Cystocele (Prolapsed Bladder) - Symptoms, Causes, Risk Factors, Treatment, Prevention
PACE Hospitals
Cystocele definition
A cystocele, also known as a prolapsed bladder, develops when the bladder moves out of its normal position in the pelvis and pushes onto the vaginal wall and perineum (The part between the anus and the genitals). A cystocele is caused by weakened or damaged muscles and connective tissues that support the bladder and vaginal wall.
However, in males, this condition is relatively uncommon. Men may have different types of bladder hernias, such as scrotal cystoceles, in which the bladder herniates into the scrotum. A
Urologist or Urogynecologist treats cystocele.
Cystocele meaning
The word "cystocele" comes from two Greek words, "kystis"- which means "bladder", and "kele"- which is used to describe "tumour", "rupture", or "hernia". It is believed to have developed between 1805 and 1815 and was first documented in English in 1811 by physician and medical writer Robert Hooper.
Prevalence of cystocele worldwide
Cystocele is the most common kind of pelvic organ prolapse (POP). Cystocele has an incidence of approximately 9 per 100 women, and is most frequent in older women, with the largest frequency of symptoms occurring between the ages of 70 and 79 years old. One study discovered that 34.3% of women who participated in a hormone replacement therapy clinical trial had cystocele, while 32.9% of women who had undergone a hysterectomy also had cystocele.
Cystocele types
Based on their anatomical placement, cystoceles are characterized as:
- Apical
- Medial
- Lateral
Apical defect: The apical defect is located in the upper portion of the vagina and is developed due to endopelvic fascial defect. It leads to the development of stress urinary incontinence (SUI) by interrupting the urethra-vesical junction.
Medial defect: Caused by the separation of the pubocervical fascia from connective tissue around the cervix and disruption to uterosacral ligaments.
Lateral defect: The vaginal wall separates from the arcus tendinous, resulting in a decrease in the lateral vaginal sulcus on one or both sides.
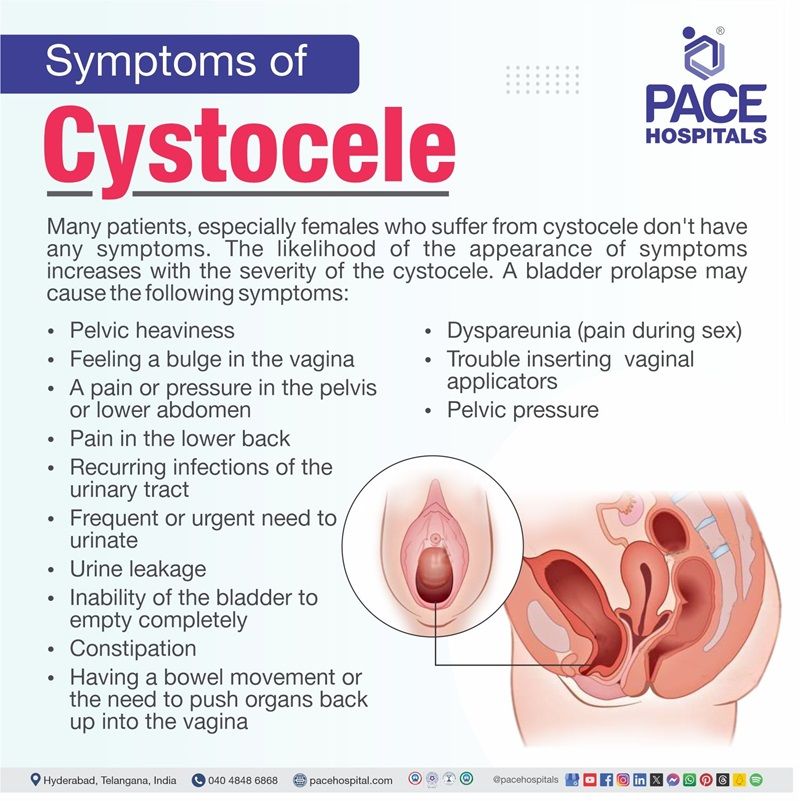
Cystocele symptoms
Many patients, especially females who suffer from cystocele don't have any symptoms. The likelihood of the appearance of symptoms increases with the severity of the cystocele. A bladder prolapse may cause the following symptoms:
- Sensation of fullness or heaviness in the pelvis
- Feeling a bulge in the vagina
- A pain or pressure in the pelvis or lower abdomen
- Pain in the lower back
- Recurring infections of the urinary tract
- Frequent or urgent need to urinate
- Urine leakage
- Inability of the bladder to completely empty the bladder
- Constipation
- Having a bowel movement or the need to push organs back up into the vagina
- Dyspareunia (pain during sex)
- Trouble inserting tampons or vaginal applicators
- Pelvic pressure that worsens with standing, lifting, coughing, or as the day progresses
Cystocele causes and risk factors
Addressing the causes and risk factors of bladder prolapse is crucial for prevention, early discovery, and successful management. By investigating these factors, we can learn more about how this disorder develops and identify those who may be at a higher risk. This research will aid in developing focused therapies and preventive strategies to address and lessen the impact of bladder prolapse on affected people's quality of life. Below are some of the causes and risk factors of cystocele:
- Menopause and aging: Oestrogen (female reproductive hormone) levels in women, tend to decrease after menopause. Oestrogen is said to maintain the strength of the pelvic floor muscles. Due to decreased levels of oestrogen in menopausal women, the bladder may protrude into the vaginal wall.
- Constipation and straining: Straining during bowel motions, having a long-term coughing problem, or suffering from chronic constipation can all cause pelvic floor muscle injury leading to prolapse.
- Being overweight: Elevated body mass index (BMI) is a major lifestyle factor that influences pelvic organ prolapse. The most likely mechanism of pelvic organ prolapse development among obese people is a rise in intra-abdominal pressure that may lead to the weakening of the pelvic floor muscles.
- Repeated heavy lifting: Heavy lifting raises abdominal pressure and strains the muscles and ligaments that support the pelvic organs.
- An inherited condition that causes a higher risk of prolapse: Despite the fact that there are no known particular genes responsible for the development of vaginal prolapse, a review of 16 research studies found that women with pelvic prolapse are highly likely to have a family member suffering from this disorder.
- Previous pelvic surgery : Damage is done to the endopelvic fascia (tissue covering the pelvic floor and joining them to the surrounding bone and muscle) structures and nerves after pelvic surgery, particularly surgical removal of uterus (hysterectomy). This raises the possibility of bladder herniation (prolapse) and vaginal prolapse.
- Pregnancy and childbirth:
Pregnancy and childbirth can lead to bladder prolapse, by affecting the muscles of the pelvic floor and nerves and damaging the muscles that support the pelvic organs. This can happen during pregnancy, vaginal birth, or both.
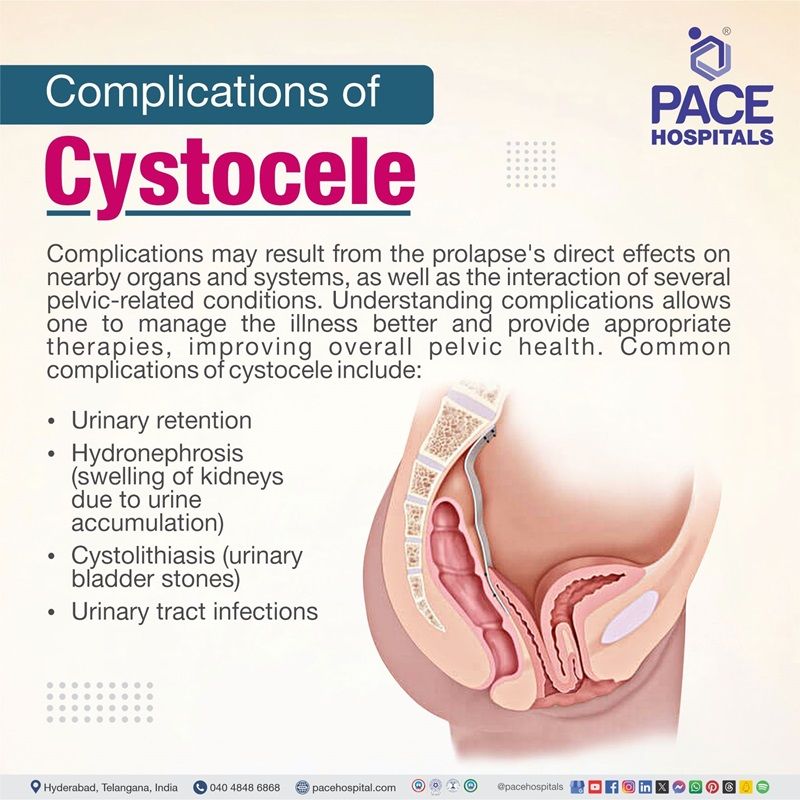
Cystocele complications
Complications may result from the prolapse's direct effects on nearby organs and systems, as well as the interaction of several pelvic-related conditions. Understanding complications allows one to manage the illness better and provide appropriate therapies, improving overall pelvic health. Common complications of cystocele include:
- Urinary retention: It may be difficult to fully empty the bladder due to pressure from a cystocele on the urethra.
- Hydronephrosis (swelling of kidneys due to urine accumulation): In rare situations, a cystocele may induce an obstruction in the ureters, resulting in urine buildup in the kidney, potentially leading to kidney damage.
- Cystolithiasis (urinary bladder stones): The pelvic muscles and tissues that support the bladder can weaken, allowing the bladder to slip from its original position. This can cause urine retention, which increases the risk of bladder stones.
- Urinary tract infections:
Due to difficulty in emptying the bladder completely, there is a high risk of developing recurrent urinary tract infections as a complication of pelvic organ prolapse (bladder prolapse).
Cystocele diagnosis
General physicians play an important role in the initial evaluation and management of bladder prolapse. However, if the symptoms persist or worsen, or if more advanced diagnostic tools and treatment choices are required, a general physician may refer the patient to a urologist.
To diagnose a cystocele, a urologist may ask about the symptoms and medical history and perform a physical exam, including a pelvic exam to check the lower abdomen. The urologist may also order medical tests to determine how advanced the cystocele is or to rule out other problems in the urinary tract or pelvis.
Medical tests
The urologist/urogynecologist may use one or more of the following tests to examine the urinary tract if the patients are experiencing symptoms related to the lower urinary tract or having problems emptying their bladder entirely.
- Postvoid residual urine measurement
- Voiding cystourethrogram
- Magnetic resonance imaging (MRI)
- Cystoscopy
- X-rays
- Ultrasound
Cystocele treatment
Depending on the grade of the cystocele the available treatment modalities to manage the cystocele include:
- Lifestyle modifications
- Pelvic floor exercises (Kegel exercises)
- Vaginal pessaries
- Hormone replacement therapy
- Surgical interventions
- Anterior colporrhaphy (Anterior vaginal repair)
- Sacrocolpopexy (sacral colpopexy)
Cystocele prevention
Bladder prolapse, or cystocele, is a disorder that has a substantial impact on quality of life. However, knowing and applying preventive techniques can play an important role in reducing its recurrence. Individuals who focus on preventive measures may lower their risk of developing cystocele and preserve better pelvic health.
Here are some lifestyle changes that may help prevent a prolapsed bladder:
- Indulging in pelvic floor exercises: Pelvic floor exercises, such as Kegels, can help strengthen the pelvic floor muscles and nerves, thereby controlling bladder prolapse symptoms and preventing them from worsening.
- Maintaining a healthy weight: Being overweight causes pressure on the pelvic region. Changing the diet and lifestyle by eating more fruits and vegetables and exercising on a regular basis may help to maintain the ideal body weight to prevent bladder prolapse.
- Avoiding heavy lifting and lifting correctly : Heavy lifting could damage the pelvic floor's muscles and connective tissues that support the bladder, uterus, and intestines.
- Preventing and treating constipation: Constipation can result in pelvic organ prolapse. It can also be a symptom caused due to bladder prolapse. Trying to prevent constipation and straining when defecating may help.
- Controlling chronic cough:
Coughing causes the pelvic floor to shift downward. Repeated or aggressive coughing can stretch the pelvic floor tissues.
Difference between Urethrocele and Cystocele
Urethrocele vs Cystocele
Understanding the differences between the various types of pelvic organ prolapse is critical for accurate diagnosis and therapy. Cystocele and urethrocele are two often seen disorders that involve pelvic organ protrusions but differ in their specific presentations and consequences. Below are some of the parameters that help in differentiating urethrocele and cystocele:
| Aspect | Urethrocele | Cystocele |
|---|---|---|
| Definition | Prolapse of the urethra | Prolapse of the bladder into the vagina |
| Location | Occurs in the urethra | Occurs in the bladder and vaginal wall |
| Symptoms | Urinary difficulties, Urinary incontinence and Pain during urination | Pelvic pressure or discomfort, Frequent urination and feeling of fullness or bulging in the vagina |
| Treatment | Pelvic floor exercises, Pessary (a device to support the urethra) and Surgery (for severe cases) | Pelvic floor exercises, Pessary (for mild cases) and Surgery (if symptoms are bothersome) |
Frequently Asked Questions (FAQs) on Cystocele
How to fix a prolapsed bladder without surgery?
If a cystocele, or bladder prolapse, is not severe, it can be treated non-surgically. The urologist might suggest non-surgical procedures such as pelvic floor exercises, pelvic floor physical therapy, pessaries, and lifestyle modifications such as avoiding heavy lifting, smoking cessation, etc.
Can a prolapsed bladder heal itself?
If bladder prolapse is asymptomatic (without symptoms), it typically doesn't need to be treated.in case of severe symptoms, they often do not go away on their own and may even get worse with time. Urologists/urogynecologists may recommend treatments such as pelvic floor exercises, vaginal pessaries, or surgery.
Can a prolapsed bladder cause bleeding?
Yes, bladder prolapse can result in bleeding in its severe stages. When organs prolapse, tissue irritation can happen, which results in bleeding. Prolapse-induced mucosal damage can also result in haematuria (blood in urine)
Can a prolapsed bladder cause bowel problems?
Yes, bladder prolapse might potentially cause gastrointestinal difficulties. When the bladder deviates from its normal position, it can induce pressure and alterations in the surrounding structures, including the rectum. This may lead to bowel problems.
What is the main cause of cystocele?
The main cause of cystocele is due to weakened pelvis. The pelvis can become weaker due to many reasons such as obesity, aging, childbirth, etc. It may also develop as a result of pelvic surgery, aberrant collagen, a familial history of cystocele, and persistently elevated intraabdominal pressure.
Can a prolapsed bladder cause constipation?
Yes. A prolapsed bladder may cause constipation. Bladder prolapse may disrupt the body's ability to pass stool, worsening or causing new constipation. This is because the prolapse might pull the rectum down.
Can a prolapsed bladder cause back pain?
Yes. Back pain due to bladder prolapse is frequently brought on by the pressure on the surrounding tissues and muscles of the pelvic floor. The pain might manifest as heaviness, fullness, or a dragging sensations in the vagina or lower abdomen.
Is bladder prolapse an emergency?
A prolapsed bladder, also known as a cystocele, is rarely fatal, but it can cause discomfort and make it difficult to empty the bladder. It is recommended to see a urologist/urogynecologist if an individual has any symptoms that disturb daily activities.
Is cystocele a hernia?
Yes, a cystocele is a hernia in which the bladder protrudes into the vaginal opening or anterior vaginal wall. It is sometimes referred to as a prolapsed bladder, herniated bladder, dropped bladder, or falling bladder. Cystocele is a persistent disorder that causes pelvic organ prolapse.
Can a prolapsed bladder be cancerous?
No, pelvic organ prolapse is unrelated to the development of any specific type of cancer. However, cancer can arise because a huge mass in the belly causes abdominal pressure due to a significant volume of fluid accumulates in the pelvis.
Should I see a urologist or gynecologist for a prolapsed bladder?
Male bladder prolapse is treated by urologists, who are specialists in the urinary tract and reproductive system. They have been trained in medical and surgical procedures. Women with bladder prolapse can be diagnosed and treated by urogynecologists, medical professionals, and surgeons who are specialize in the female reproductive and urinary systems.
Does bladder prolapse affect sexual function?
Bladder prolapse can impair sexual function. It may cause discomfort or pain during intercourse, and anatomical changes in the pelvic region might impair normal sexual function. Prolapse's psychological effects, such as body posture issues or symptom anxiety, can also have an impact on sexual intimacy. Open conversation with a urologist/urogynecologist and potential actions can aid in addressing these concerns.
What is the difference between cystocele and rectocele?
Cystocele and rectocele are both kinds of pelvic organ prolapse (POP) that develop when the pelvic floor weakens, allowing pelvic organs to protrude into the vaginal canal. While they have the same cause, they affect various organs and produce different symptoms. Rectocele is a condition in which the rectum protrudes into the vaginal wall due to weakening of the pelvis. The bladder will swell up against the front vaginal wall in case of a cystocele.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles











