Esophageal Cancer - Symptoms, Causes, Complications and Prevention
PACE Hospitals
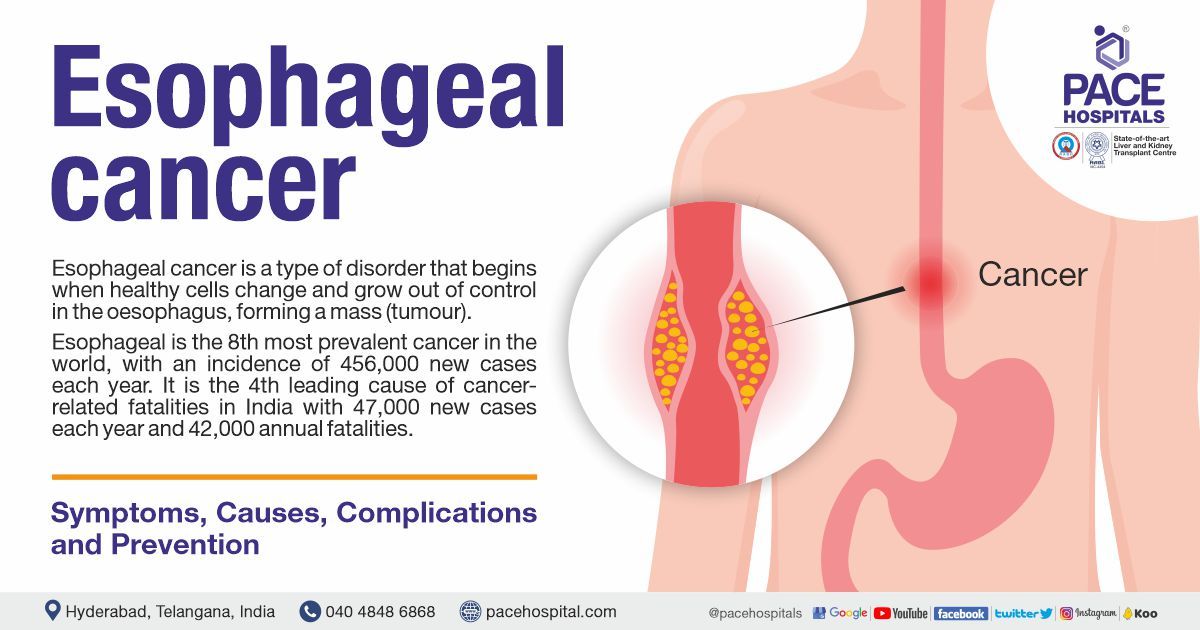
Esophageal cancer definition
Esophageal cancer is a type of disorder that begins when healthy cells change and grow out of control in the oesophagus, forming a mass (tumour).
The esophagus is a 10-inch-long, muscular, hollow tube that links the throat to the stomach. It is a portion of the gastrointestinal tract. When a person swallows, the oesophagus's walls contract to force food downward into the stomach through peristalsis (involuntary constriction and relaxation of the muscles, creating wave-like movements pushing the contents forward).
Esophageal cancer occurs when healthy cells transform and expand uncontrollably, becoming a tumour. A tumour may be malignant (may develop and spread to other organs) or benign (grows but does not spread). Esophageal cancer, starts in the oesophagus' lining cells.
If it spreads through the esophageal wall, it can travel to lymph nodes (small, bean-shaped organs that help fight infection), blood vessels in the chest and other organs. Esophageal cancer can also spread to the lungs, liver, stomach, and other parts of the body.
What are the types of esophageal cancer?
There are mainly 2 main types of esophageal cancer, the treatment for each of these kinds of esophageal cancer is same. They are:
- Squamous cell carcinoma: Begins in the esophageal lining of squamous cells, usually beginning in the upper and middle part of the oesophagus.
- Adenocarcinoma: Originates in the glandular tissue at the junction of esophagus and the stomach.
- The other types of very uncommon esophageal tumours (<1%) include:
- small cell neuroendocrine tumours
- sarcoma
- lymphomas
Esophageal cancer prevalence
Esophageal cancer is so common that it is the 8th most prevalent cancer in the world, with an incidence of 4,56,000 new cases each year.
- It is the 4th leading cause of cancer-related fatalities in India.
- The incidence of esophageal cancer has increased significantly around the globe.
- The esophageal cancer is of two types - esophageal adenocarcinoma and esophageal squamous cell carcinoma.
- The prevalence of esophageal cancer varies widely by area.
- While nations with a higher Human Development Index (HDI) have a greater prevalence of esophageal adenocarcinoma and nations with low HDI tend to contain greater prevalence of esophageal squamous cell carcinoma.
- In nations with a low HDI, such as India, the incidence of esophageal squamous cell carcinoma is greater.
- Currently, esophageal squamous cell carcinoma is greater is the most prevalent form of esophageal cancer in the Indian subcontinent, with the distal part of the esophagus being the most frequent site.
- In India,
around 47,000 new cases are recorded annually, and 42,000 fatalities are reported annually.
Esophageal cancer symptoms
There are various sign and symptoms of esophageal cancer. It is not necessary that they all must be presented in all the patients. The esophageal cancer symptoms include:
- Difficulty and pain while swallowing, particularly solid food.
- With the growth of tumour, it can block the pathway to the stomach and in that stage even liquids could be painful to swallow.
- Pressure or burning in the chest
- Indigestion or heartburn
- Vomiting
- Frequent choking on food
- Unexplained weight loss
- Coughing or hoarseness in voice
- Pain behind the breastbone or in the throat
Also, it must be understood that merely the manifestation of sign or symptoms may not be concluded as esophageal cancer. These symptoms can also be seen in other medical conditions as well.
Esophageal cancer causes
While there is no clear answer, various risk factors (such as tobacco and alcohol) have been identified promoting esophageal cancer by disrupting the DNA in esophagus-lining cells.
DNA mutations alter tumour suppressor genes that govern cell division. Altering the function of tumour suppressor genes causes uncontrolled cell growth. Esophageal cancer requires changes in numerous genes. DNA mutations are of 2 types - inherited and acquired gene mutations
- Inherited gene mutations: Some DNA mutations are inherited and present in all cells. Rarely, these mutations cause esophageal cancer.
- Acquired gene mutations: Most cancer-causing mutations are acquired which occur within a person's lifetime and aren't inherited. Tobacco and alcohol usage are the most common factors which have a role in producing acquired mutations, although the main reason is unknown.
Risk factors and environmental causes of esophageal cancer
There are various risk factors for esophageal cancer. Esophageal squamous cell carcinoma develops from tiny polypoid excrescences (distinct outgrowth, resulting from disease/abnormality), denuded epithelium (loss of surface layers), and plaques (a sticky deposits in which microbes grow), which are often seen in the middle of the oesophagus.
Habits
- Tobacco Use
- Alcohol consumption
- Opium consumption
- Consumption of hot drinks
- Consumption of carbonated soft Drinks
- Eating pickled vegetables
Nutritional Deficiencies
- Low intake of fresh fruit and vegetables
- Vitamin and mineral deficiencies
Medications
- Non-steroidal anti-inflammatory drugs
- Medications that relax lower esophageal sphincter
- H2 receptor antagonists
Infections
- Human Papillomavirus
Chemical carcinogens
- Polycyclic aromatic hydrocarbons
- Nitrosamines
- Acetaldehyde
Physiologic or pathologic predisposing conditions
- Gastroesophageal acid reflux
- Hiatal hernia
- Achalasia, gastric atrophy
- Poor oral health
Occupational exposure (to silica and asbestos)
Low socioeconomic status
Tobacco use
- Cigarette smoking is connected with esophageal squamous cell carcinoma more strongly than with esophageal adenocarcinoma.
- The risk of esophageal cancer is around three-seven times higher for current smokers
- Similar hazards are seen with cigar and pipe smoking.
- Chewing betel quid containing tobacco, which is prevalent in South and Southeast Asia, may also lead to esophageal squamous cell carcinoma.
Alcohol consumption
- In the 1970s and 1980s, researchers established alcohol as a significant cause of esophageal cancer and the interaction with cigarette smoking can double the risk.
- When used in excess (3 or more drinks per day), the risk normally rises 3-5fold.
- According to several research, only certain forms of alcohol may be connected with esophageal adenocarcinoma. For instance, one research revealed that consuming straight liquor may raise risk, whilst another suggested that drinking wine may decrease risk.
Opium use
- Although opium in its natural state is not mutagenic, smoking opium however may create carcinogenic polycyclic aromatic hydrocarbons or other chemicals.
- Opium dross (residue remaining after opium has been smoked) and smoke condensates from opium can induce mutations.
- Very high rates of opium consumption in north-eastern Iran were linked with increased prevalence of esophageal cancer
Hot foods and drinks
- Esophageal cancer has been linked to repeated thermal harm from consuming hot meals and beverages.
- Ingestion of hot beverages may significantly raise intra esophageal temperature, and this rise is dependent on the initial drinking temperature and, more critically, the size of the sip.
- Depending on the size of the sip, consuming coffee at 65 °C elevated intraesophageal temperature by 6-12°C
Consumption of carbonated soft drinks
- Carbonated soft drinks contributed to the rise in the prevalence of esophageal cancer since they are acidic and may promote reflux by generating stomach distension.
Consumption of pickled vegetables
- The consumption of pickled vegetables was considered a key risk factor for esophageal cancer in certain regions.
- A higher incidence of esophageal cancer was seen in regions with a greater consumption of pickled vegetables.
- Fungi and yeasts may produce potentially carcinogenic chemicals.
- However, epidemiologic investigations have had contradictory findings.
- In 1993, the International Agency for Research on Cancer (IARC) stated that traditional Asian pickled vegetables may be harmful to humans.
Low intake of fresh fruit and vegetables
- Low intake of fresh fruit and vegetables has long been considered as a possible risk factor for esophageal cancer.
- World Cancer Research Fund and American Institute for Cancer Research report, published in 2007 identified an inverse association of fruit intake (especially citrus fruits like lemon) and esophageal cancer.
- The final comment on vegetables was: “Non-starchy vegetables probably protect against oesophageal cancer”
- Gathering all evidence together, high intake of fruit and vegetables probably decreases oesophageal cancer risk by approximately 20% per 50 grams of fruit or vegetable intake per day.
Vitamin and mineral deficiencies
- Epidemiologists from the early 1980s, had gathered compelling evidence of vitamin and micronutrient deficiencies in the in the genesis of oesophageal cancer.
- Studies demonstrated the antioxidant effects of some vitamins could prevent tumour formation; and people in some areas with a very high risk of oesophageal cancer
- Meta-analyses demonstrated that deficiencies of selenium and zinc deficiencies may contribute to the pathogenesis of ESCC.
Non-steroidal anti-inflammatory drugs
- Meta-analysis published in 2003, concluded that non-steroidal anti-inflammatory drugs (NSAIDs) reduced risk of oesophageal cancer in a dose-response manner.
Medications that relax the lower oesophageal sphincter
- The lower oesophageal sphincter normally prevents acid reflux from the stomach into the oesophagus.
- There are few medications which help in relaxing the lower oesophageal sphincter, resulting in acid reflux and an increased risk of oesophageal cancer. They are:
- asthma treatments (-adrenergic agonists and theophylline-containing pharmaceuticals)
- calcium channel blockers
- benzodiazepines
H2 receptor antagonists
- Excessive use of H2 receptor antagonist may raise the risk of oesophageal cancer by neutralising gastric pH, which enables bacteria to thrive in the stomach and may lead to an increase in carcinogen formation (nitrosamines and acetaldehyde). However, few studies stated H2 receptor antagonists may lessen the incidence of oesophageal cancer by lowering the acidity of gastroesophageal reflux
Human papillomavirus
- Human papillomavirus (HPV) infection has been correlated with an increased incidence of squamous cell cancers of the upper oesophagus Apart from oesophageal cancer, the association of HPV (most notably HPV 16 and HPV 18 strains) is also seen in the epithelial cancers of the vulva, anus and penis.
Polycyclic aromatic hydrocarbons
- Polycyclic aromatic hydrocarbons have been carcinogens (cancer causing agents) for a long time which result from the incomplete combustion of organic substances.
- Exposure to polycyclic aromatic hydrocarbons include: Tobacco use, Consumption of charbroiled meat and other foods, Air pollution, Occupational exposure
- A causal link between polycyclic aromatic hydrocarbons or polycyclic aromatic hydrocarbons-containing substances and cancer has been established for cancers of the skin, lung, and bladder.
- Oesophageal cancer is causally connected to tobacco smoke, which includes substantial levels of polycyclic aromatic hydrocarbons.
N-Nitroso compounds
- N-nitroso compounds (NNCs) are strong carcinogens inducing oesophageal cancer, and stomach cancers. Humans may be exposed to NNCs by Cigarette smoking, Occupational exposure, Variety of dietary sources.
- Vegetables are the primary source of exogenous nitrates, although water may potentially contain large concentrations.
- Poor oral health with oral bacteria can increase N-nitroso compounds which increases the risk of oesophageal and gastric cancer.
- Consuming processed meat, a significant source of nitrites and nitrosamines, was consistently linked to an increased risk of oesophageal cancer.
Acetaldehyde
- Acetaldehyde exposure can be through various ways most notably by drinking alcohol.
- Alcohol is broken down into acetaldehyde in the body. Apart from alcohol, acetaldehyde exposure can be done by Smoking cigarettes, Eating mouldy food, Burning wood and coal, Metabolism of sugars in the body by oral and colonic bacteria.
- Lymphocytes can undergo point mutations with acetaldehyde exposure initiating cancer.
Fumonisins
- Toxins from a fungus that grows mostly on corn (Fusarium verticillioides).
- Chinese and African ecologic studies demonstrated a higher risk of oesophageal cancer with increased exposure to fumonisins.
Gastroesophageal acid reflux
- Symptomatic gastroesophageal acid reflux disease (GERD) illness is one of the most important recognised risk factors for oesophageal cancer.
- Although any reflux may raise the risk of oesophageal cancer by as much as 8-fold, very frequent and severe reflux can increase the risk by as much as 20-fold.
- Oesophageal cancer may be induced by recurrent acid reflux in the lower part of the esophagus and changing the local squamous tissue into Barrett’s oesophagus.
Obesity
- Overweight (body mass index from 25 to < 30 Kg/m2) and obesity (body mass index of 30 Kg/m2 or higher) are associated with oesophageal cancer.
- About 2–3-fold increase in oesophageal cancer risk is seen in overweight and obese individuals (slightly higher risk in obese compared with overweight people).
- Increased risk of gastroesophageal reflux and Barrett’s esophagus can be seen with intra-abdominal pressure caused by obesity.
Hiatal Hernia
- By increasing gastric acid reflux, hiatal hernia may raise oesophageal cancer risk.
- Hiatal hernia - condition where the top part of stomach bulges through an opening in the diaphragm which can happen to people of any age and any gender.
- Studies linked 2-6 times higher risk of oesophageal cancer with hiatal hernia
- Hiatal hernia can also increase the possibility of high-grade dysplasia and oesophageal cancer in individuals with Barrett’s oesophagus.
Achalasia Cardia
- Achalasia is an oesophageal motility condition marked by aperistalsis (devoid of peristaltic movement) in the distal esophagus and lack of lower oesophageal sphincter relaxation.
- This resulted in stasis and fermentation of food in the oesophagus, which may have contributed to an increase in inflammation and oesophageal cancer risk.
- A 10-fold increased oesophageal risk of cancer is seen with achalasia cardia.
- Other benign disorders that produce oesophageal blockage, such as oesophageal webs and lye stricture, have also been associated with significant increases in the incidence of EC.
Gastric atrophy
- Patients with gastric atrophy (thinning of the inner lining, gastric glands and mucosa of the stomach wall) are 3 times more likely to contract oesophageal cancer.
- As gastric glands are reduced, bacterial proliferation is increased due to reduced acid secretion is reduced.
- Increased acid production can increase the production of carcinogens such as nitrosamines and acetaldehyde.
- Nitrosamines and acetaldehyde can cause gastric cancer and oesophageal cancer.
Poor oral hygiene and tooth loss: Poor oral health could potentially be a risk factor for oesophageal cancer. The various factors through which poor oral health could cause oesophageal cancer are:
- changes in oral microbial flora leading to poor oral health with increased production of carcinogens such as nitrosamines and acetaldehyde
- physical irritation and oesophageal epithelium damage due to swallowing of unchewed food
- changes in dietary patterns and nutrient intake due to poor dentition
- infection of the oesophageal mucosa with an oral microorganism
Occupational exposure
- Although not considered an occupational cancer, the risk of oesophageal cancer is 2-16 times higher with occupational exposure to asbestos.
- Similar effect is seen with silica too.
- Crystalline silica is can also cause lung cancer and mesothelioma (cancer of mesothelial tissue)
Low socioeconomic status
- Oesophageal cancer has long been known as a disease of the poor and the socially disadvantaged.
- Approximately nine out of ten individuals with this condition belong to the lower middle class and are often financially insecure.
- Comparing people with lower socioeconomic position to those with better socioeconomic status, the majority of research have shown a 2-4-fold increase in risk.
Esophageal cancer prevention
To significantly improve the prognosis of esophageal cancer, preventative methods have been researched, developed, and are strongly advised.
Abstinence from tobacco and alcohol - Tobacco and alcohol use are the most prominent lifestyle risk factors for esophageal cancer.
- Each of these variables increases the chance of esophageal cancer, and their combination multiplies the risk even more.
- Tobacco and alcohol avoidance is one of the greatest strategies to reduce the risk of esophageal cancer.
Maintenance of diet, body weight, and physical activity - Indulgence in balanced diet is as essential as maintenance of a healthy weight.
- A diet rich in fruits and vegetables may reduce the incidence of esophageal cancer.
- Obesity has been associated with esophageal cancer, namely adenocarcinoma, therefore maintaining a healthy weight may also reduce the chance of developing this illness.
- Physical activity may help lessen the chance of developing esophageal cancer.
Testing for gastroesophageal reflux disease or Barrett’s esophagus - Treating people with gastroesophageal reflux disease may help prevent Barrett’s esophagus and esophageal cancer.
- Often, reflux is treated with changes in diet and lifestyle (for example, weight loss for overweight individuals), as well as drugs called H2 blockers or proton pump inhibitors (PPIs).
- Surgery might also be an option for treating reflux if it is not controlled with diet, lifestyle changes, and medicines.
- For patients suffering with Barrett's oesophagus, daily therapy with a proton pump inhibitor (PPI) may reduce the chance of cancer-causing cell alterations (dysplasia).
Frequently asked questions
Is esophageal cancer curable?
Yes. There are better chances of recovery from esophageal cancer if found very early, but its symptoms are noticeable usually in an advanced stage. At later stages, treatment of esophageal cancer can be palliative, but rarely can be cured. The treatment options and prognosis always depend on the:
- The stage of the cancer.
- The potentiality of tumour completely being removed by surgery.
- The patient’s general health
The body
Can MRI detect esophageal cancer?
Yes. Magnetic resonance imaging (MRI) can be utilised for diagnosing esophageal cancer. MRI has a poor specificity but a high sensitivity for identifying esophageal cancer. Nevertheless, it must be understood that MRI is contraindicated in the following patients with:
- Implanted pacemakers
- Intracranial aneurysm clips
- Cochlear implants
- Certain prosthetic devices
- Implanted drug infusion pumps
- Neurostimulators
- Bone-growth stimulators
- Certain intrauterine contraceptive devices; or
- Any other type of iron-based metal implants.
How to treat esophageal cancer?
Treatment for symptoms and adverse effects may also be included in the care plan. Some of the most typical approaches of treating esophageal cancer which include:
- Esophageal cancer surgery
- Endoscopic therapy
- Radiation therapy
- Therapies using medication
Does esophageal cancer show up in blood test?
Yes. esophageal cancer can be diagnosed through blood tests. There are various biomarkers which establish the diagnosis of esophageal cancer. They are:
- Micro-RNA
- Long non-coding RNA
- Propanoic acid
- Linoleic acid
- L-glutamine
- Antibodies against p53, NY-ESO-1 etc
- Antibodies against amino acid L-proline, ketone body 3-hydroxybutyrate etc
- Neutrophil-lymphocyte ratio
- Erythrocyte mutant frequency
Does esophageal cancer cause back pain?
Back pain is one of the symptoms of advanced esophageal cancer. It occurs if the metastasis of esophageal cancer spread into the pericardium (membrane that encloses heart) or mediastinum (membrane between lungs). The other symptoms of advanced esophageal cancer include:
- Hiccups – due to the spread of cancer into the phrenic nerves or the diaphragm.
- Chronic coughing and vocal hoarseness – due to metastasis of cancer into the laryngeal nerves.
- Bone pain and high blood calcium levels (hypercalcemia) - the metastasis of cancer into the bones.
Can CT scan detect esophageal cancer?
Yes. Computed tomography (CT or CAT) scan can be utilised to detect esophageal cancer.
- CT scan uses many x-ray views to provide an image of the body's internal structures.
- These images are then combined by a computer to create a high-resolution, three-dimensional image of the patient, revealing any tumours or other abnormalities.
- A CT scan may be performed to assess the tumour’s size.
- Before a scan, it is common practise to provide a specific dye called a contrast medium in order to improve resolution.
- In most cases, this dye is administered through intravenous injection.
- The low quantity of radiation during a CT scan poses no danger.
- Pregnants must refrain from CT scan as radiation may result in birth abnormalities.
- Patients must inform to their oncologist about their condition, especially if they are allergic or sensitive to drugs or suffering with renal disease
Can endoscopy detect esophageal cancer?
Yes. Endoscopy can detect esophageal cancer.
- The lining of esophagus examination during an upper endoscopy.
- Patient is sedated before a tiny, flexible tube called an endoscope is inserted down the mouth and into the oesophagus.
- Medication used to induce a state of calm, relaxation, or sleepiness is referred to as sedation.
- If the esophagus is obstructed, an endoscopic balloon dilation may expand the esophagus and allow food to flow through while therapy is being administered.
- The biggest disadvantages include the inability to distinguish between benign and malignant tissues based on imaging alone, leading to overstaging because to peritumour inflammation
Can esophageal ulcers turn into cancer?
While chronic irritation accompanied by long-standing infections are focussed on a localised esophageal tissue, it causes esophageal ulcers. Negligence of esophageal ulcers over time can increase the risk of esophageal cancer. Helicobacter pylori is usually the microbe which causes the infection of esophagitis.
Can metastatic esophageal cancer be cured?
No. The metastatic esophageal cancer is the advanced stage in which the curable rates are very low. In these patients only palliative therapy can be provided. Around 20% of the patients with stage 4 esophageal cancer will survive for 1-year or more after they are diagnosed.
Can ultrasound detect esophageal cancer?
Yes, ultrasound is used to detect esophageal cancer. The staging of esophageal cancer is mostly determined by computed tomography and endoscopic ultrasonography. Endoscopic ultrasonography better performs than computed tomography and is regarded as the most precise imaging technique for esophageal cancer staging. Clinical staging of esophageal cancer is essential for deciding perioperative care and treatment choices, particularly T staging.
Does eosinophilic esophagitis cause cancer?
No. Till date there haven’t been any evidence of eosinophilic esophagitis causing esophageal cancer.
- A study in 2017 analysed various cases from 1999-2014 to demonstrate that there is no significant difference or increase in the risk of contracting esophageal cancer between the normal population and patients suffering with eosinophilic esophagitis.
- Nevertheless, it must be understood that the raise of eosinophilic esophagitis incidence since the last two decades have raised concerns especially that many of its symptoms and physical features [such as dysphagia (swallowing difficulties), odynophagia (painful swallowing), heartburn, and food impaction (food stuck in esophagus) are similar to those of esophageal cancer.
How to detect esophageal cancer?
The detection of esophageal cancer can be done by the following diagnostic tests post physical examination.
- Barium swallow (oesophagram)
- Upper endoscopy
- Endoscopic ultrasound
- Bronchoscopy
- Biopsy
- Computed tomography scan
- Magnetic resonance imaging
- Positron emission tomography
The options for esophageal cancer diagnosis are extensive and must be understood that all the tests may not be utilised on everyone. When deciding which for a specific diagnostic test, the oncologist can consider:
- The type of cancer suspected
- The signs and symptoms
- The age and general health
- The results of earlier medical tests
Will a chest X-ray show esophageal cancer?
While not conclusive, the physician may prescribe for a chest X-Ray which could provide an additional value to the preliminary tests after completing physical examination.
- This may be done when the doctor may fully not suspect the manifestation of esophageal cancer in the body.
- If the suspicion of esophageal cancer manifestation is increased, the physician may then refer the patient to oncologist who may prescribe few more tests to confirm and know the stage of esophageal cancer.
- Chest x-ray is a diagnostic procedure that employs invisible electromagnetic radiation rays to make pictures of inside tissues, bones, and organs on film.
How long stage 2 esophageal cancer treatment takes?
About 18 months or longer active therapy is necessary for stage 2 breast cancer. The range of therapy vary from surgery and six weeks of radiation to a comprehensive regimen of chemotherapy, radiotherapy, and biologic treatments.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868