Arthritis Explained: Causes, Types & Diagnosis
PACE Hospitals
Written by: Editorial Team
Medically reviewed by: Dr. Shweta Bhardwaj - Consultant Rheumatologist and Clinical Immunologist
Overview
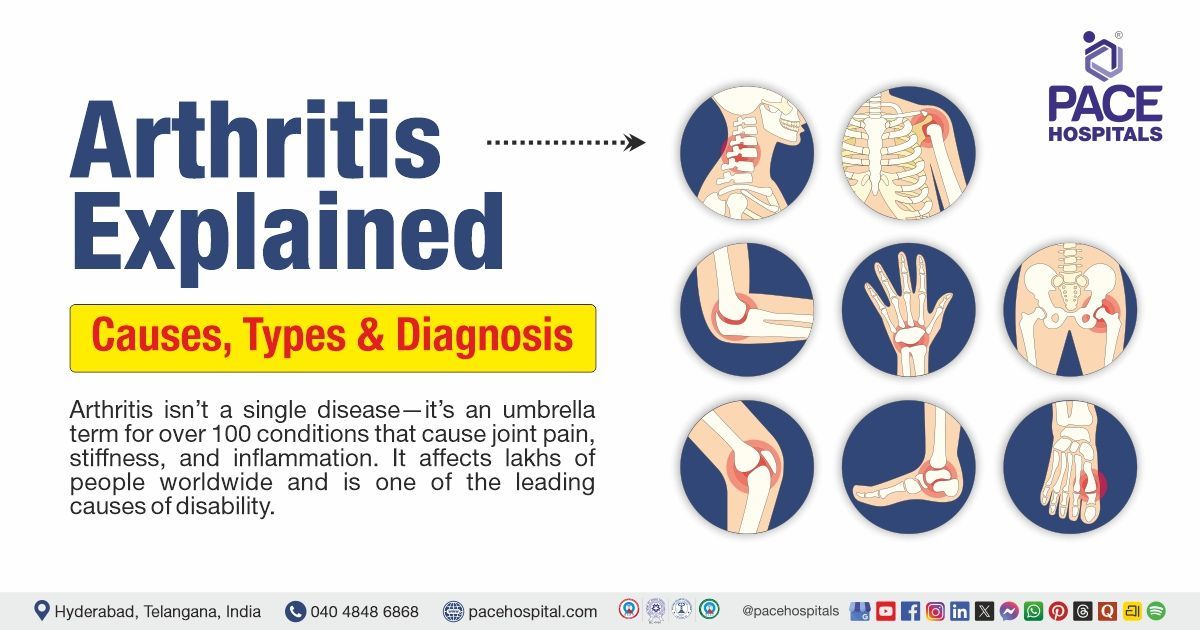
Arthritis is not a single disease — it’s a group of more than 100 disorders that cause inflammation, pain, and stiffness in the joints and surrounding tissues. It affects people of all ages, though it becomes more common as we grow older. Worldwide, arthritis is one of the leading causes of disability and chronic pain, impacting mobility, independence, and quality of life.
At PACE Hospitals, Hyderabad, our team of orthopaedic surgeons, rheumatologists, and physiotherapists provides advanced diagnosis, treatment, and joint care solutions for arthritis. From early screening to minimally invasive joint surgeries, we offer patient-centric care designed to restore movement and reduce pain.
Understanding arthritis — its causes, types, symptoms, and diagnostic approach — is the first step toward effective management and long-term joint health.
What Is Arthritis?
Arthritis is the inflammation of one or more joints, resulting in pain, stiffness, and a limited range of motion. Over time, chronic inflammation may damage cartilage, the smooth tissue that cushions joints, causing bones to rub together and resulting in edema, deformity, or loss of function.
Arthritis can be acute (short-term, due to infection or injury) or chronic (long-lasting and progressive). It may affect a single joint (monoarthritis) or multiple joints (polyarthritis).
Common Causes of Arthritis
Arthritis develops from a combination of genetic, environmental, metabolic, and lifestyle factors.
- Age and Wear & Tear: As we age, the protective cartilage naturally wears down, increasing friction and inflammation. This is the most common cause of osteoarthritis.
- Autoimmune Disorders: In some types, such as rheumatoid arthritis (RA), the immune system mistakenly attacks healthy joint tissue, causing chronic inflammation.
- Infections: Certain bacteria or viruses can enter the joint, causing septic arthritis. Immediate treatment is important to prevent permanent damage.
- Genetic Predisposition: A family history of arthritis, particularly autoimmune types, can increase the risk.
- Joint Injury or Overuse: Previous fractures, repetitive strain, or occupational stress can speed up cartilage breakdown and trigger inflammation.
- Obesity and Metabolic Factors: Excess weight increases joint load, especially on the knees and hips, while metabolic issues like gout lead to uric acid crystal buildup in joints.
- Hormonal and Gender Factors: Women are more prone to rheumatoid and lupus-related arthritis, especially post-menopause, due to hormonal changes that influence immune responses.
Main Types of Arthritis
Though there are over a hundred forms, these are the most prevalent and clinically significant:
Osteoarthritis (OA)
- The most common type, OA, is a degenerative joint disease resulting from cartilage wear and tear.
- Affected joints: knees, hips, spine, hands.
- Symptoms: joint pain after activity, stiffness in the morning, and swelling.
- Treatment: lifestyle modification, weight control, physiotherapy, and joint replacement surgery in severe cases.
Rheumatoid Arthritis (RA)
- It is an autoimmune disorder in which the body's immune system attacks the lining of its own joints (synovium).
- Key features: symmetrical joint involvement (both hands or knees), prolonged morning stiffness, fatigue, and low-grade fever.
- If untreated, it can lead to joint deformity and organ involvement.
- PACE Hospitals uses disease-modifying antirheumatic drugs (DMARDs) and biological therapies for targeted management.
Psoriatic Arthritis (PsA)
- Occurs in certain people with psoriasis, a persistent skin illness.
- Symptoms: red patches on the skin with joint pain, nail changes, and swollen fingers or toes.
Ankylosing Spondylitis (AS)
- A chronic inflammatory condition that mostly impacts the spine and sacroiliac joints.
- Symptoms: lower-back pain, stiffness that improves with movement, and reduced flexibility.
- Complication: fusion of spinal vertebrae (“bamboo spine”) in advanced stages.
Gout
- Metabolic arthritis is caused by uric acid buildup in the joints, which forms crystals.
- Common sites: big toe, ankle, or knees
- Triggers: High-protein diets, alcohol, and dehydration
- Treatment: It consists of lowering uric acid levels with drugs and dietary changes.
Juvenile Idiopathic Arthritis (JIA)
- It affects young people under the age of sixteen. The symptoms such as joint swelling, fever, and weariness. Early detection helps to prevent growth and mobility issues, whilst correct treatment can significantly improve long-term joint health and general quality of life.
Infectious (Septic) Arthritis
- Caused by bacterial or viral infections entering the joint. Requires urgent antibiotic therapy and joint drainage.
Lupus-Related Arthritis
- Seen in patients with systemic lupus erythematosus (SLE), an autoimmune disease that affects multiple organs.
Early Symptoms and Warning Signs
Recognizing arthritis early can help preserve joint function.
- Persistent joint pain or swelling
- Morning stiffness lasts more than 30 minutes
- Warmth or redness around joints
- Reduced flexibility or clicking sounds
- Autoimmune conditions can cause fatigue, low-grade fever, or weight loss
Diagnosis of Arthritis at PACE Hospitals
A correct diagnosis is required for successful treatment. PACE Hospitals in Hyderabad makes use of cutting-edge diagnostic procedures.
Detailed Medical History and Physical Examination
- Doctors examine symptom patterns, family history, injuries, and the influence of daily activities.
Laboratory Tests
- Blood Tests: ESR and CRP, which are markers of inflammation.
- Rheumatoid Factor and Anti-CCP: Used to confirm rheumatoid arthritis
- Uric Acid Test: It is used to diagnose gout
- ANA Test: It is used to detect lupus or other autoimmune conditions
Imaging studies
- X-rays can indicate joint constriction, bone spurs, and other abnormalities.
- Ultrasound and MRI can detect early soft-tissue inflammation and cartilage degradation.
- DEXA Scan: It assesses bone density, particularly in elderly people.
Joint Aspiration (Arthrocentesis)
- It involves examining joint fluid for infection, crystals, and inflammatory cells.
Arthroscopy
- A simple procedure using a small camera to look inside the joint, which can help diagnose problems and sometimes treat them.
Treatment Approach at PACE Hospitals
At PACE Hospitals, Hyderabad, arthritis management is multidisciplinary — combining medical, surgical, and lifestyle care.
Non-Surgical Management
- Medications include NSAIDs for pain, corticosteroids for inflammation, DMARDs or biologics for autoimmune arthritis.
- Physiotherapy & Rehabilitation to improve mobility and strengthen muscles.
- Dietary counselling needs to focus on anti-inflammatory foods, such as omega-3 fatty acids, turmeric, and fibre-rich vegetables.
- Weight Management Programs to reduce joint load.
Surgical Management
For advanced arthritis or severe joint damage:
- Arthroscopy for joint cleaning or cartilage repair.
- Osteotomy for realigning bones and redistributing weight.
- Joint Replacement (Knee, Hip, Shoulder): uses high-precision implants for long-term mobility.
PACE Hospitals uses computer-assisted and minimally invasive joint replacement techniques that ensure faster recovery and lasting results.
Lifestyle and Home Care Tips
- Maintain a healthy weight.
- Stay active — gentle exercises like swimming or yoga improve flexibility.
- Use heat or cold packs to help alleviate pain and stiffness.
- Avoid smoking and excess alcohol.
- Ensure adequate sleep and stress control.
- Schedule regular follow-ups to monitor joint health.
Why Choose PACE Hospitals for Arthritis Care?
- Team of expert orthopaedic surgeons and rheumatologists
- Advanced diagnostic imaging and laboratory support
- Comprehensive physiotherapy department
- Personalised pain-management and rehabilitation plans
- Cashless insurance facilities
- Ethical, evidence-based, and compassionate care
At PACE Hospitals in Hyderabad, every arthritis patient receives individualised care designed to preserve joint mobility and improve quality of life.
What is arthritis, and why does it occur?
Arthritis is joint inflammation that causes pain and stiffness. It occurs due to cartilage wear, immune system disorders, infections, or genetic factors.
Which type of arthritis is most common in India?
Osteoarthritis is the most common form, especially among women and older adults. It results from long-term wear and tear of joint cartilage.
Can young people develop arthritis?
Yes. Conditions like Juvenile Idiopathic Arthritis and autoimmune disorders can affect children and young adults, though it's less common.
What are the first signs of arthritis?
Early signs include joint pain, morning stiffness lasting over 30 minutes, and swelling or redness around the joints. Early evaluation is key.
How is arthritis diagnosed at PACE Hospitals?
Diagnosis includes blood tests (ESR, CRP, RF, Anti-CCP), X-rays, MRI, ultrasound, and joint fluid analysis for infection or crystals.
Is arthritis curable?
While most forms aren't fully curable, early diagnosis and proper treatment can control symptoms, prevent joint damage, and maintain mobility.
What foods help reduce arthritis pain?
Anti-inflammatory foods like fatty fish, turmeric, ginger, olive oil, green leafy vegetables, and nuts may help reduce joint inflammation.
Does exercise make arthritis worse?
No — regular low-impact exercises like walking or swimming strengthen muscles around joints and reduce pain without damaging cartilage.
When should I see a doctor for joint pain?
Consult a doctor if pain lasts longer than a week, worsens with activity, or is accompanied by swelling and stiffness. PACE Hospitals offers expert joint evaluation.
Why choose PACE Hospitals for arthritis treatment in Hyderabad?
PACE Hospitals provides advanced arthritis diagnosis, medical & surgical treatments, joint replacement surgery, and comprehensive rehabilitation under one roof.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles