World Antimicrobial Awareness Week (WAAW), 2025 - Theme and Importance
PACE Hospitals
World Antimicrobial Awareness Week (WAAW) is a global healthcare event focused on preventing the emergence, and spread of antibiotic resistance; and promoting best practices among the public, health workers, and policymakers by raising awareness of the issue worldwide during the week of November 18 to November 24.
Previously (before 2020), this week was known as "World Antibiotic Awareness Week”. From 2020 onward, it included all antimicrobial such as antibiotics, antifungals, antiparasitic drugs, and antiviral drugs.

World Antimicrobial Awareness Week 2025 Theme
This year, 2025, the World Antimicrobial Awareness Week theme is "Act Now: Protect Our Present, Secure Our Future". This theme emphasizes the urgent need for bold, united action to address antimicrobial resistance (AMR), highlighting that AMR is a current global threat impacting health, food systems, the environment, and economies, requiring immediate and sustained efforts across all sectors.
Year by year theme of World Antimicrobial Awareness Week
- World Antimicrobial Awareness Week 2024 Theme: Educate. Advocate. Act now.
- World Antimicrobial Awareness Week 2023 Theme: Preventing Antimicrobial Resistance Together
- World Antimicrobial Awareness Week 2022 Theme: Preventing Antimicrobial Resistance Together
- World Antimicrobial Awareness Week 2021 Theme: Spread Awareness, Stop Resistance
- World Antimicrobial Awareness Week 2020 Theme: United to preserve antimicrobials
- World Antibiotic Awareness Week 2019 Theme: The future of antibiotics depends on us all
- World Antibiotic Awareness Week 2018 Theme: Change Can’t Wait. Our Time with Antibiotics is Running Out
- World Antibiotic Awareness Week 2017 Theme: Seek advice from a qualified healthcare professional before taking antibiotics
- World Antibiotic Awareness Week 2016 Theme: Antibiotics: Handle with Care
- World Antibiotic Awareness Week 2015 Theme: Antibiotics: Handle with Care
Necessity for the Antimicrobial Resistance Awareness
The development of antimicrobial resistance (AMR) occurs when pathogens (such as bacteria, viruses, fungi, and parasites) evolve to become immune to treatment with antimicrobials, causing drug resistance, especially with the rapid global spread of multi- and pan-resistant bacteria, for which the current available antibiotics are ineffective. Due to this, antimicrobial drugs lose their efficacy, making the treatment more challenging or impossible in some cases. The effectiveness of modern medicine in treating infections, including those that occur during major surgery and cancer chemotherapy, would be in jeopardy without the use of effective antimicrobials. Considering this, the World Health Organization (WHO) has included AMR in its list of the top 10 dangers to global public health.
In addition to this, the lack of novel antimicrobials in clinical development has been a major problem. The WHO identified only six antibiotics as innovative out of 32 antibiotics that are under clinical development and targeting WHO's priority diseases in 2019. Moreover, the general population's inability to obtain high-quality antimicrobials remains a severe issue. Antibiotic shortages are wreaking havoc globally, regardless of level of development, and are especially harmful to healthcare systems.
Drug resistance stats:
- In 2019, it was projected that 12.7% (95% uncertainty interval 0.911% - 1.71%) of all deaths worldwide were caused by drug-resistant illnesses, based on an analysis of 88 different pathogen-drug combinations.
- Globally, approximately 3.4% of newly diagnosed cases and 18% of previously treated patients in 2018 were diagnosed with multi-drug resistance tuberculosis (MDR-TB)/rifampicin-resistant TB, and the presence of new 'last resort' tuberculosis medications (used to treat MDR-TB) are also been on impending threat due to emergence of resistance.
- Countries reporting to the Global Antimicrobial Resistance and Use Surveillance System (GLASS) found a range of resistance to the antibiotic ciprofloxacin from 8.4% to 92.96% for Escherichia coli and from 4.1% to 79.4% for Klebsiella pneumoniae.
- The rising incidence of drug-resistant fungal infections exasperating the already challenging therapeutic environment. Existing treatability concerns, such as toxicity, make many fungal infections difficult to treat, especially in patients with concurrent underlying infections (e.g., HIV). Despite being one of the most often treated invasive fungal infections, candida auris is becoming increasingly resistant to antifungal drugs like fluconazole, amphotericin B, and voriconazole, and there are even reports of rising caspofungin resistance.
- It was reported, as per the WHO, that in sub-Saharan Africa, over 50% of the infants newly diagnosed with HIV carry a virus that is resistant to non-nucleoside reverse transcriptase inhibitors (antiviral class of drug).
- The misuse of broad-spectrum antimicrobials is rampant in India, contributing to an annual rise in resistance of 5-10%.
- In a study conducted in India, the antibiotic (carbapenem) used to treat Acinetobacter baumannii bacteria was found to be resistant in 87.5 percent of the sample population, restricting treatment choices.
- There was a 22% rise in resistance to the antibiotic (Imipenem) from 2016 (14%) to 2021 (36%) that is used to treat infections caused by the bacteria E.coli
- Methicillin-Resistant Staphylococcus aureus rate had shown 14.2% increase from last 5 years (2016 to 2021).
History of World Antimicrobial Awareness Week
In May 2015, the 68th World Health Assembly supported a global action plan to address the growing problem of antibiotic and other antimicrobial resistance. This came after European governments adopted a strategic action plan on antibiotic resistance in 2011. One of the primary goals of these strategies is to raise antimicrobial resistance awareness and understanding through effective communication, education, and training. The Tripartite Executive Committee decided to set all future World Antimicrobial Awareness Week (WAAW) dates as 18 to 24 November.
Drivers of Antimicrobial Resistance (AMR)
Multidrug-resistant (MDR) are the alarming trend toward widespread antimicrobial resistance (AMR) that is being seen in hospitals and other healthcare settings, as well as in the general population. It's a big contributor to health problems and raises expenses for individuals and society. It develops gradually over time, mainly as a result of genetic alterations.
- Inappropriate (misuse and overuse) usage of antimicrobials
- Lack of clean water access, sanitation, and hygiene for both humans and animals
- Poor infection, disease prevention, control in health-care facilities and farms
- Poor access to quality, affordable medicines, vaccines and diagnostics
- Lack of awareness and knowledge
- Lack of enforcement of legislation
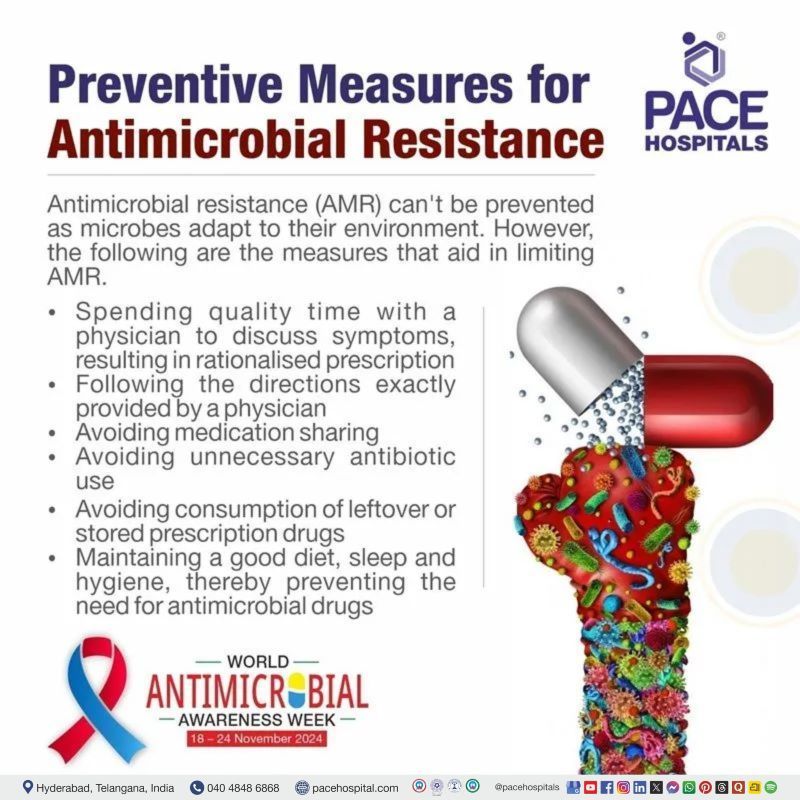
Preventive Measures for Antimicrobial Resistance
Antimicrobial resistance (AMR) can't be prevented as microbes adapt to their environment. However, the following are the measures that aid in limiting AMR:
- Spending quality time with a physician to discuss symptoms, resulting in rationalised prescription
- Following the directions exactly provided by a physician
- Avoiding medication sharing
- Avoiding unnecessary antibiotic use
- Avoiding consumption of leftover or stored prescription drugs
- Maintaining a good diet, sleep and hygiene, thereby preventing the need for antimicrobial drugs
Approaches for Combating of Antimicrobial Resistance (AMR)
Misuse and overuse of antibiotics, along with ineffective infection prevention and control, speed up the development of antibiotic-resistant bacteria. To lessen the impact and slow the development of resistance, measures can be implemented on an international, national, community, hospital or health care setting, as well as on an individual (physician, health care professionals, patient) scale.
International measures:
- Collaboration between governments, nongovernmental organizations, professional groups, and international agencies should be increased.
- Emerging systems for monitoring antimicrobial consumption and its resistance
- Development of international strategies for preventing the circulation of counterfeit antimicrobials
- Granting more funds for the research and development of new drugs and vaccines.
- Establishing new, and reinforcing current, programmes to control AMR.
National measures:
- A national committee should be formed to track the effects of antibiotic resistance. In addition to this, developing and executing national standard treatment guidelines, having an essential drug list (EDL), and increasing immunisation coverage are very desirable at the national level.
- Implementation of a strict national antimicrobial resistance policy, which aims to understand the emergence, spread, and factors influencing AMR; to establish an antimicrobial programme; to rationalise antimicrobial use; and to promote the development of newer, more effective antimicrobials.
Community measures:
- Mandatory public and professional education towards rational use of antibiotics is needed.
- Regulatory control of over-the-counter use of antibiotics.
- Optimisation of antibiotic selection as per the guideline (dosing, route of administration, and duration of therapy).
- Prevention of infection with the use of alcohol-based hand rubs.
Hospital or health care measures:
- Measures to prevent and control infections at health-care facilities:
- The formation of a committee to oversee infection control (IPC).
- Maintenance of good hand hygiene practices.
- Accurate diagnosis and treatment of infection.
- Rational antimicrobial use.
- Monitoring of antibiotic resistance and antibiotic use.
- Improving the antimicrobial quality and supply chain.
- Good microbiology practices.
Physician / Health care providers/ Patient measures
- Compliance with local infection control and antibiotic use policies and timely notification of resistant cases to IPC by the physician.
- By educating nurses and other health care personnel about AMR and aseptic techniques may aid in infection management, as they have direct contact with the patients.
- Concerns about antibiotic use and optimal dosing should be addressed by pharmacists with both patients and clinicians. In addition to this, the pharmacist should educate the patient regarding antibiotic use and the necessity of following the prescribed treatment regime.
The patient should follow these to curb AMR:
- Aseptic protocol for any procedures.
- Control the spread of diseases by covering the mouth or wearing masks while coughing or sneezing, and by taking timely vaccinations.
- Adherence to the antimicrobial regime and antibiotics.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868