Hysterectomy Surgery - Procedure Indications, Side effects & Benefits
At Pace Hospitals, the state-of-the-art OT is equipped with AI robotic surgery system and world-class advanced 3D HD laser and laparoscopic equipment to perform minimally invasive major and supra-major surgery for cancerous and non-cancerous gynecological disorders.
Our team of the top laparoscopic hysterectomy surgeon and best gynecologist in Hyderabad, obstetrics and gynecology doctors are having extensive experience in performing Hysterectomy surgery by open, laparoscopic and robotic methods.
Request an appointment for Hysterectomy surgery
Hysterectomy surgery - appointment
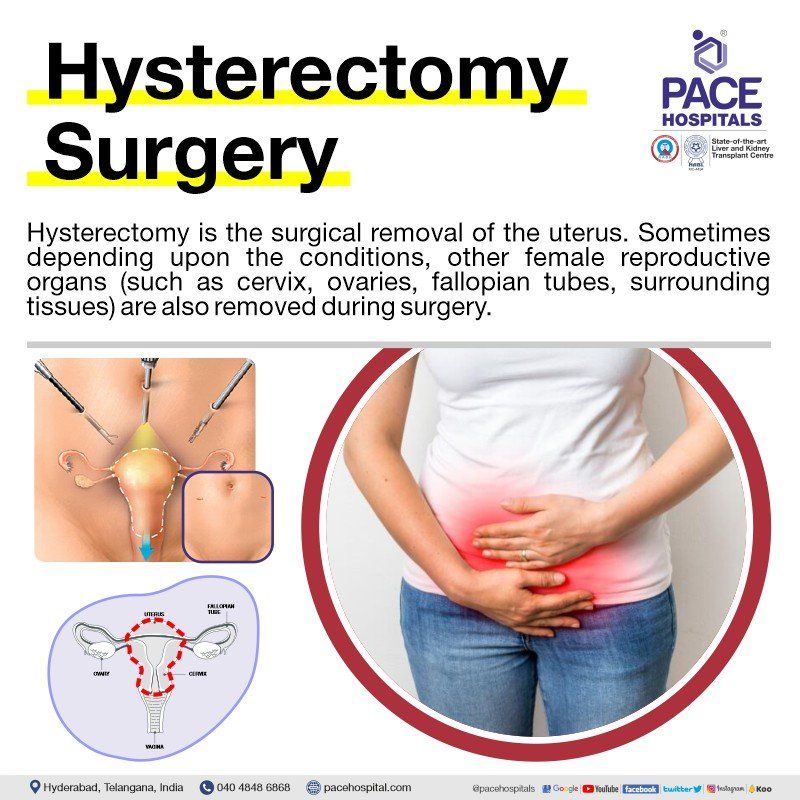
What is Hysterectomy and its purpose?
Hysterectomy meaning
Hysterectomy is the surgical removal of the uterus also called as uterus removal surgery. Sometimes depending upon the conditions, other female reproductive organs (such as ovaries, with cyst fallopian tubes, surrounding tissues) are also removed during surgery.
The benefits of hysterectomy primarily include the relief from the chronic and excruciating pelvic pain, heavy and irregular bleeding due to any underlying cause.
Hysterectomy or uterus removal surgery can also save the patient’s life if she is at an increased risk for developing uterine cancer. Recovery could be lengthy as it is major surgery, post-surgery female can't conceive the child in future. The possibility of entering menopause or experiencing menopausal symptoms after hysterectomy surgery is typically high.
What are the indications for hysterectomy surgery?
Majority of the patients are presented to the gynaecologist with overlapping symptoms. Usually, it is during the diagnosis of other indications that the presence of undetected diseases / disorders such as asymptomatic uterine fibroids are discovered.
Some of the reasons for hysterectomy, which indicates for the uterus removal, are:
- Heavy, irregular or prolonged menstrual periods refer as menorrhagia
- Increased frequency in menstrual periods that are painful (dysmenorrhea) or menstrual cramps, which do not respond to medicines or other therapies
- Presence of symptomatic uterine fibroids (non-cancerous womb growths)
- Uterine prolapse or a prolapsed womb, in which weaker ligaments (tough, flexible fibrous connective tissue connecting two bones in a joint) and muscles which cannot hold the womb resulting uterus sags or falls down into the vagina.
- Cells or tissues similar to the lining of the uterus or endometrium grows outside of uterus refer as endometriosis
- Uterus thickening and enlargement due to endometrial tissue growth into the muscular wall of the uterus, refer as adenomyosis
- Pelvic inflammatory disease (PID) that can cause infection to the female reproductive system including the fallopian tubes, ovaries, cervix, and the uterus due to sexually transmitted infections (STIs) or bacterial infection.
- Malignancy (cancer) of the vagina, cervix, uterus, fallopian tubes, or ovaries
Similarly, the contraindications for hysterectomy include:
- Benign and asymptomatic uterine fibroids
- Abnormal pelvic bleeding
- Pelvic pain and
- Interstitial cystitis (painful bladder condition)
Types of hysterectomy surgery
Based on the patients’ conditions and pathology, your primary care doctor or surgeon may suggest you which type is needed. There are mainly five types of hysterectomy surgery, comprising:
- Total hysterectomy
- Subtotal hysterectomy
- Pan hysterectomy
- Radical hysterectomy
- Ultra-radical (extensive) surgery
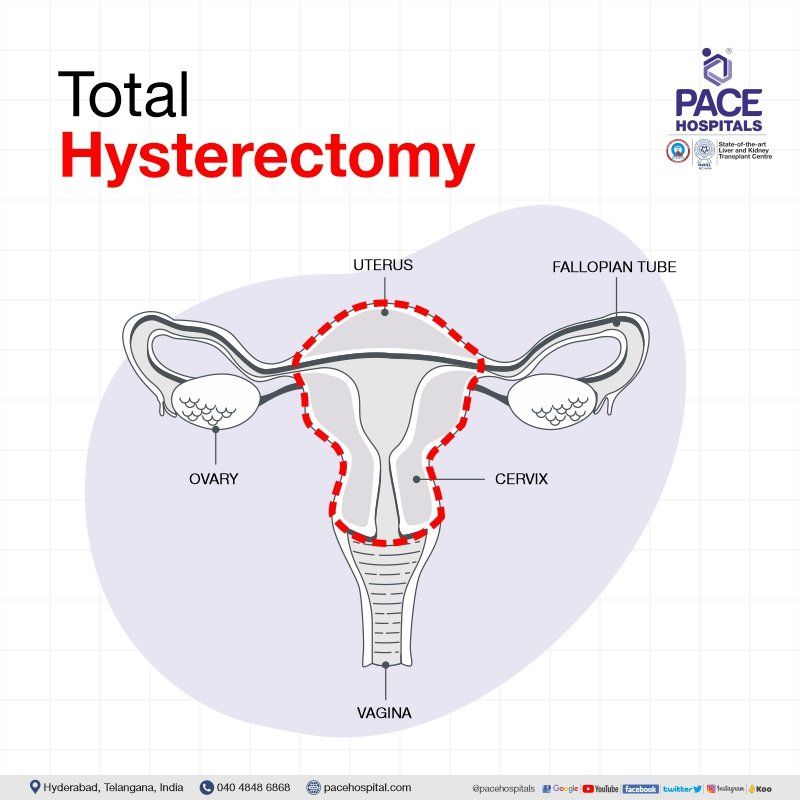
Total hysterectomy
A total hysterectomy surgery involves removing the uterus and the cervix, leaving the ovaries and fallopian tubes in place.
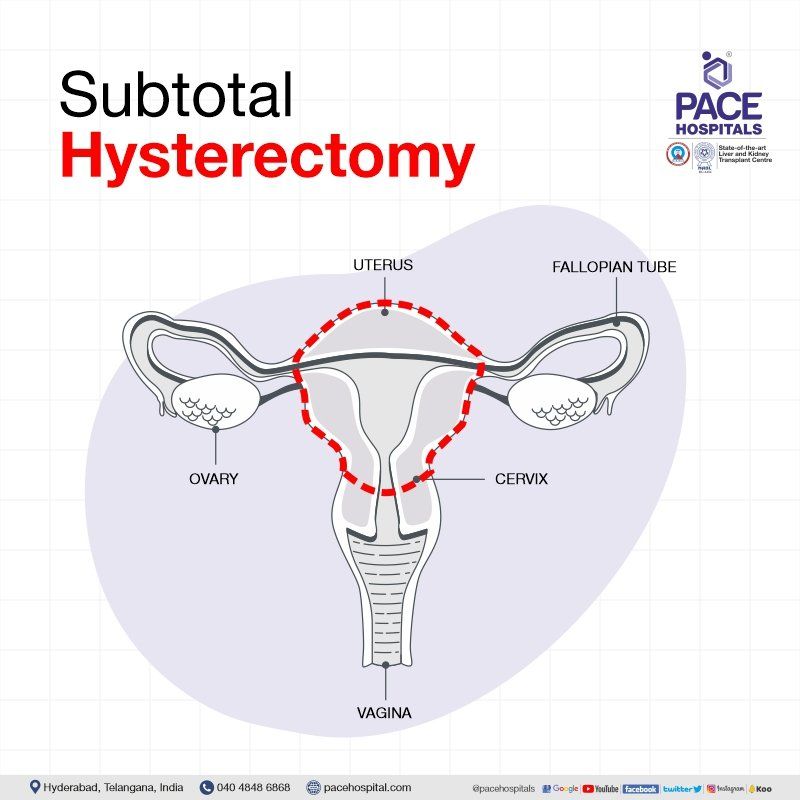
Subtotal hysterectomy / Partial hysterectomy
A subtotal hysterectomy surgery involves removing the upper part of the uterus and leaving the cervix in place. This operation is not performed commonly due to post-surgery risk of cervical cancer in and regular cervical screening (a smear test) will be needed to rule out the cancer.
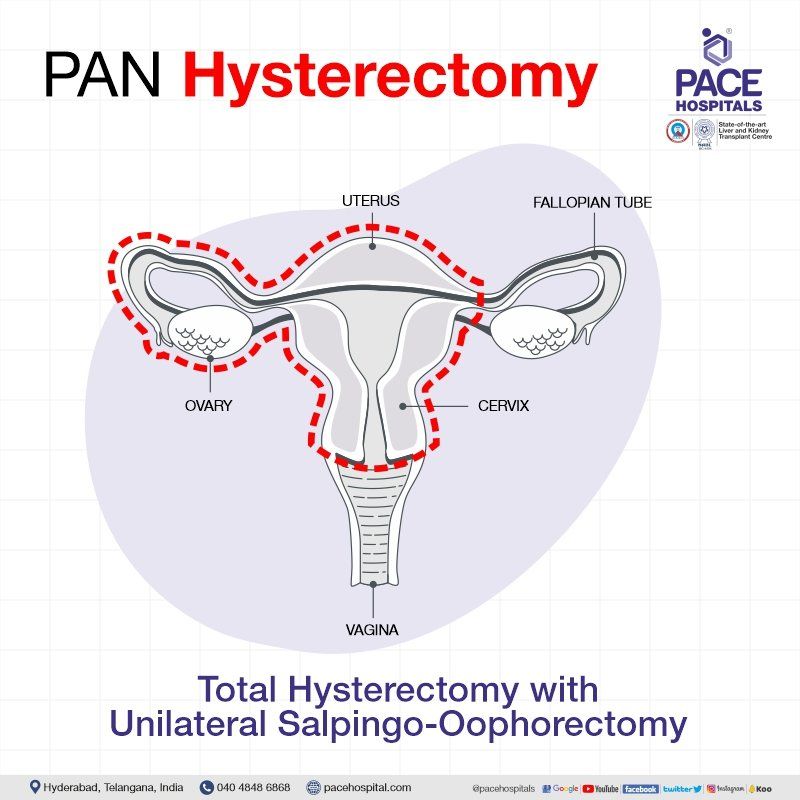
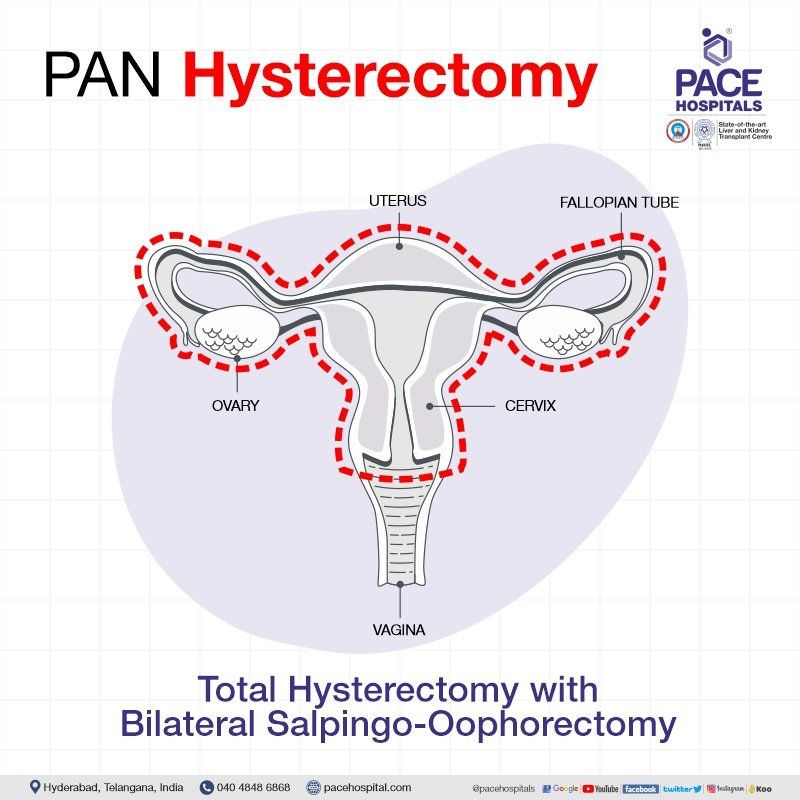
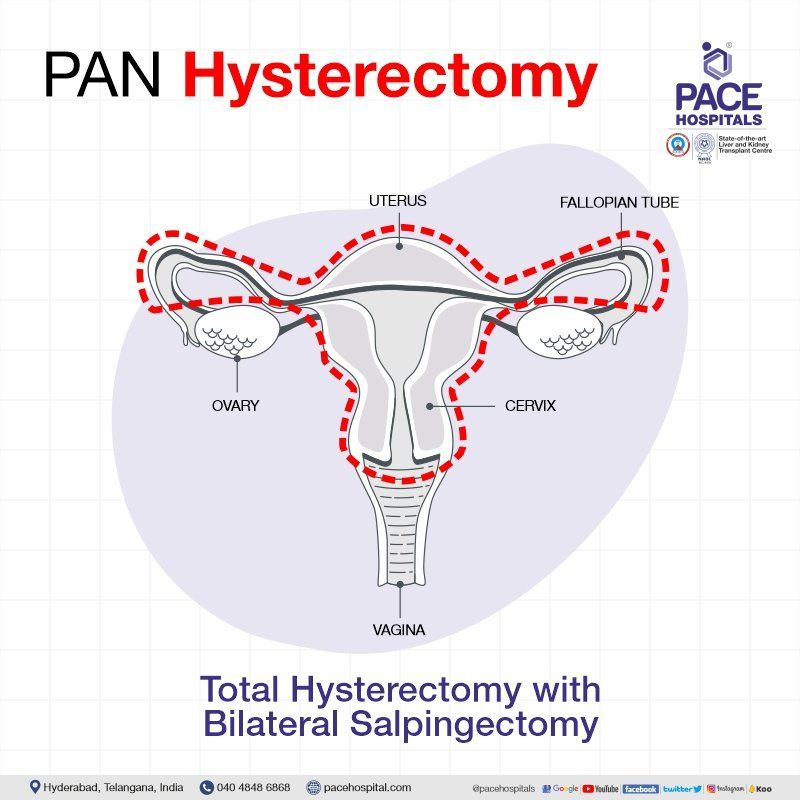
Pan hysterectomy
A pan hysterectomy surgery involves removing the uterus, the cervix, the fallopian tubes and / or the ovaries. Based on the patients’ pathology, surgeons may suggest the below type:
Total hysterectomy with salpingo-oophorectomy (TH with SO): it is of 2 types
- Total hysterectomy with unilateral salpingo-oophorectomy – the uterus, the cervix with one of the ovary and fallopian tube are removed
- Total hysterectomy with bilateral salpingo-oophorectomy - the uterus, the cervix with both ovaries and fallopian tubes are removed.
Total hysterectomy with bilateral salpingectomy – This procedure involves removing the uterus, the cervix with both fallopian tubes and leaving both ovaries in place.
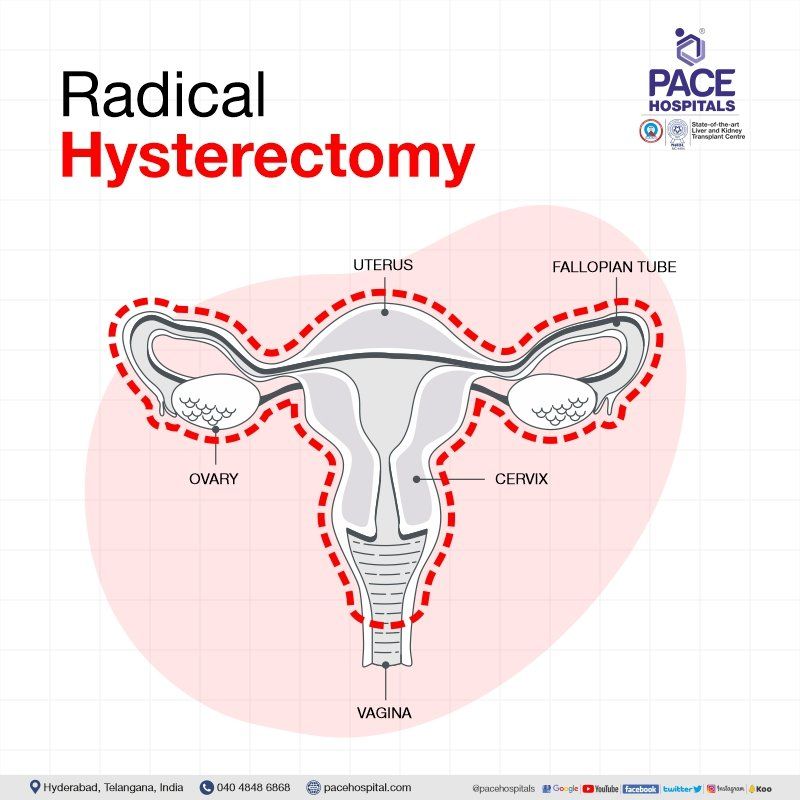
Radical hysterectomy
A radical hysterectomy surgery involves removing the whole uterus, tissue or cells on the sides of the uterus (parametrium), the cervix, pelvic lymph nodes and the top part of the vagina. This operation is mainly performed when gynecological cancer is present.
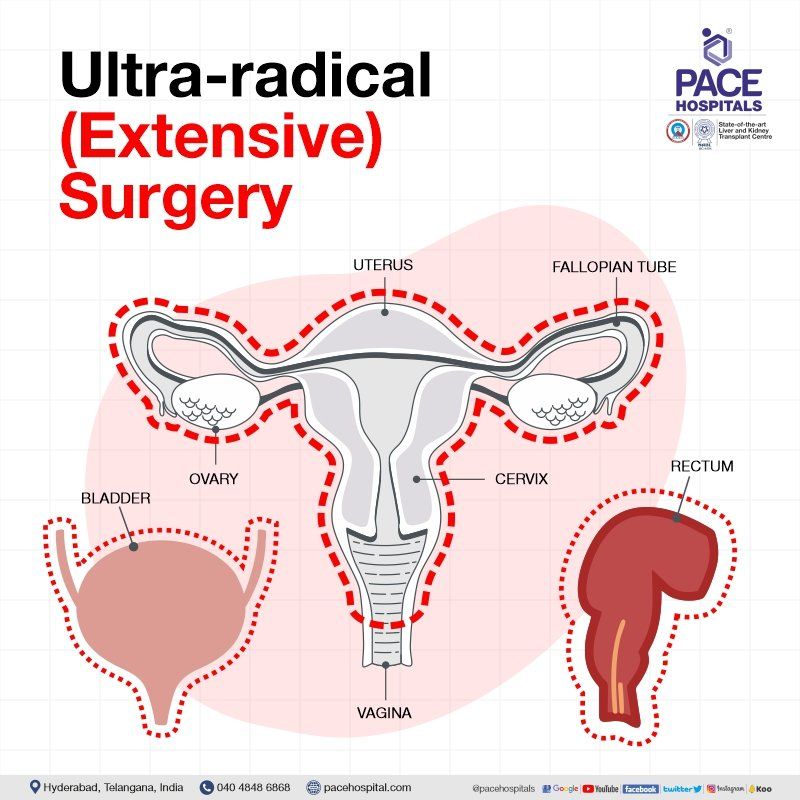
Ultra-radical (extensive) surgery
An ultra-radical (extensive) surgery involves removing the whole uterus, tissue or cells on the sides of the uterus (parametrium), the cervix, pelvic lymph nodes, the top part of the vagina with the bladder and rectum. This operation is mainly performed when gynecologic cancer are at advanced stage.
Methods of hysterectomy surgery
There are various factors which can influence the hysterectomy surgery for benign (non-cancerous) causes such as size and shape of vagina and uterus, accessibility to the uterus, extent of extrauterine disease, necessity of concurrent procedures, urgency of the case and the preference of the informed patient.
There are mainly five ways to perform hysterectomy surgery, comprising:
- Abdominal hysterectomy
- Laparoscopic hysterectomy
- Robotic hysterectomy
- Laparoscopically assisted vaginal hysterectomy (LAVH)
- Vaginal hysterectomy
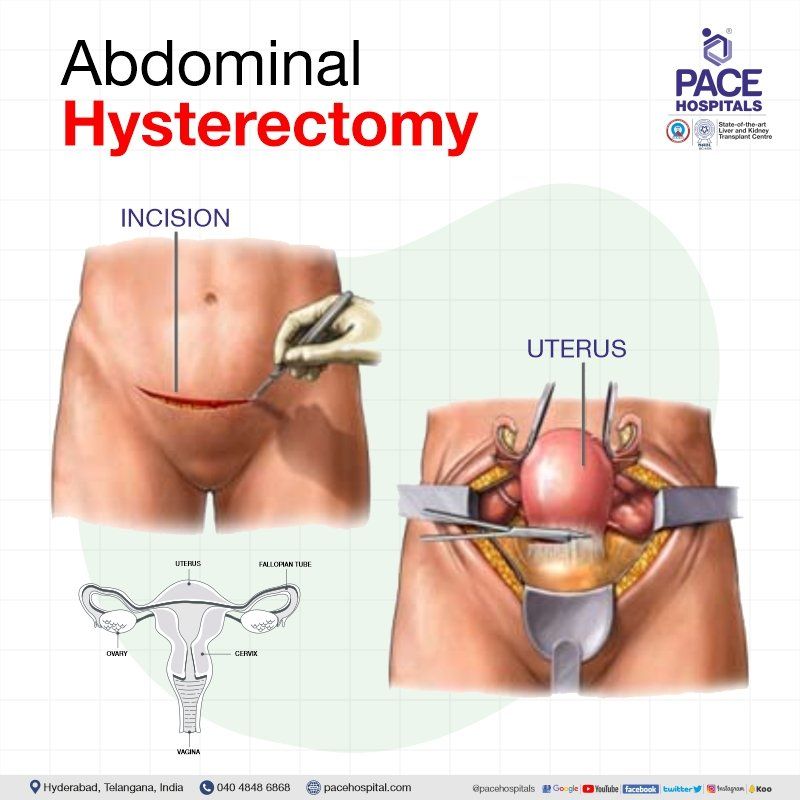
Abdominal hysterectomy
Abdominal hysterectomy also called as open hysterectomy, it is typically performed for gynaecological cancer, enlarged uterus, or when other pelvic diseases are present (such as endometriosis (occurrence of endometrial tissue outside the uterus causing pelvic pain) or adhesions). It is still the "fallback option" if other methods of hysterectomy fail.
In the open hysterectomy the surgeon create a horizontal incision along the pubic hairline resulting in a little scar for females. In case of a big uterine fibroid / cancer being the cause of a hysterectomy, the patient may require a midline incision in the lower abdomen.
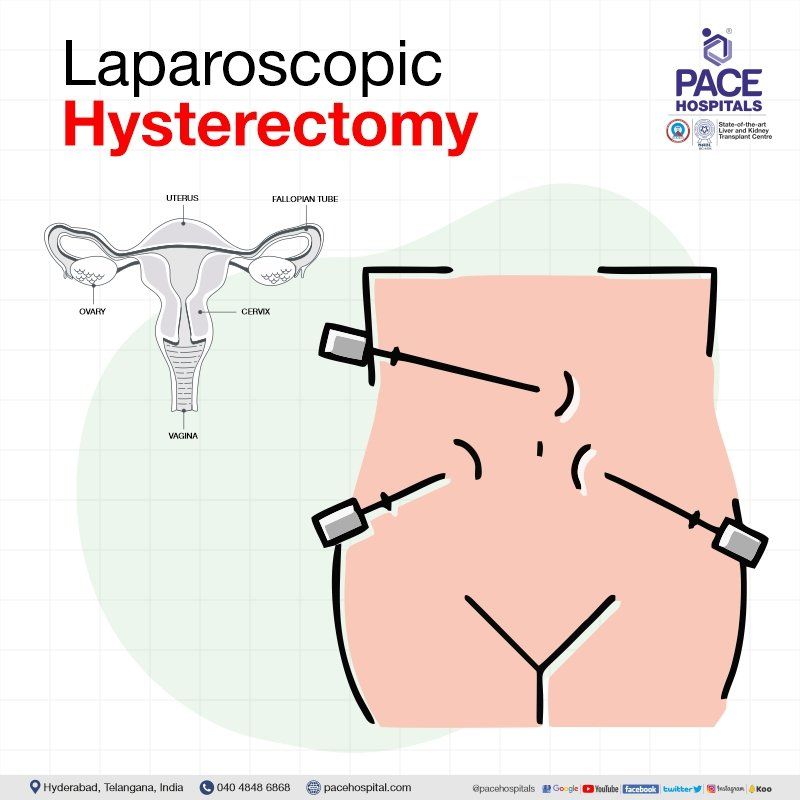
Laparoscopic hysterectomy
The whole uterus or womb (and sometimes the fallopian tubes and ovaries) is removed via four small incisions or cuts in the abdomen during laparoscopic hysterectomy, also known as "keyhole surgery."
Laparoscopic hysterectomy take longer than open hysterectomy, their advocates point to the fact that they allow for the diagnosis and treatment of additional pelvic diseases (such as endometriosis (occurrence of endometrial tissue outside the uterus causing pelvic pain)) as well as the removal of the ovaries and other adnexal (surrounding female reproductive organs and supporting tissues) structures, as well as the ability to secure thorough intraperitoneal haemostasis at the end of the procedure, and a quick recovery.
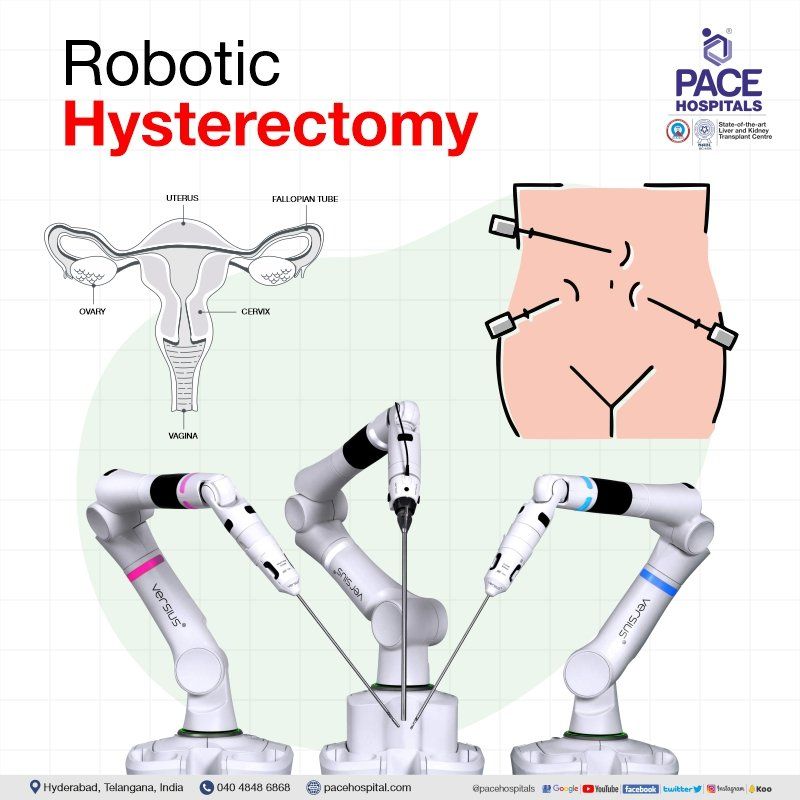
Robotic hysterectomy
In robotic assisted laparoscopic hysterectomy, a robotic console with laparoscopic hysterectomy instruments are involved, which brings more sophistication and precise manoeuvrings to the table. It is more advantageous than that of laparoscopic hysterectomy.
Depending upon the surgery either the uterus, together with the ovaries and fallopian tubes, or all of them are surgically removed through the vagina. A total laparoscopic hysterectomy is performed when the vaginal opening is sutured (sewn) using keyhole incisions. It is considered a laparoscopically assisted vaginal hysterectomy if the gynaecologist sews the vaginal opening shut using stitches placed inside the vagina.
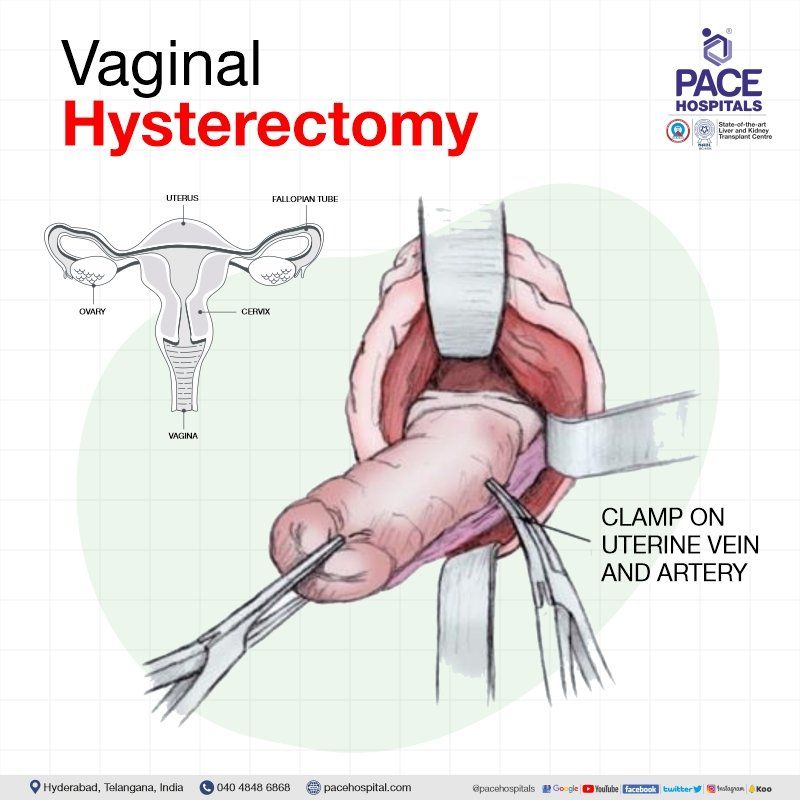
Vaginal hysterectomy
This surgery is performed through the vagina rather than an abdominal incision. When the uterus is prolapsed, it can be removed via vaginal hysterectomy, which does not leave an abdominal scar.
Most often, this procedure is used to correct uterine prolapse (occurs when pelvic floor muscles and ligaments stretch and weaken until they no longer provide enough support for the uterus resulting in the descendor protrusion beyond the vaginal canal). Even in the absence of uterine prolapse, a vaginal hysterectomy is preferred by some surgeons.
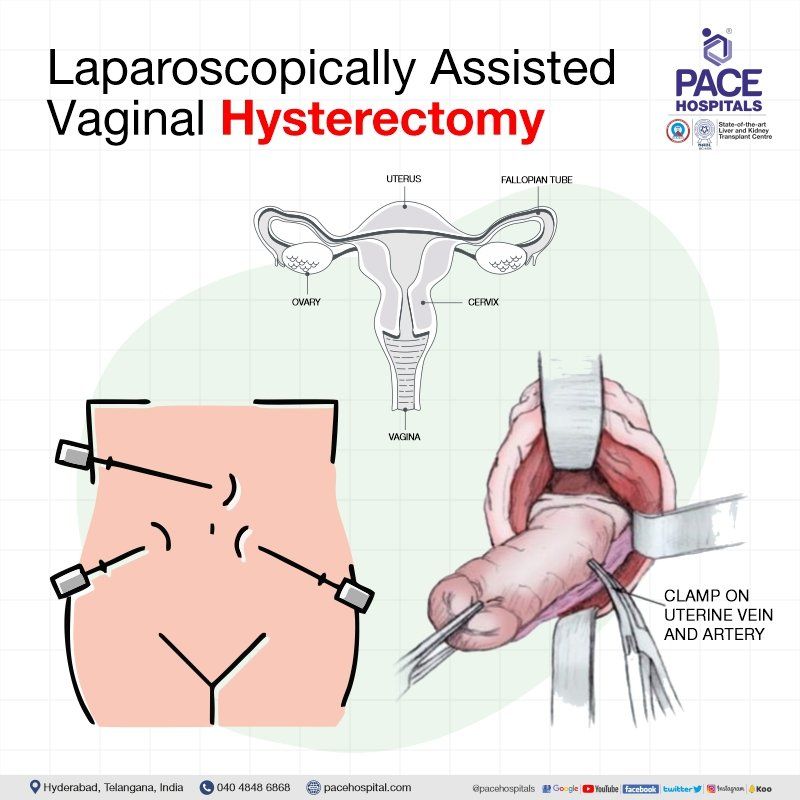
Laparoscopically assisted vaginal hysterectomy (LAVH)
Laparoscopically assisted vaginal hysterectomy is performed through both laparoscopy and vagina for removing the uterus, the cervix, the ovaries and fallopian tubes. This procedure is carried mainly in the female with uterine fibroids, endometrosis, abnromal uterine bleeding etc.
Considerations of the surgeon / gynaecologist before opting a specific hysterectomy surgery
A hysterectomy is typically not an emergency procedure but rather an “elective surgery” which deems the choice a patient makes for herself. Though there are a variety of situations in which it could be essential, it is rarely done to save a life.
Although it was suggested that the presence of technical difficulties and the risk of complications are the main obstacles to execute any procedure of hysterectomy; none of them, in an able doctor’s hands with extensive training, should hinder the implementation of the appropriate type of hysterectomy.
Prior to performing a hysterectomy procedure, the surgeon makes sure to assess each patient's unique clinical circumstances and decide which incision will best allow for the removal of the uterus while minimizing risk to the patient and maximising the likelihood of a positive outcome.
The obstetrician-gynaecologist owes it to the patient to explain the various hysterectomy techniques and to suggest the one that, in the individual case, offers the best balance of advantages and dangers.
The patient and healthcare provider should have a conversation about the relative benefits and risks of the various hysterectomy methods, keeping the patient's values and preferences in mind. Referral to a different surgeon who can perform the hysterectomy in the preferred manner may be necessary in some cases.
Preparing for the surgery
The primary care physician or gynecologist who will perform a hysterectomy surgery will discuss the operations' risks and benefits with you. Required radiology imaging and laboratory tests for the surgery are being completed at least 3 days before surgery to avoid any last-minute hassles.
After that, you'll sign a consent form for the hysterectomy operation, acknowledging that you've read and understood the procedure. Before surgery, you will be informed about what to do and what to avoid.
These are some general points that you have to follow before surgery:
- You have to stop taking few of the ongoing prescriptions before the surgery recommended by the treating surgeon, and you may be prescribed a list of new drugs.
- Inform in advance about your allergies to your surgeon.
- Lifestyle changes such as smoking/drinking might hinder your recuperation after surgery, so it is preferable to stop smoking 6 to 8 weeks before surgery.
- Usually, the patients are refrained to either eat or drink anything after midnight on the night before surgery, though this should be confirmed with the surgeon beforehand. Also, on the day of the surgery, the patient may be instructed to eat a light breakfast and lunch, followed by a clear liquid diet.
- The surgeon may ask you to either to fast the night before the surgery imaging tests. If not, enema (expelling bowel contents by injecting liquid into the rectum) may be used.
During the surgery
- It is beneficial to arrive to the hospital at least 2 hours before the surgery as the patient will be asked to change into a hospital gown and once laid down on the bed, the vitals are taken. Either the surgeon or any other healthcare personnel can be expected to explain the entire procedure to the patient, after which the patient is supposed to sign an informed consent form.
- Patients' surgical area cleaned up prior to the surgery, as it could be a hindrance and obstruct the vision of the surgeon. Moreover, it also helps in reducing the propensity of infections at the incision site.
- Any comfortable and loose-fitting clothing can be worn by the patient, but valuables such as watch, jewellery etc. are to be removed.
- An IV line (intravenous line) will be placed, through which fluids and preoperative antibiotics will be administered to prevent infection. A sedative can be prescribed, which can help calm down the patients’ nerves while reeling to the operating room.
- The patient loses consciousness, after which the surgery starts. Further, based on the patients' pathology, the surgeon may use different types of hysterectomy instruments to perform any of the following:
- Open or abdominal hysterectomy
- Laparoscopic hysterectomy
- Robotic hysterectomy
- Vaginal Hysterectomy
After hysterectomy surgery (Post-surgical Recovery)
Depending upon the surgery, the patient may be hospitalised for a few days or sent sooner. The patient can be encouraged to stand and take a brief stroll the day following hysterectomy.
- In case of abdominal hysterectomy, she should be able to leave the hospital within a few days
- In case of a vaginal hysterectomy, after 48 to 72 hours the patient can be sent home
The patient can be able to return home three to four days after a keyhole surgical procedure, but rest is necessary. The patient is encouraged to rest and refrain from moving heavy objects while recovering at home for about a period of six weeks, after which the patient can be able to drive a car or swim.
By the fifth or sixth week, she should be feeling normal. After the post-operative check-up, or six to eight weeks after being discharged from the hospital, the patient can return to work. In the second month following surgery, it is common to experience unexpected fatigue, but this passes quickly. Usually, there is no justification for weight gain following a hysterectomy.
Numbness around abdominal scars is typical. Sometimes, after a few weeks, the feeling returns, but in some women, the area is numb for a much longer time.
By the sixth week following surgery, light sexual activity can be possible and significant improvement in the mood of the patients can be observed once the unpleasant symptoms and worries about getting pregnant are lost.
- On the other hand, the opposite results can also be expected to occur. Few patients believe that the purpose of sex has been tarnished, which could lead to a psychological libido loss. At times, such thoughts can exist even after several months post-surgery.
- Nevertheless, these patients can be helped by psychosexual counselling which restore them to their former, or even better-than-ever state.
It must be understood that the ovaries do continue to produce androgen long even after menopause, and this hormone is crucial for the healthy maintenance of women's libidos.
Any woman, whatever of age, is deprived of this sexual stimulant if the ovaries are removed via a hysterectomy. However, some women report that their sex drive returns to what is typical for them after they begin testosterone therapy after the operation.
Complications of Hysterectomy Surgery
There are very little chances of both short- and long-term complications. The surgical and post surgical complications include infection, haemorrhage (internal bleeding), vaginal vault prolapse (uterine prolapse occurs when pelvic floor muscles and ligaments stretch and weaken until they no longer provide enough support for the uterus resulting in the descend or protrusion beyond the vaginal canal), and injury to the ureter, bowel, or bladder.
Infection: Minor postoperative complications are commonly caused by postoperative fever and infection. Patients who have an abdominal hysterectomy are more likely to contract an infection than those who have a vaginal hysterectomy, with the former having 6-25% range of infection rates.
Haemorrhage: One of the most dangerous after-effects of a hysterectomy is haemorrhage (internal blood loss). Around 1-3% of all hysterectomies experience complications due to excessive bleeding.
Vaginal Vault Prolapse: The sagging and falling of the vaginal vault (the top of the vagina) into the vaginal canal), when the uterus stops providing support for the vagina, the vaginal roof can sag or even fall into the vaginal canal, causing vaginal prolapse. Constipation and urine incontinence are usually accompanied by this condition.
Ureteral Injury: As the incidence of laparoscopically assisted hysterectomies has risen in the recent times, so as the ureteral damage. In laparoscopically assisted operations, this complication occurs in 0.7-1.7% of abdominal hysterectomies and in0.1% of vaginal hysterectomies.
Bowel Injury: Intestinal injury is a significant complication linked with laparoscopic-assisted abdominal hysterectomy, but uncommon in vaginal hysterectomy. The surgeon takes extra care when dealing at the areas of the rectum, ascending colon, and descending colon as these are vulnerable to damage during abdominal and vaginal procedures.
Bladder Injury: There is a risk of bladder injury in about 0.5-2% of all hysterectomies. The surgeon takes extra precautions as these bladder injuries occur during dissecting the bladder free of the lower uterine segment, cervix, and upper vagina.
Thromboembolic Disease (blood clot which dislodged from another site in the circulation resulting in blood vessel obstruction): Low-risk patients who undergo abdominal hysterectomy have a 0.2% chance of venous thromboembolism, while high-risk patients have a 2.4% risk. It is a common risk for every patient who underwent any form of surgery, let alone hysterectomy. Early ambulation after surgery and the use of graduated compression stockings can reduce the risk of developing deep venous thrombosis and pulmonary embolism (blockage in one of the pulmonary arteries in the lungs) during the perioperative period. Each patient's risk variables will determine which form of prevention is advised.
Impaired Sexual Function: Research shows that the most prevalent source of anxiety for women undergoing hysterectomy is the fear of sexual dysfunction after the operation. The possible causes of sexual dysfunction include vaginal shortening, atrophic vaginitis (vaginal dryness) owing to oestrogen insufficiency (ovaries stop functioning before age of 40 resulting in irregular production of oestrogen or eggs), and disturbance of vaginal innervation (the entire collection of nerve endings in vagina that provide sexual gratification among various other functions).
Early menopause: Changes in hormone balance cause a number of the long-term complications seen after hysterectomy, including premature menopause. While some medical healthcare professionals advocate for removing the ovaries to prevent cancer, others believe in retaining "normal ovaries" so that hormonal functions can continue without the need for long-term hormone therapy, especially in women who cannot take oestrogen due to other medical contraindications.
Psychological Effects: Loss of childbearing potential, negatively effects on a woman's self-image, social disruption due to a long recovery time, and a history of inadequate dealing with loss have all been linked to an increased risk of emotional distress after hysterectomy. The psychological outcomes of hysterectomy may be improved with early detection of ovarian failure, immediate initiation of hormone therapy in perimenopausal women and in those undergoing oophorectomy, and regular follow-up.
Myomectomy vs Hysterectomy | Difference between hysterectomy and myomectomy
While myomectomy and hysterectomy are a couple of the common procedures in the gynaecological sphere and there are various differences between them corresponding to their indications, propensity for complications, quality of life after surgeries etc. A few of them are listed below:
| Points | Myomectomy | Hysterectomy |
|---|---|---|
| Indications | Myomectomy surgery is indicated when patients have gynecological conditions such as uterine fibroids, menometrorrhagia (when menstrual bleeding occurs outside the monthly cycle or extremely heavy and/or prolonged periods) and anaemia, pelvic pain and pressure, enlarging fibroids with the possibility of malignancy (cancer), ureteral obstruction, gestational size greater than 12 weeks and inability to evaluate adnexa (gynaecological organs around the uterus, - ovaries, fallopian tubes and neighbouring connective tissues). | Hysterectomy surgery is indicated when patients have gynecological conditions such as uterine fibroids, uterine cancer, endometriosis (the tissue in the lining of the uterus, or endometrium, grows outside the uterus), uterine prolapse, adenomyosis (the protrusion of uterine lining (endometrium), through the uterine muscle wall (myometrium), and pelvic inflammatory disease. |
| Procedure | Here only the fibroids are removed leaving the uterus intact. | There are 5 types of hysterectomies and depending on the type of hysterectomy, only uterus or its adnexa can be removed. |
| Fibroid reoccurrence | Has scope of reoccurrence. | Permanent solution for uterine fibroids. |
| Usual patient type | Usually, nulliparous patients and those who wish to preserve uterus. | Usually, patients with kids and nearing menopause are the ideal types. |
| Complications | Myomectomy surgery has very few complications such as surgical wound infection (bleeding, infection, visceral damage, and thromboembolism), intraoperative blood loss depends on the size and location of uterine fibroids, very few or almost nil intraoperative visceral injuries and unusually high incidence of fever occurring in the first 48 hours postoperatively. | Hysterectomy surgery has recorded few complications such as Surgical wound infection (Injury to the bowel, bladder, ureter, or major blood vessel), Excessive bleeding, A number of intraoperative visceral injuries, Urinary tract infection, Nerve damage, Postoperative thromboembolism, Atelectasis (partial collapse or incomplete inflation of the lung), Early onset of menopause and Loss of ovarian function. |
| Effect on menopause | Usually myomectomy doesn’t effect on menopause as the ovaries which regulates the female hormones are left intact. | Depending upon the type of hysterectomy, either the retention or excision of one or both the ovaries can be seen due to which menopause can be seen around 5 years after the surgery. This type of menopause is also called surgical menopause. |
Explore the Total Hysterectomy cost as per the types and methods
How much does a laparoscopic hysterectomy cost in India?
The average cost of laparoscopic hysterectomy in India is approximately Rs. 1,12,000 (one lakh twelve thousand only). However, cost of laparoscopic hysterectomy surgery in India may vary depending upon the different hospitals in different cities.
A laparoscopic hysterectomy cost in Hyderabad ranges vary from Rs. 90,000 to Rs. 1,20,000 (ninety thousand to one lakh twenty thousand). However, cost of laparoscopic hysterectomy surgery depends upon the multiple factors such as type of surgery, selection of room for hospital stay and corporate, Central Government Health Scheme (CGHS), ESI, Employee And Journalist Health Scheme by Telangana State Government, EHS or insurance approval for cashless facility.
How much does a robotic hysterectomy cost in India?
The average cost of robotic hysterectomy in India is approximately Rs. 2,65,000 (two lakh sixty-five thousand only). However, cost of robotic hysterectomy surgery in India may vary depending upon the different hospitals in different cities.
A robotic hysterectomy cost in Hyderabad ranges vary from Rs. 2,45,000 to Rs. 3,25,000 (two lakh forty-five thousand to three lakh twenty-five thousand). However, cost of robotic hysterectomy surgery depends upon the multiple factors such as patients age and health condition, room selection for hospital stay, Central Government Health Scheme (CGHS), ESI, EHF - Telangana State Government, EHS - Employees Health Scheme or insurance, corporate approval for cashless facility.
How much does a radical hysterectomy cost in India?
The average cost of radical hysterectomy in India is approximately Rs. 2,25,000 (two lakh sixty-five thousand only). However, cost of robotic hysterectomy surgery in India may vary depending upon the different hospitals in different cities.
A radical hysterectomy cost in Hyderabad ranges vary from Rs. 2,15,000 to Rs. 2,55,000 (two lakh fifteen lakh a thousand to two lakh fifty-five thousand). However, cost of robotic hysterectomy surgery depends upon the multiple factors such as patient's age and health condition, stage of the cancer, room selection for hospital stay, Central Government Health Scheme (CGHS), ESI, EHF - Telangana State Government, EHS - Employees Health Scheme or insurance, corporate approval for cashless facility.
How much does abdominal hysterectomy cost in India?
The average cost of abdominal hysterectomy in India is approximately Rs. 65,000 (sixty-five thousand only). However, cost of abdominal hysterectomy surgery in India may vary depending upon the different hospitals in different cities.
Abdominal hysterectomy cost in Hyderabad ranges vary from Rs. 55,000 to Rs. 85,000 (fifty-five thousand to eighty-five thousand). However, cost of abdominal hysterectomy surgery depends upon the multiple factors such as patients age and health condition, room selection for hospital stay, Central Government Health Scheme (CGHS), ESI, EHF - Telangana State Government, EHS - Employees Health Scheme or insurance, corporate approval for cashless facility.
How much does a vaginal hysterectomy cost in India?
The average cost of vaginal hysterectomy in India is approximately Rs. 72,000 (seventy-two thousand only). However, cost of vaginal hysterectomy surgery in India may vary depending upon the different hospitals in different cities. Whereas the average cost of laparoscopic assisted vaginal hysterectomy in India is approximately Rs. 1,18,000 (one lakh eighteen thousand only).
A vaginal hysterectomy cost in Hyderabad ranges vary from Rs. 65,000 to Rs. 92,000 (sixty-five thousand to ninety-two thousand) whereas LAVH - the laparoscopic assisted vaginal hysterectomy cost in Hyderabad ranges vary from Rs. 98,000 to Rs. 1,20,000 (ninety-eight thousand to one lakh twenty-two thousand).
However, cost of vaginal hysterectomy surgery and LAVH depends upon the multiple factors such as patients age and health condition, room selection for hospital stay, Central Government Health Scheme (CGHS), ESI, EHF - Telangana State Government, EHS - Employees Health Scheme or insurance, corporate approval for cashless facility.
How much does total hysterectomy with bilateral salpingo-oophorectomy cost in India?
The average cost of total hysterectomy with bilateral salpingo oophorectomy in India is approximately Rs. 1,28,000 (one lakh twenty eight thousand only). However, cost of total hysterectomy and oophorectomy surgery in india may vary depending upon the different hospitals in different cities.
Total hysterectomy with bilateral salpingo oophorectomy cost in Hyderabad ranges vary from Rs. 1,18,000 to Rs. 1,35,000 (one lakh eighteen thousand to one lakh thirty five thousand). However, cost of total hysterectomy and oophorectomy surgery depends upon the multiple factors such as patients age and health condition, room selection for hospital stay, length of stay, CGHS, ESI, EHF, EHS - Employees Health Scheme or insurance, corporate approval for cashless facility.
How much does a supracervical hysterectomy cost in India?
The average cost of supracervical hysterectomy in India is approximately Rs. 1,15,000 (one lakh fifteen thousand only). However, cost of supracervical or partial hysterectomy surgery in India may vary depending upon the different hospitals in different cities.
A supracervical hysterectomy cost in Hyderabad ranges vary from Rs. 1,10,000 to Rs. 1,65,000 (one lakh ten thousand to one lakh sixty-five thousand). However, cost of partial hysterectomy or supracervical hysterectomy surgery depends upon the multiple factors such as patient's age and health condition, room selection for hospital stay, Central Government Health Scheme (CGHS), ESI, EHF - Telangana State Government, EHS - Employees Health Scheme or insurance, corporate approval for cashless facility.
Frequently asked questions: