Emergency Liver Transplant in a Young Mother with 2 Weeks of Coma and Severe Jaundice
PACE Hospitals
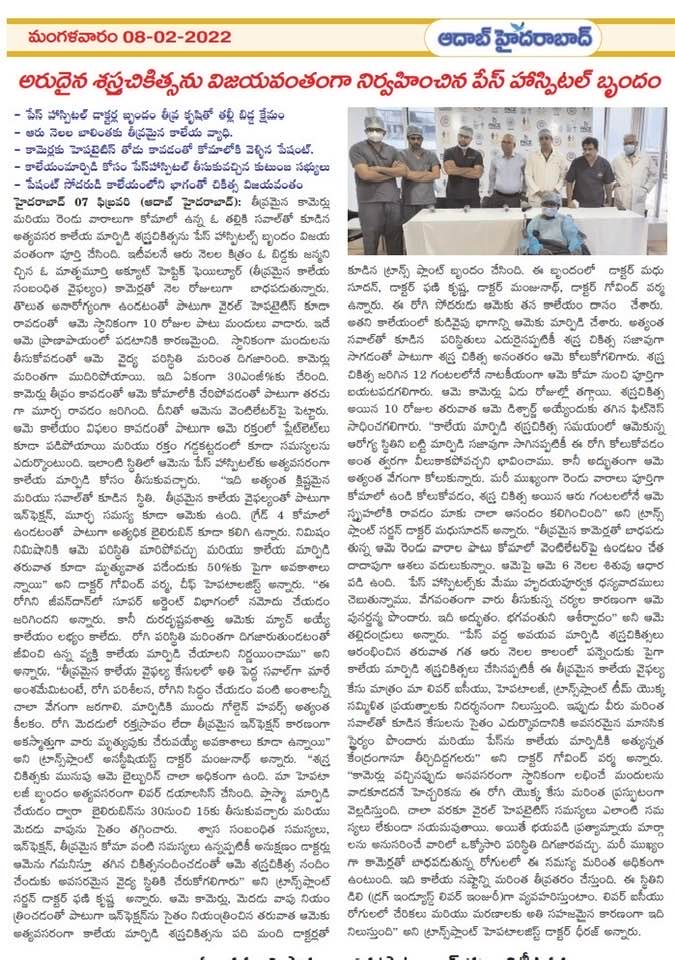
The PACE Hospitals Liver Transplant Team successfully performed a challenging emergency Liver Transplantation in a young mother with a 2-week coma and severe jaundice.
Introduction
A young mother, six months postpartum, suddenly faced a major medical crisis. About a month after developing viral hepatitis, she became jaundiced. Hoping for relief, she took native herbal medicine for ten days, but her condition deteriorated. Her bilirubin levels reached approximately 30 mg/dL, and she developed deep jaundice, progressed to coma, and suffered seizures. With severe bleeding tendencies and low platelet counts typical of acute liver failure, her family brought her to PACE Hospitals for an emergency liver transplant evaluation.
Case Summary
- Patient profile: A six-month postpartum woman with no history of chronic liver disease.
- Initial illness: She had viral hepatitis with jaundice lasting about one month.
- Self-medication: She took native medicine for ten days, after which her jaundice worsened significantly, and her bilirubin level increased to around 30 mg/dL.
- Clinical deterioration: She lapsed into a deep coma with seizures and needed mechanical ventilation. Her platelets were very low, and her blood wouldn't clot, consistent with classic acute liver failure.
- Transfer to transplant centre: She was referred to PACE Hospitals, Hyderabad, India, for urgent evaluation and advanced management.
Challenges in Management
Dr Govind Verma, the chief hepatologist at PACE Hospitals, described the situation as a race against time. The patient had severe infection, seizures and a grade IV coma with extremely high bilirubin. In acute liver failure, conditions can change from minute to minute, and survival after transplant can be precarious.
The team placed her on the super urgent transplant list through the Jeevandan organ donation programme. When no suitable organ became available, and her condition continued to deteriorate, they decided to move forward with a living donor transplant.
Bridging Therapy
Before surgery, the hepatology team performed urgent plasma exchange (liver dialysis) to lower her bilirubin from approximately 30 mg/dL to 15 mg/dL and reduce brain swelling. Continuous monitoring and meticulous intensive care were needed to manage respiratory complications, infection and deep coma until she could undergo transplantation.
Transplant Procedure and Donor Information
A ten member transplant team, including Dr CH Madhusudhan, Dr Suresh Kumar S, Dr Govind Verma and other medical staff, performed the emergency living donor transplant. The patient's brother donated the right half of his liver. Despite the complexities of surgery and the patient's critical condition, both the operation and the donor procedure were smooth.
Outcome and Follow Up
The outcome was dramatic. The patient's coma reversed within 12 hours after surgery. Her jaundice improved rapidly and normalized within seven days. By postoperative day 10, she was fit for discharge. Dr CH Madhusudhan commented on the remarkable recovery: "Considering her deplorable condition at transplant, despite a very smooth transplant, we were keeping our fingers crossed. But her miraculously rapid recovery, especially from a complete coma for two weeks to fully conscious within six hours of transplant, was very heartening."
Her parents expressed gratitude: "We had almost given up hope after two weeks of coma on a ventilator with such high jaundice. She has a six month old baby depending on her. We are very thankful to PACE Hospitals for their immediate action and for giving her a second life. It is a miracle and God's blessing."
Dr Govind Verma highlighted that PACE Hospitals performed over a dozen liver transplants in the past six months. This case underscores the combined efforts of the liver ICU, hepatology and transplant teams and establishes PACE Hospitals as a centre of excellence for liver transplantation.
Lessons and Warnings
Dr Govind Verma, Interventional Gastroenterologist and Hepatologist, used the case to warn against unregulated treatments: "This case highlights a warning against unnecessary usage of native medicine in jaundice patients. Most viral hepatitis resolves without any problem; the affected individual has to be patient, but mostly in panic, they go for alternative therapy, which is very dangerous in jaundiced patients. It worsens the liver damage, causing drug induced liver injury (DILI), which is one of the commonest causes of admission and death in the liver ICU." The case underscores the importance of:
- Avoid self-medication: Herbal preparations and over-the-counter medicines can worsen jaundice and further injure the liver.
- Seek early specialist care: Early assessment at a dedicated liver centre greatly improves the chances of survival in acute liver failure.
- Support organ donation: Both living-donor and deceased-donor programmes, including Jeevandan, play a vital role in providing life-saving organs when time is limited.
Conclusion
This young mother's case shows how dangerous acute liver failure can be and how living donor liver transplantation can save lives when done at the right time. After self-medicating, her condition got worse very quickly, so she needed immediate care, close monitoring, and a well-coordinated transplant team. At PACE Hospitals, quick decisions and cutting-edge medical care led to a remarkable recovery, with the patient waking up from a coma within hours and being discharged within ten days. The case also serves as a critical reminder to stay away from treatments that aren't regulated and to get medical help right away for jaundice and hepatitis.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles