Transurethral Resection of Bladder Tumour (TURBT)
PACE Hospitals
Overview
Transurethral Resection of Bladder Tumour (TURBT) is the first-line, minimally invasive surgical procedure used both to diagnose and treat bladder cancer. It allows the surgeon to remove visible bladder tumours and evaluate their grade and stage without open surgery.
At PACE Hospitals, Hyderabad, our urology and uro-oncology experts perform advanced TURBT using high-definition endoscopic systems, bipolar resection technology, and laser assistance to ensure safe tumour clearance with minimal bleeding and faster recovery.
This article explains what TURBT involves, its purpose, preparation, procedure, recovery, cost, and the modern techniques used at PACE Hospitals.
What Is TURBT?
TURBT stands for Transurethral Resection of Bladder Tumour.
It is performed through the urethra, using a special instrument called a resectoscope inserted into the bladder under general or spinal anaesthesia. No external incision is required.
During the procedure, the surgeon:
- Locates the tumour using a camera and light source.
- Removes the tumour piece by piece using an electrical loop.
- Sends tissue samples to a laboratory for histopathological examination (biopsy) to confirm the type and stage of cancer.
Purpose of TURBT
TURBT is both diagnostic and therapeutic. It helps:
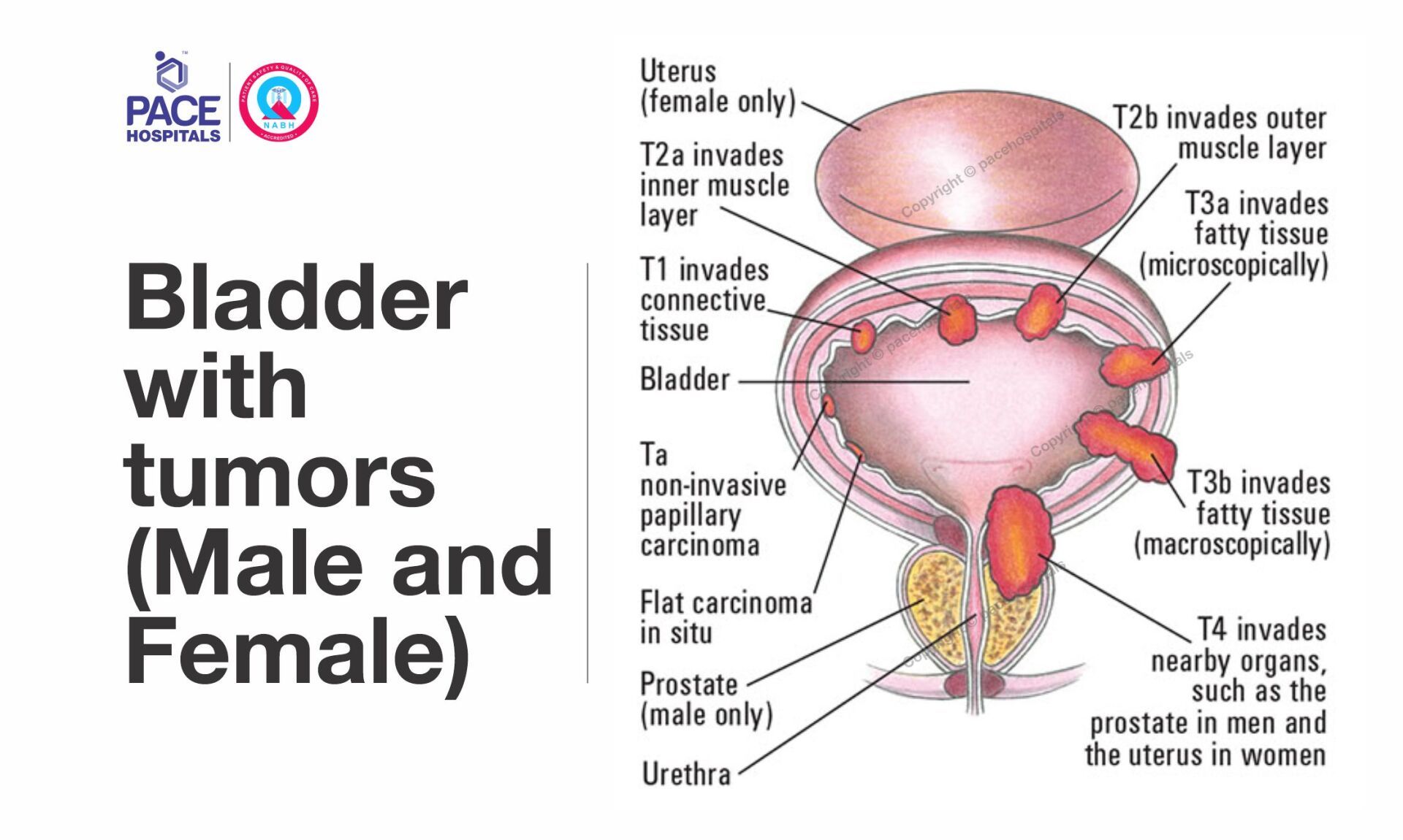
- Confirm whether a bladder mass is cancerous or benign.
- Determine tumour grade (low/high) and stage (superficial/invasive).
- Remove visible tumours completely for non-muscle-invasive bladder cancer (NMIBC).
- Control bleeding and prevent obstruction of urinary flow.
- Prepare patients for additional therapy such as intravesical BCG or chemotherapy if required.
Who Needs TURBT?
A urologist may recommend TURBT if you experience:
- Blood in urine (hematuria)
- Frequent urination or burning
- Lower abdominal pain or discomfort
- Bladder mass detected on ultrasound or CT scan
Early evaluation is crucial. Bladder cancers caught at an early stage are highly treatable with TURBT.
Pre-Procedure Evaluation at PACE Hospitals
Before TURBT, patients undergo a comprehensive pre-operative assessment:
- Urine tests – to detect infection or abnormal cells.
- Blood tests – kidney function, coagulation profile.
- Ultrasound / CT Urogram / Cystoscopy – to visualize tumour location, size, and multiplicity.
- Anaesthesia evaluation – to decide between spinal or general anaesthesia.
PACE Hospitals provides integrated diagnostics, ensuring same-day evaluation and surgery planning for most patients.
How the TURBT Procedure Is Done
- Anaesthesia and Positioning: The patient receives spinal or general anaesthesia and is placed in the lithotomy position.
- Insertion of Resectoscope: The urologist inserts a resectoscope into the bladder through the urethra.
- Tumour Resection
- The surgeon removes tumour tissue using a wire loop that cuts and cauterises simultaneously.
- Deep resection may be performed to include muscular tissue for accurate staging.
- Specimen Collection: Removed tissue is sent to pathology for microscopic analysis.
- Bladder Irrigation: After resection, the bladder is irrigated to flush out remaining fragments and to prevent clot formation.
- Post-Operative Instillation (Chemotherapy / BCG): In many cases, a single dose of intravesical chemotherapy is administered immediately after TURBT to reduce recurrence.
Duration and Hospital Stay
- Surgery Time: 30 – 90 minutes (depending on tumour size and number).
- Hospital Stay: 1 – 2 days.
- Catheter Removal: Usually after 24 – 48 hours.
- Return to Work: Within 5 – 7 days for most patients.
TURBT Cost at PACE Hospitals Hyderabad
At PACE Hospitals, the cost of Transurethral Resection of Bladder Tumour (TURBT) ranges between
₹ 60,000 to ₹ 1,20,000 (approximately USD 720 – 1,450),
depending on:
- Tumour complexity (size and number)
- Type of resection (bipolar / laser assisted)
- Hospital stay and room category
- Need for intravesical chemotherapy or BCG instillation
Cashless insurance and financing options are available at PACE Hospitals, Hitech City and Madinaguda branches.
Recovery and Aftercare
After TURBT, mild burning or blood-tinged urine for a few days is normal. Patients are advised to:
- Drink plenty of fluids (2–3 litres/day).
- Avoid strenuous activity for one week.
- Take prescribed antibiotics and pain relievers.
- Report fever, heavy bleeding, or clot retention immediately.
Follow-up cystoscopy at 3 months is essential to detect any recurrence.
PACE Hospitals provides long-term surveillance programs for bladder cancer that include routine ultrasound follow-up, urine cytology, and cystoscopic monitoring.
Risks and Possible Complications
When performed by an experienced urologists, TURBT is usually safe, but there are some risks:
- Minor bleeding or clot retention
- Perforation of the bladder wall (rare)
- Bladder infection or irritation
- Recurrence of tumour requiring repeat TURBT
Early detection of recurrence through scheduled follow-ups is crucial to prevent progression.
Advances in TURBT at PACE Hospitals
PACE Hospitals Hyderabad employs next-generation endoscopic technologies for precision bladder cancer surgery:
- Bipolar Plasma Kinetic Resection – reduces bleeding and thermal damage.
- Blue Light Cystoscopy & Narrow-Band Imaging (NBI) – enhances tumour visualization.
- Laser-Assisted TURBT – for select superficial tumours with minimal collateral injury.
- Intravesical Therapy Unit – for post-surgery chemotherapy and immunotherapy.
These technologies enable faster recovery, reduced recurrence rates, and superior outcomes.
Life After TURBT
With early diagnosis and complete tumour resection, most patients can lead a normal, active life.
The main goals of long-term care are monitoring, recurrence prevention, and following a lifestyle that is healthy for the bladder, which includes:
- Staying hydrated
- Avoiding tobacco and chemical exposure
- Maintaining regular urology check-ups
- Following medical therapy, if recommended
PACE Hospitals provides comprehensive care with urologists, oncologists, and nurses specializing in the management of bladder cancer.
FAQs on Transurethral Resection of Bladder Tumour (TURBT)
What is TURBT surgery?
TURBT stands for Transurethral Resection of Bladder Tumour — a minimally invasive procedure to remove bladder tumours through the urethra without any external cuts.
Why is TURBT done?
It is performed to diagnose and treat bladder cancer by removing visible tumours and collecting samples to determine their grade and stage.
How long does TURBT take, and what is the recovery time?
The surgery takes about 30–90 minutes. Most patients are discharged within 24–48 hours and resume normal activities in 5–7 days.
Is TURBT painful?
No. The procedure is performed under spinal or general anaesthesia. Mild burning or blood in urine after surgery is temporary and manageable.
What is the cost of TURBT surgery in Hyderabad?
At PACE Hospitals, the cost ranges from ₹ 60,000 to ₹ 1,20,000 (USD 720 – 1,450) depending on case complexity, equipment, and room type.
Will I need chemotherapy after TURBT?
Some patients receive a single dose of intravesical chemotherapy after TURBT to prevent recurrence. Further treatment depends on the tumour stage and biopsy report.
Can a bladder tumour recur after TURBT?
Yes, recurrence can occur in up to 40–50 % of cases, which is why regular cystoscopy and urine tests are important for early detection and management.
What are the risks of TURBT surgery?
Risks include mild bleeding, infection, and rare bladder wall perforation. At PACE Hospitals, advanced bipolar resection techniques reduce these risks.
Is hospitalization required for TURBT?
Yes. A short stay of 1–2 days is recommended to monitor urine output and provide catheter care after the procedure.
Why choose PACE Hospitals for TURBT in Hyderabad?
PACE Hospitals offers cutting-edge urology facilities, experienced uro-oncologists, advanced endoscopic equipment, and cashless insurance options for TURBT patients.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868