused by structural flaws and decreased anal tone.
Rectal Prolapse Causes
The etiology of rectal prolapse is multifactorial. Some structural defects and risk factors increase the chance of rectal prolapse. Paediatric patients are more prone to develop rectal prolapse when compared to adults. It includes:
Structural defects
Defects in the pelvis or lower GI tract are found in adults with rectal prolapse, which may increase the rectal prolapse. Weakened anal sphincter and pelvic muscles, and a rectum that is not positioned correctly and tends to prolapse more than usual, are among the structural defects that increase the risk of rectal prolapse in adults.
In paediatrics, rather than the usual curve of the rectum, it is in a straight, vertical position, which may increase the chance of rectal prolapse.
Rectal Prolapse Risk Factors
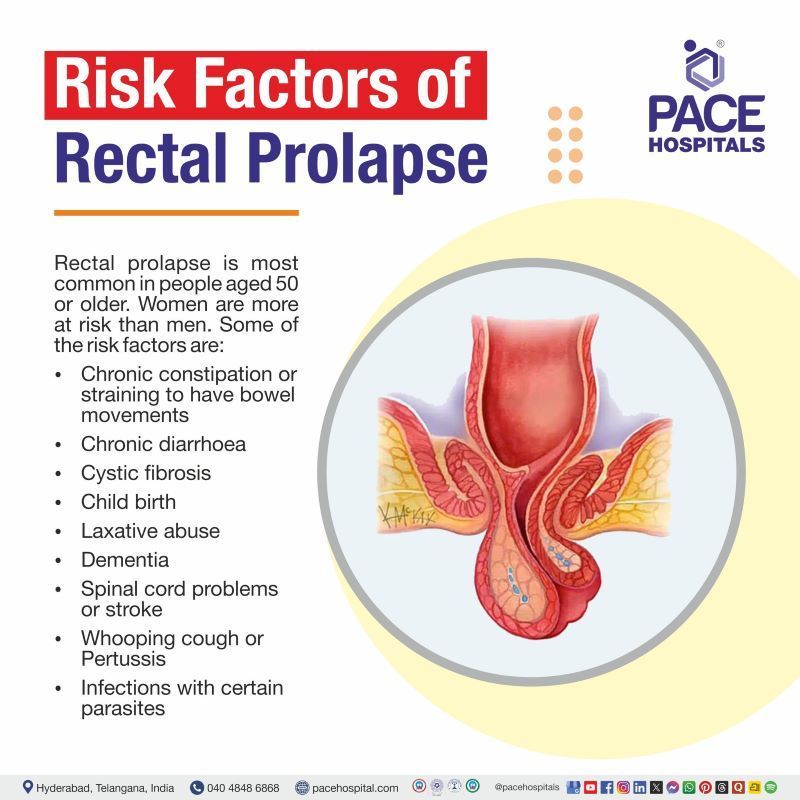
Rectal prolapse is most common in people aged 50 or older. Women are more at risk than men. Some of the risk factors are:
- Chronic constipation or straining to have bowel movements
- Chronic diarrhoea
- Cystic fibrosis
- Child birth
- Laxative abuse
- Dementia
- Spinal cord problems or stroke
- Whooping cough or Pertussis
- Infections with certain parasites
Chronic constipation or straining to have bowel movements: It is the most important factor of the rectal prolapse. During defecation, due to constipation, the rectal muscles strain. Repeated straining causes pressure in the abdomen and the rectum. This pressure stretches the attachments of the rectum and the pelvic floor, leading to rectal prolapse.
Chronic diarrhoea: In chronic diarrhoea, frequent bowel movements increase pressure on the rectum. Repeated pressure on the rectal muscles during bowel movements can cause prolapse.
Cystic fibrosis: Cystic fibrosis increases the risk of rectal prolapse, causing malabsorption from pancreatic insufficiency, which results in large, fatty stools and persistent straining when defecating. Young children are most frequently affected by this strain, which weakens the pelvic floor and the supporting ligaments of the rectum. It may even occur before a formal diagnosis, acting as an early warning sign.
Child birth: Women are more affected than men, especially in women with multiple deliveries. Pregnancy and childbirth can stretch or injure pelvic floor muscles and nerves. Difficult, prolonged, or instrument-assisted deliveries further increase the risk by damaging pelvic support structures.
Laxative abuse: Abuse of laxatives causes chronic diarrhoea, which over time irritates and weakens the pelvic floor muscles and rectal mucosa, leading to rectal prolapse. Protrusion is more likely due to this loss of rectal support.
Dementia: Rectal prolapse is most prevalent in elderly dementia patients. Inadequate bowel movements and diminished defecation awareness increase stress, which is exacerbated by persistent constipation brought on by immobility, dehydration, poor diet, and medication. Rectal strength is further decreased by general muscle weakness and loss of pelvic floor tone.
Spinal cord problems or stroke: Spinal cord problems or stroke are one of the risk factors of rectal prolapse, resulting from neurogenic bowel dysfunction, which leads to chronic constipation and excessive straining. Rectal pressure increases and pelvic support weakness, both of which increase the risk of prolapse.
Whooping cough or Pertussis: Whooping cough (Pertussis) can cause rectal prolapse, mainly in children, due to repeated increases in abdominal pressure. Constant straining of the rectum and weakened pelvic support lead to prolapse. This prolapse resolves once the cough is treated.
Infections with certain parasites: Some of the parasitic infections in the intestine cause chronic diarrhoea, straining and May also lead to rectal prolapse. It can be diagnosed by identifying the parasite's eggs or larvae in stool or the rectum.
Rectal Prolapse Complications
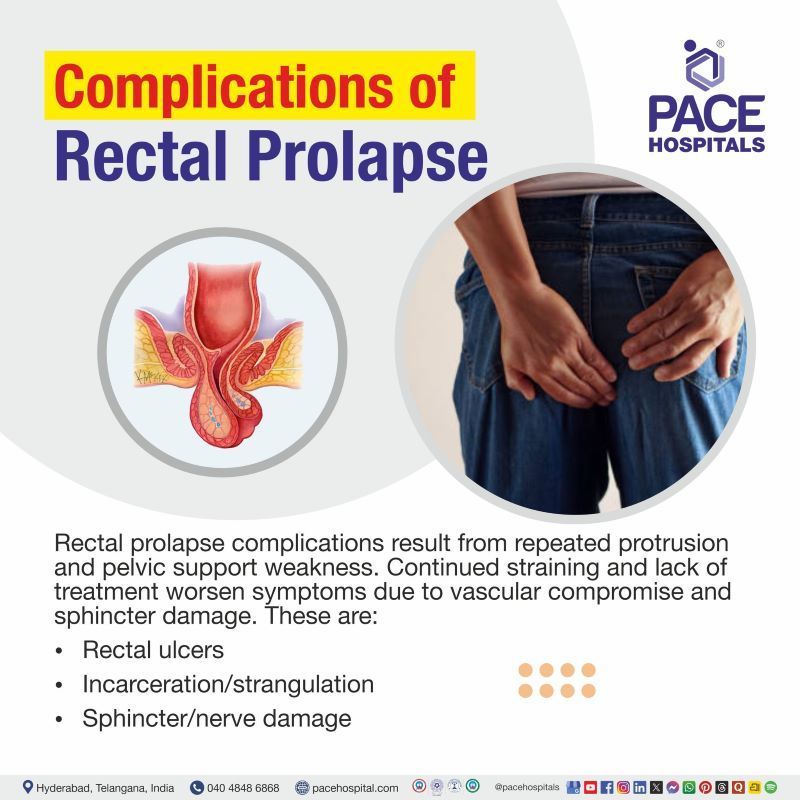
Recurrent tissue damage from protrusion and the progressive weakening of pelvic structures are the main causes of complications from rectal prolapse. Persistent straining from constipation or diarrhoea causes prolapse, but untreated cases get worse due to vascular compromise, sphincter stretching, and persistent inflammation. Complications are:
- Rectal ulcers
- Incarceration/strangulation
- Sphincter/nerve damage
Rectal ulcers: Rectal ulcers are painful sores in the rectum that can bleed uncontrollably and cause anaemia. Solitary rectal ulcer syndrome is seen in rectal prolapse. Chronic trauma and a reduced blood supply to the prolapsed rectal mucosa are the causes of rectal ulcers.
Incarceration/strangulation: Incarceration means the rectal prolapse is trapped and cannot be pushed back into the rectum, but it still has a blood supply. In contrast, strangulation means the blood supply is cut off to the trapped tissue, which is a medical emergency. Incarceration leads to strangulation if untreated.
Sphincter/nerve damage: Sphincter muscle or nerve damage in the rectum occurs due to persistent stretching, leading to improper bowel movements and rectal prolapse, which can cause faecal incontinence.
Rectal Prolapse Diagnosis
To diagnose rectal prolapse, the proctologist or colorectal surgeon performs a physical examination, reviews medical history, and then advises lab tests.
The following are the steps included in the diagnostic criteria for rectal prolapse:
- Medical history
- Physical examination
- Laboratory test
- Blood tests
- Imaging tests
- Defecogram/ Defecography
- Barium enema
- Endoscopic evaluation
- Colonoscopy
- Other diagnostic tests
- Anorectal manometry
- Special urologic or gynaecologic evaluations
Rectal Prolapse Treatment
The main goals of treatment in rectal prolapse include lowering the prolapse, easing symptoms like pain and bleeding, and making it easier to control bowel movements. Lifestyle and dietary changes also help treat prolapse. Rectal prolapse treatment includes:
- Non-pharmacological therapy
- Pharmacological therapy
- Surgical interventions
Non-pharmacological therapy
- Most rectal prolapses can be reduced manually with gentle digital pressure, pushing the prolapsed rectum back into the anal canal.
- In incarcerated prolapse, oedema is reduced by applying salt or sugar.
- Factors that cause prolapse, like constipation and diarrhoea, are managed.
- Biofeedback therapy is a non-invasive, behavioural therapy which trains the patient about the rectal pressure and sphincter relaxation during defecation to improve the anal and sphincter functions.
- Changing diet by increasing the fibre intake and maintaining hydration
Pharmacological therapy
There is no specific treatment for rectal prolapse; symptoms can be managed. They are:
- Stool softeners
- Laxatives
- Anti-diarrhoeal drugs
- Suppositories or enema
Surgical interventions
Surgical treatment of rectal prolapse is based on the patient’s age and other comorbidities. These are classified into two types:
- Abdominal procedures
- Perineal procedures
Abdominal procedures
- Laparoscopic surgical rectopexy
- Anterior resection
- Marlex rectopexy
- Suture rectopexy
- Resection rectopexy
Perineal procedures
- Anal encirclement
- Delorme mucosal sleeve resection
- Altemeier perineal rectosigmoidectomy
- Perineal stapled prolapse resection
- Haemorrhoidectomy
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
Rectal Prolapse Prevention
Preventing rectal prolapse primarily involves addressing factors that increase rectal pressure and weaken pelvic muscles. Those are:
- Avoiding constipation
- Avoiding straining
- Kegel exercises
- Maintain a healthy body mass index
- Avoiding strenuous activities
- Postpartum care
Avoiding constipation: Eating plenty of fibre and maintaining hydration will help keep the bowels regular. Fruits, vegetables, and whole-grain cereals are all high in fibre. Regular gentle exercise will also help prevent constipation.
Avoiding straining: Applying excessive pressure on the pelvic floor area when trying to empty the bowels will make it harder and cause the pelvic floor muscles to weaken, which can lead to a rectal prolapse.
Kegel exercises: Regularly performing Kegel exercises, which strengthen the pelvic floor muscles, can help. As the muscles become stronger, the pelvic organs become stronger and prevent prolapse.
Maintain a healthy body mass index: Obesity is a significant problem that causes abdominal pressure and weakened pelvic muscles. Maintaining a healthy body mass index (BMI) is essential to prevent rectal prolapse.
Avoiding strenuous activities: Excessive heavy lifting or strenuous work weakens the pelvic floor muscles. Proper exercise techniques are used to minimise pelvic floor weakness.
Postpartum care: Proper postpartum care needs to be taken in women who have had multiple vaginal deliveries, which increases the risk of rectal prolapse.
Difference between Rectal Prolapse and Hemorrhoid
Rectal prolapse refers to when the wall of the rectum sticks out all the way around the anal opening. Haemorrhoids, on the other hand, are swollen blood vessels in the anal canal. They differ in origin, anatomical involvement, and clinical presentation. Some of the differences are:
Rectal prolapse vs Haemorrhoids
| Parameters | Rectal prolapse | Hemorrhoids |
|---|---|---|
| Definition | Rectal prolapse is a condition where the rectum protrudes through the anus. The rectum, the final part of the large intestine, loses its attachments and becomes weakened, protruding towards the anus. | Inflammation of the veins in and around the anus is called haemorrhoids. These are of two types, external and internal haemorrhoids. |
| Etiology | Chronic constipation, diarrhoea, cystic fibrosis, dementia, pregnancy, etc | Abnormal bowel movements, constipation, diarrhoea, pregnancy. |
| Pathophysiology | Weakened pelvic floor support can cause internal rectal intussusception or a sliding hernia of the rectum. | Develops due to the deterioration of the muscular and elastic support of the anal vascular cushions (corpus cavernosum recti), resulting in their distal displacement. It can cause swelling, congestion, bleeding, and even prolapse. |
| Symptoms | A reddish-coloured mass that protrudes out of the anus, faecal incontinence, having blood or mucus in the stool, constipation, or diarrhoea. | Itching, swelling, pain and irritation around the anus, blood in the stools. |
| Diagnosis | Defecography, colonoscopy, Anorectal manometry, MRI. | Anoscopy, proctoscopy, sigmoidoscopy |
| Treatment | Symptomatic treatment includes laxatives, stool softeners, suppositories and surgery. | Sclerotherapy, Rubber band ligation, Hemorrhoidectomy |
Frequently Asked Questions (FAQs) on Rectal Prolapse
What is rectal prolapse?
Rectal prolapse is a condition where the rectum falls through the anus. The rectum, the final part of the large intestine, loses its attachments and becomes weakened, protruding towards the anus. It is more likely to occur in females than in men. Common symptoms of rectal prolapse include constipation, diarrhoea, passing blood and mucus from the rectum, and feeling like a bulge from the anus.
What causes rectal prolapse?
The aetiology of rectal prolapse is multifactorial. Some structural defects and risk factors increase the chance of rectal prolapse. Structural defects in the pelvic and lower GI tract, chronic diarrhoea, constipation, cystic fibrosis, and straining of bowel movements cause rectal prolapse.
Is rectal prolapse dangerous?
Rectal prolapse is not usually life-threatening, but if it is not treated, it can cause problems like rectal ulcers, incarceration or strangulation, which means preventing the blood supply to the rectum. It mainly affects older women more than men, and it can cause symptoms like bleeding, faecal incontinence, and a bulging rectal mass. Getting medical help right away is very important to stop things from getting worse.
Can pregnancy and childbirth increase the risk of rectal prolapse?
Rectal prolapse is quite rare in women of childbearing age and infrequently occurs during pregnancy. Giving birth itself doesn't usually raise the risk, but women who have had perineal tears or multiple vaginal deliveries before may be more vulnerable. Suppose a patient had rectal prolapse while pregnant, extra care has to be taken. Using forceps to help with delivery while the mother is under epidural anaesthesia can help ease the strain and stop the prolapse from getting worse.
How to prevent rectal prolapse?
Rectal prolapse can be prevented by making lifestyle changes that address constipation and pelvic floor weakness. Avoid straining the pelvic muscles; maintain a high-fibre diet to prevent constipation; maintain a healthy weight; perform Kegel exercises; and avoid strenuous activities.
Can rectal prolapse be treated without surgery?
In adult patients, the primary treatment of rectal prolapse is surgical, as there is no specific medical treatment available; early signs can be managed with lifestyle changes. Whereas in kids, it's treated without surgery by addressing the underlying problem.
Can rectal prolapse go away on its own?
In adults, rectal prolapse rarely resolves on its own; in most cases, surgery is required. Whereas in children, they can benefit from a bowel management program. It can be done by fixing constipation, diarrhoea and bowel habits. It shows that surgical intervention is rarely required in children.
What are the symptoms of rectal prolapse?
Rectal prolapse manifests with various symptoms, some of the common symptoms are a reddish lump sticking out from the anus, faecal incontinence, and mucus or blood discharge, incomplete bowel movements, abdominal discomfort or pain; these may worsen if untreated.
Which doctor to consult for rectal prolapse?
A proctologist or colorectal surgeon, a doctor specialised in the lower gastrointestinal tract, such as the colon, rectum, and anus, can accurately diagnose and provide appropriate treatment for rectal prolapse.
What are the types of rectal prolapse?
Rectal prolapse types are based on whether one part or all of the rectum falls out of the anus. These are classified into three types, they are: Complete (or full thickness) rectal prolapse where all the layers of the rectal wall falls out of the anus, Mucosal (or partial-thickness) rectal prolapse is where the mucosal or inner layer of the rectum protrudes out through the anus and internal rectal prolapse also called rectal intussusception, in which the rectum folds itself but doesn't falls out of the anus.
What is internal rectal prolapse?
Internal rectal prolapse is where one part or all of the rectal wall folds in on itself without protruding out of the anus. It occurs due to straining during defecation because the abdominal pressure is higher. The prolapse is not visible externally, but it can cause symptoms such as constipation or the feeling that the bowel is not emptying. Imaging tests such as defecography or MRI are usually used to diagnose this disease.
What is incarceration and strangulation?
Incarceration means the rectal prolapse is trapped and cannot be pushed back into the rectum, but it still has a blood supply. In contrast, strangulation means the blood supply is cut off to the trapped tissue, which is a medical emergency. Incarceration leads to strangulation if untreated.
What is the difference between rectal prolapse and haemorrhoids?
Rectal prolapse and prolapsed internal haemorrhoids may have similar causes and symptoms. Rectal prolapse is complete intussusception of the entire rectal wall, characterised by circular (concentric) mucosal folds. On the other hand, internal haemorrhoids are swollen submucosal blood vessels in the anal canal that have radial folds. It is very important to correctly identify these two conditions because the treatments are very different.
Who is more likely to develop rectal prolapse?
Rectal prolapse is more common in adults over 50, especially women. This is because the pelvic floor weakens with age, childbirth, chronic straining, and constipation.
When to consult a doctor for rectal prolapse?
Consult a doctor for rectal prolapse if tissue keeps coming out from the anus, if there is discomfort during defecation, or if there is a feeling of incomplete bowel emptying. Signs that indicate a need for medical assistance are:
- Having blood or mucus in the stool
- A reddish-coloured mass that comes out of the anus
- Incomplete bowel movements
- Abdominal discomfort or pain
- Constipation, diarrhoea, or both
- Fecal incontinence
If these symptoms persist, it is best to see a rectal prolapse specialist for an accurate diagnosis and treatment. Seek emergency medical attention if the prolapsed tissue cannot be pushed back in, or if you experience pain, blood or mucus in the stool. A proctologist can provide the best rectal prolapse treatment to manage symptoms and reduce long-term risks.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868