Third Space Endoscopy - Indications and Techniques
Dept. of Gastroenterology at PACE Hospitals, is equipped with advanced Endoscopic Resection and Third-Space Endoscopy System, The SpyGlass® Direct Visualization System and Laparoscopic surgery equipment to perform complex and supra-major precancerous and cancerous conditions of gastrointestinal (GI) tract.
Our team of the Top Gastroenterologist in Hyderabad, India; are having extensive experience in performing endoscopic Resection and third space endoscopy (TSE) techniques such as endoscopic mucosal resection (EMR), endoscopic submucosal dissection (ESD), peroral endoscopic myotomy (POEM), and submucosal tunneling endoscopic resection (STER) to treat conditions of gastrointestinal system.
Request Appointment Third Space Endoscopy
Third Space Endoscopy - appointment
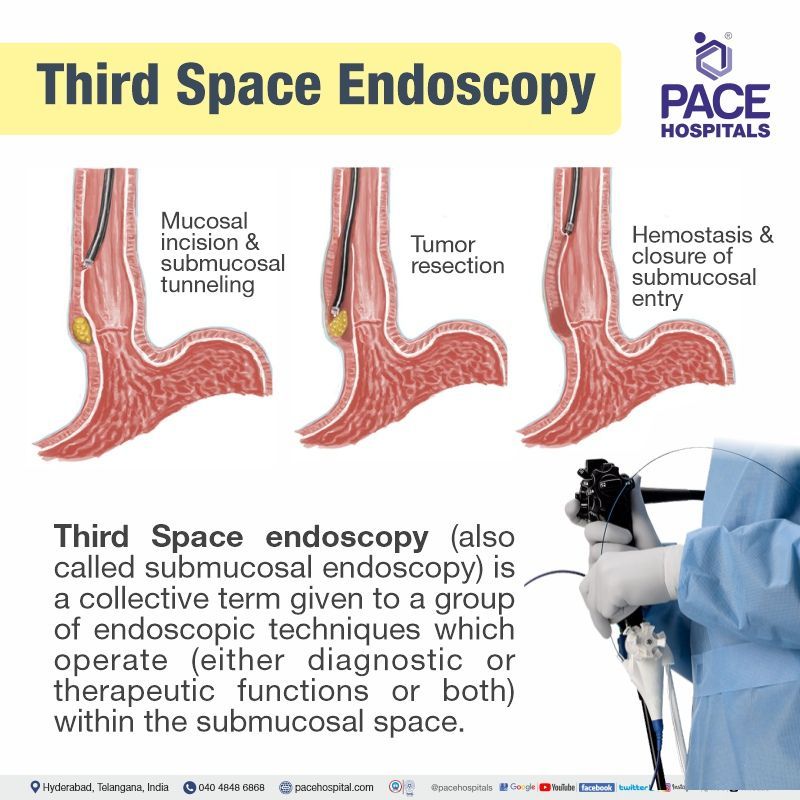
What is Third-Space Endoscopy?
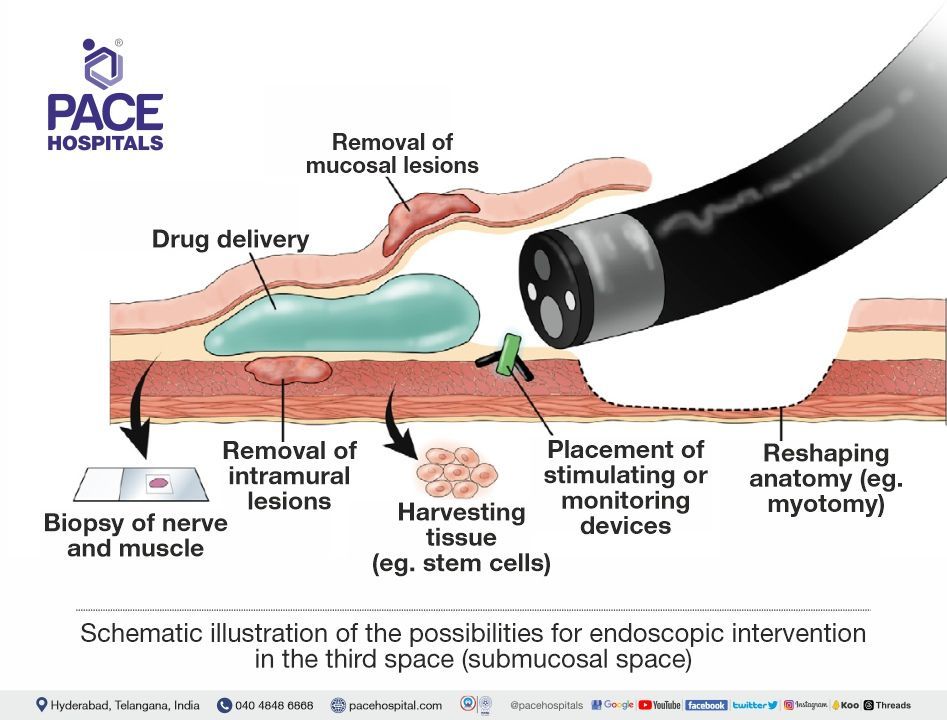
Third-space endoscopy (also called submucosal endoscopy) is a collective term given to a group of endoscopic techniques which operate (either diagnostic or therapeutic functions or both) within the submucosal domain (the wall of the gut called the submucosal space). In a few cases, third-space endoscopy also delves into muscular and subserosal layers. These layers form the wall of the gastrointestinal (GI) lumen.
What is Endoscopy?
An endoscopy is a procedure to look into the alimentary canal (gut). It is done with the help of an endoscope, which consists of a thin, long tube fitted with a tiny camera with a light source. Through an endoscope, the healthcare personnel is able to look inside the alimentary canal by inserting it into the body through a natural opening such as either mouth or anus.
Endoscopy may be prescribed if the patients display certain symptoms. There are various types of endoscopies done depending on symptoms presented, through which gastroenterologists seek a way to understand ailments of the body through:
- Peering inside the human body,
- Unlocking the secrets to understanding the form and function of organs,
- Learning how disease originates and progresses,
- How injuries affect the body's system and structure, and, most importantly, to offer surgical methods that promote rapid healing.
With the ability to access, visualise, and manipulate a patient's internals came the advent of new techniques and cures for disease and injury, but more importantly, the concept of minimal invasion to treat these internal complications.
Illumination and visualisation – How did fibre optics pave the way for endoscopy?
A British physicist named Harold Hopkins could be considered the most prominent inventor and pioneer of endoscopic visualisation. In 1967, he devised an optic system that used "large quartz, rod-shaped lenses", which not only significantly enhanced the image projected to the eye but also is a device still used in modern-day scopes.
By the 1970s, Hopkins' quartz rod-lens had evolved into a "flexible fibre optic" made from thousands of glass fibres, which were developed by heating a segment of glass rod until it is molten and then stretching it rapidly, creating a thread-like fibre with altered physical properties. These threads ended up being far smaller than human hair, ending up with a diameter between 5-25µm and having the ability to flex without breaking.
These long glass fibres also preserved their capability of conducting light through "internal refraction", and in an ideal world, none of this light was lost beyond that which was internally absorbed by the glass itself, a system known as "optical insulation". Easy manufacturing combined with the fibres' small size and flexible properties while still being able to sufficiently transmit light made fibre-optics the first choice over traditional short glass lenses and later Hopkins' initial rod-lens design.
Light cannot be transmitted by individual fibres since they are too weak on their own. Therefore, thousands of small fibres are combined to intensify the light being transmitted. This bundle of fibres combines the two most basic necessities of visualisation:
- Illumination of the interior body
- Transmission of the lighted image to the user's eye or camera.
To clarify, there is one bundled unit of fibres that has been separately insulated into those two units for lighting and reflecting the image. The illumination bundle is just that, a non-specific arrangement of fibres called an “incoherent” blend.
However, the fibres in the image bundle are organised in such a way that the pattern found at the distal tip is the same at the proximal end. Each fibre transmits one piece of information, like one pixel on a computer screen. Those ‘pixel’ images line up in the exact manner they accepted the image inside the patient so that the image the viewer sees is the same coherent image. This arrangement of the image bundle is called “coherent”.
Modern endoscopes that use Hopkins' fibre-optic technology can be made of flexible tubing rather than the rigid scopes of past designs. Fibre optics replaced the "standard relay assembly". The resolution of the image reflected back to the user is higher than were classical endoscopes.
It should not be forgotten that this resolution still depends on the physical structure of the fibres. When the fibres are regularly spaced, with an even density, they transmit the highest quality image.
More fibres translate to more ‘pixels’ in the analogy above, but when the fibres are much smaller than 5µm, their physical strength and structural integrity are lost, and fracturing becomes a concern. It is for this reason the range of 5-25µm has become standard. Another advantage of many small fibres is their ability to allow the reflected image to be transmitted with high precision and clarity, even when the bundle is curved.
Modern endoscopy developed basically overnight toward the technology currently being used. It is easy to understand this immediate jump toward modernity due to “clear and colour-true images, with a breathtaking 3-D like field of vision with a depth of field never before imagined".
Why is it called third-space endoscopy?
While general endoscopy (usually for diagnosis) is called first-space endoscopy, with increasing technology, second-space endoscopy, which deals with the peritoneal cavity, has evolved. The development of flexible endoscopy widened the range of endoscopy. The final frontier – the third space endoscopy deals with endoscopic activities related to intramural or submucosal space.
| Elements | First space endoscopy | Second space endoscopy | Third space endoscopy |
|---|---|---|---|
| What it is? | Inserted into the alimentary canal either through the mouth or anus | The endoscope, which is inserted into the gut, reaches peritoneal space by breaching the gut wall to perform the medical procedure. | The endoscope is inserted into the gut, and it performs medical procedures at the wall of the gut (intramural or the submucosal space). |
| History | In 1955, the first endoscopic procedure (polypectomy) was performed by Rosenbergto perform patients with rectal and sigmoid polyps, using a rigid scope. | In 2004, flexible transgastric peritoneoscopy was done in pigs. | In 2010, the first human results of peroral endoscopic myotomy (POEM) were done. It opened the significance of submucosal space as an operating field. |
| Examples | Colonoscopy, Colposcopy, Cystoscopy, Gastroscopy, Hysteroscopy etc | Natural orifice transluminal endoscopic surgery (NOTES), Endoscopic transgastric appendectomy, etc | G-POEM, POET, POETRE, POP, STER, STESD, Z-POEM etc |
Third-space endoscopy indications
With its initial utilisation for the treatment of achalasia, the field of third-space endoscopy has been ever-expanding, gradually replacing conventional surgeries. The indication of third-space endoscopies greatly depends on the type of procedure. A few of the indications include:
- Subepithelial tumours (asymptomatic lesions with normal overlying mucosa)
- Refractory gastroparesis (delayed gastric emptying despite medication)
- Zenker diverticulum. (tightened throat muscle causing pharyngeal pouch)
- Restoration of completely obstructed oesophageal lumen after chemoradiation
- Hirschsprung disease (a large intestine condition affecting stool passage)
- Internal anal sphincter achalasia (lack of relaxation of the internal anal sphincter)
- Oesophagogastric junction outflow obstruction with preserved peristalsis
- Distal oesophageal spasm (oesophageal muscle constrictions)
- Jackhammer oesophagus (abnormal muscular actions of the oesophagus)
- Barrett's Oesophagus (damaged lower oesophagus due to acid reflux)
Types of endoscopic procedures which fall in third space endoscopy
Inoue and team performed the first-ever case of peroral endoscopic myotomy (POEM) for achalasia in 2010, which opened the doors of innovation and advancement for the development of third-space endoscopy.
Since then, various types of third-space endoscopic procedures have been developed to satiate various diseases. A few of the common third-space endoscopic procedures include :
- Esophageal peroral endoscopic myotomy (E-POEM)
- Gastric peroral endoscopic myotomy (G-POEM)
- Peroral endoscopic myotomy for Zenker diverticulum (Z-POEM)
- POET, peroral endoscopic tunnelling (POET)
- Peroral endoscopic myotomy (POEM)
- Per-oral pyloromyotomy (POP)
- Endoscopic submucosal dissection (ESD)
- Submucosal tunnelling endoscopic dissection (STER)
- Submucosal tunnelling endoscopic septum division (STESD)
- Peroral endoscopic tunnelling for restoration of the esophagus (POETRE)
Third-Space Endoscopy Advantages
Third-space endoscopy offers several advantages in the field of therapeutic endoscopy. Given that third-space endoscopy is a collective term, the advantages could be listed only from isolated procedural settings. Recent studies have considered comparing individual submucosal endoscopic procedures with conventional surgeries to understand the advantages offered by third-space endoscopy.
Listed below are a few of the various key advantages obtained from a few recent studies:
- Precise dissection
- Minimally invasive
- Avoidance of full-thickness incision
- Enhanced visualisation
- Potential for robotic assistance
- Precise dissection: An article published in Gastrointestinal Endoscopy Clinics of North America in 2023 provided an overall advantage of accuracy and precision present in third-space endoscopy operating in the submucosal plane. Such precision can only be obtained from third-space endoscopic procedures such as endoscopic submucosal dissection (ESD) and peroral endoscopic myotomy (POEM)
- Avoidance of full-thickness incision: Third-space endoscopy allows procedures (especially submucosal tunnelling) to be performed without the necessity of a full-thickness incision in the gastrointestinal tract. Submucosal tunnelling is also useful for procedures such as peroral endoscopic myotomy and submucosal tunnelling endoscopic resection.
- Minimally invasive: The saline lift technique (fluid injection into the submucosa separating the mucosa and muscle layers) has been in use for a long time. Achieving the lift, a relatively new technique, CO2is pumped, creating a space for the endoscopist/interventional gastroenterologist to navigate between the various layers of the submucosa. This procedure allows for interventions to be done within the lining of the bowel wall, an approach that cannot be achieved by laparoscopy or simple, flexible endoscopy. This new technique has led to the introduction of novel, less invasive, and sometimes unique surgical approaches to various gastrointestinal diseases.
- Colour correction and enhanced visualisation: Novel imaging techniques, which include image-enhanced endoscopy (IEE) and narrow-band imaging (NBI), are used in third-space endoscopy. Their utilisation combined with colour correction provides improved visualisation and clear discrimination of lesions and surrounding tissues, aiding in the detection and evaluation of conditions such as Barrett's oesophagus. Japanese endoscopic examination is usually done through the trans nasal route (sending the endoscope through the nose and into the gut), which results in a lower disease detection rate despite complex planning because of poor image quality. With the development of a third-generation ultrathin endoscope containing a high-quality metal-oxide semiconductor sensor, the colour differences between the lesion and the surrounding areas are distinct.
- Potential for robotic assistance: The concept of natural orifice transluminal endoscopic surgery (NOTES) broke the boundaries of conventional intraluminal gastrointestinal endoscopy. Many procedures which were traditionally part of the surgical field are now being addressed using interventional endoscopy.Robotising the endoscopy allowed the expansion of endoscopic procedural frontiers, thus enhancing the performance of minimally invasive interventional gastroenterologists. In third-space endoscopy, roboticisation could help overcome the technical obstacles, which could increase its adoption for complex endoscopic procedures. Artificial intelligence (AI) has shown promising developments in the realm of gastrointestinal endoscopy. As AI could be a promising tool to reduce the burden of endoscopic image review in oncological screening, its implementation can be expected in colour correction for image enhancement and cancer detection upon colour correction.
Third Space Endoscopy Cost in Hyderabad, India
The cost of Third Space Endoscopy in Hyderabad generally ranges from ₹1,20,000 to ₹3,80,000 (approx. US $1,445 – US $4,575).
The exact cost varies depending on the specific procedure performed (POEM, G-POEM, Z-POEM, STER), the underlying condition, length of myotomy/tunneling required, need for advanced accessories, anesthesia duration, surgeon expertise, and hospital facilities — including cashless treatment options, TPA corporate tie-ups, and assistance with medical insurance wherever applicable.
Cost Breakdown According to Type of Third Space Endoscopy Procedure
- POEM (Peroral Endoscopic Myotomy – Achalasia) – ₹1,20,000 – ₹2,50,000 (US $1,445 – US $3,010)
- G-POEM (Gastric Peroral Endoscopic Myotomy – Gastroparesis) – ₹1,50,000 – ₹3,50,000 (US $1,805 – US $4,210)
- Z-POEM (Zenker’s Diverticulum Myotomy) – ₹1,40,000 – ₹2,80,000 (US $1,690 – US $3,370)
- STER (Submucosal Tunneling Endoscopic Resection) – ₹1,60,000 – ₹3,80,000 (US $1,930 – US $4,575)
- Third Space Endoscopy with Additional Interventions (Stenting / Dilation / Hemostasis) – ₹1,40,000 – ₹3,50,000 (US $1,690 – US $4,210)
What Is the Cost of Third Space Endoscopy at PACE Hospitals, Hyderabad?
At PACE Hospitals, Hyderabad, the cost of Third Space Endoscopy typically ranges from ₹1,10,000 to ₹3,50,000 and above (approx. US $1,325 – US $4,210), making it a competitively priced advanced endoscopic option. However, the final cost depends on:
- Type of procedure (POEM / G-POEM / Z-POEM / STER)
- Length and complexity of the submucosal tunnel
- Need for myotomy, tumor resection, or diverticular correction
- Disposable accessories and electrosurgical equipment
- Anesthesia and hospital stay (day-care / overnight)
- Pre-procedure tests (manometry, EndoFLIP, CT/MRI)
- Postoperative medications and follow-up endoscopy
For routine POEM cases, costs fall toward the lower range; STER, Z-POEM, or extended myotomy procedures fall toward the higher end due to complexity and accessory use.
After a complete gastroenterology evaluation, imaging review, and procedure planning, our specialists will provide a personalised treatment plan and transparent cost estimate based on your condition.




