Necrotizing Pancreatitis: Causes, Symptoms, complications, Diagnosis & Treatment
PACE Hospitals
Overview | Prevalence | Symptoms | Causes | Risk Factors | Complications | Diagnosis | Treatment | Prevention | FAQs | When to consult a Doctor
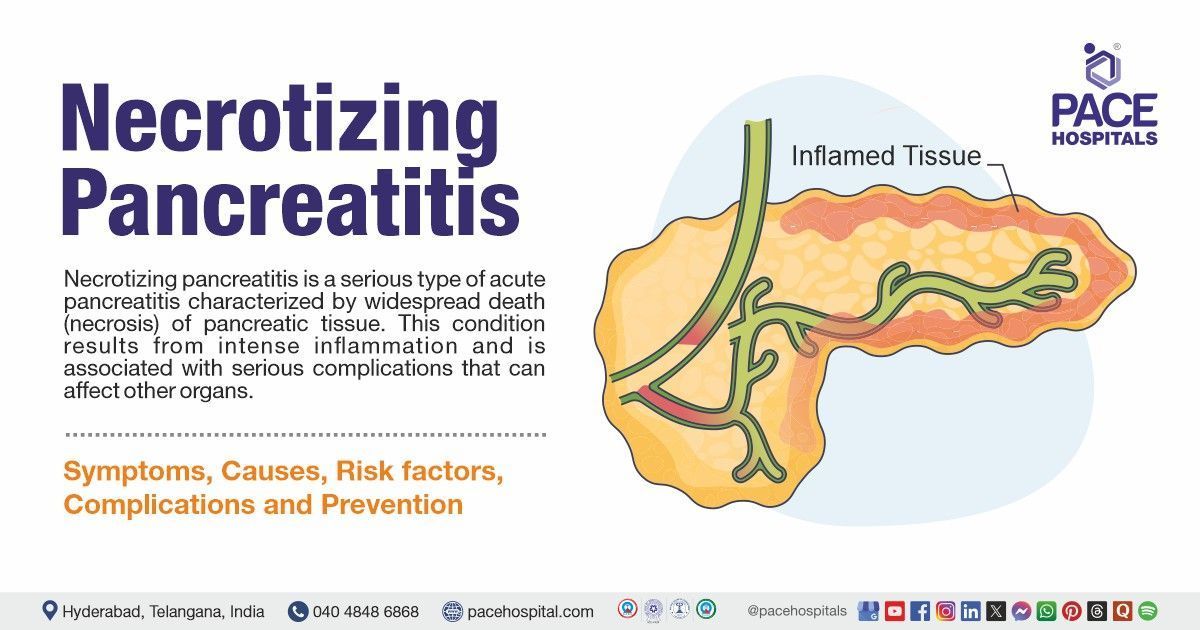
Necrotizing Pancreatitis Definition
Acute necrotizing pancreatitis is a serious type of acute pancreatitis characterized by widespread death (necrosis) of pancreatic tissue. This condition results from intense inflammation and is associated with serious complications that can affect other organs.
Pancreatic necrosis frequently necessitates intensive care and can result in lasting damage to the pancreas, as well as other severe complications, including organ failure.
Necrotizing Pancreatitis Meaning
- Necrotizing: Refers to the death of tissue as a result of severe inflammation. In necrotizing pancreatitis, parts of the pancreas undergo necrosis (tissue death).
- Pancreatitis: Inflammation of the pancreas.
Necrotizing pancreatitis typically develops when acute pancreatitis becomes severe and causes irreversible damage to the pancreatic tissue.
Prevalence of Necrotizing Pancreatitis
According to most medical sources, the global prevalence of necrotizing pancreatitis is estimated to affect around 20% of acute pancreatitis cases. For every 100 cases of acute pancreatitis, roughly 20 individuals will develop necrotizing pancreatitis.
Necrotizing pancreatitis has a significantly higher mortality rate than mild pancreatitis.
According to available data, the prevalence of necrotizing pancreatitis in India is estimated to be between 2.5% and 22.5% of acute pancreatitis cases in children, which is considered relatively high compared to Western countries; this translates to a range of 2.6-3.2 cases per 100,000 people in India overall.
This condition is diagnosed when more than 30% of the Pancreas is affected by necrosis, accounting for approximately 5% to 10% of pancreatitis cases.
Necrotizing Pancreatitis Symptoms
Acute necrotizing pancreatitis symptoms typically manifest suddenly and can escalate quickly. They include:
- Severe Abdominal Pain: Sharp, persistent pain in the upper abdomen is a hallmark symptom that radiates to the back and may worsen after eating.
- Shortness of Breath: If the disease advances to the point of organ failure, it may result in respiratory difficulties.
- Fever: Due to the inflammation and potential infection, fever often accompanies necrotizing pancreatitis.
- Tachycardia (Rapid Heart Rate): This can occur as a response to the body's systemic inflammatory response.
- Hypotension: Low blood pressure can result from systemic inflammation or sepsis.
- Jaundice: Yellowing of the skin and eyes may occur if the inflammation obstructs the bile ducts.
- Nausea and Vomiting: These symptoms are common due to the digestive system's inability to function normally.
Necrotizing Pancreatitis Causes
The acute necrotizing pancreatitis causes are similar to those of acute pancreatitis, but the inflammation severity in necrotizing pancreatitis is much greater. Key causes include:
- Excessive Alcohol Consumption: Heavy drinking can trigger acute pancreatitis and is a frequent cause of necrotizing pancreatitis.
- Hyperlipidemia: Elevated triglyceride levels can also lead to acute pancreatitis, which can develop into necrotizing pancreatitis.
- Gallstones: Gallstones are a major risk factor for acute pancreatitis, as they block the pancreatic duct, leading to inflammation and necrosis.
- Trauma or Surgery: Abdominal trauma or post-surgical complications can lead to acute pancreatitis and the progression of necrotizing pancreatitis.
- Infections: Infections, including hepatitis, mumps, and certain bacterial infections, can trigger acute pancreatitis, potentially leading to necrosis.
- Medications: Some drugs can cause pancreatitis as a side effect, potentially leading to necrosis.
- Genetic Factors: Certain genetic mutations and conditions (e.g., cystic fibrosis, hereditary pancreatitis) may predispose individuals to pancreatitis that can evolve into necrotizing pancreatitis.
Necrotizing Pancreatitis Risk Factors
There are several factors that can increase the likelihood of developing necrotizing pancreatitis, including:
- Gallstones: Individuals with gallstones or those who have had gallbladder disease are more likely to experience necrotizing pancreatitis.
- Age: Older individuals may be at greater risk due to a reduced ability to recover from the inflammation.
- Chronic Alcohol Use: Those who regularly drink excessive alcohol are at increased risk for pancreatitis and its complications.
- Obesity: Being overweight or obese increases the risk of developing acute pancreatitis, which may develop into necrotizing pancreatitis.
- High Triglyceride Levels: Elevated levels of fat in the blood can contribute to pancreatitis, making necrotizing pancreatitis more likely.
Necrotizing Pancreatitis Complications
Necrotizing pancreatitis can result in various complications, some of which can be life-threatening:
- Sepsis: Infection of the necrotic pancreatic tissue can lead to sepsis, a systemic infection that can affect multiple organs.
- Organ Failure: Severe cases of necrotizing pancreatitis can lead to failure of the heart, lungs, liver, or kidneys, requiring intensive medical support.
- Pancreatic Abscess: An infected collection of pus that may form in the pancreas and cause further complications.
- Pseudocysts: Fluid-filled sacs that form in the pancreas, which may lead to infection, bleeding, or rupture.
- Pancreatic Insufficiency: Long-term damage to the pancreas may impair its ability to produce digestive enzymes, leading to malabsorption and weight loss.
Necrotizing Pancreatitis Diagnosis
Diagnosing necrotizing pancreatitis involves a combination of clinical evaluation and diagnostic tests:
- Clinical Examination
- Physical exam
- Medical history
- Blood Tests
- Pancreatic Enzyme Levels
- Liver Function Tests (LFTs)
Necrotizing Pancreatitis Treatment
Pancreatic necrosis treatment primarily focuses on supportive care and managing complications:
- Conservative treatment
- Pain Management
- Nutritional Support
- Antibiotics
- Hospitalization
- Fluid Resuscitation
- Iv fluids
- Surgical Intervention
- Drainage and debridement
- Percutaneous drainage
- Endoscopic debridement
- Video-assisted retroperitoneal debridement (VARD).
- Open surgery (necrosectomy)

Prevention of Necrotizing Pancreatitis
Preventive measures can reduce the risk of necrotizing pancreatitis and protect the pancreas from damage, including:
- Limiting Alcohol Consumption: Overconsumption of alcohol is a major risk factor for acute pancreatitis, so reducing or eliminating alcohol intake can significantly lower the chances of developing the condition.
- Regular Checkups for Gallstones: Early treatment or removal of gallstones can help prevent gallstone-induced pancreatitis.
- Addressing underlying Conditions: Addressing conditions such as gallstones, obesity or high blood pressure (Hypertension) that affect the pancreas or bile ducts can reduce the risk of pancreatitis.
- Managing Triglyceride Levels: Maintaining blood lipids within a healthy range is essential for preventing triglyceride-induced pancreatitis.
Why Choose PACE Hospitals?
Expert Super Specialist Doctors
Advanced Diagnostics & Treatment
Affordable & Transparent Care
24x7 Emergency & ICU Support
Frequently Asked Questions (FAQs) on Necrotizing Pancreatitis
Can necrotizing pancreatitis be cured?
Necrotizing pancreatitis is not a condition that can be cured, but with proper treatment, complications can be managed, and recovery can be supported.
How is necrotizing pancreatitis treated?
Treatment involves supportive care, including pain management, fluid resuscitation, nutritional support, and antibiotics. In severe cases, surgical interventions may be required to remove necrotic tissue.
Is necrotizing pancreatitis hereditary?
Necrotizing pancreatitis is generally not hereditary, but genetic factors may predispose individuals to develop pancreatitis, which could progress to necrosis.
What lifestyle changes can prevent necrotizing pancreatitis?
Avoiding excessive alcohol consumption, maintaining a healthy weight, eating a balanced diet, and controlling triglyceride levels are key preventive measures.
What are the risks of necrotizing pancreatitis?
The risks include severe complications like organ failure, sepsis, pancreatic abscess, and permanent damage to the pancreas, including pancreatic insufficiency.
How is necrotizing pancreatitis diagnosed?
Necrotizing pancreatitis is diagnosed through imaging tests like CT scans and MRIs, blood tests to check enzyme levels, and a thorough medical history review.
Can necrotizing pancreatitis lead to pancreatic cancer?
Chronic inflammation in the pancreas can increase the risk of developing pancreatic cancer over time.
When to consult a doctor for Necrotizing Pancreatitis treatment?
Consult a doctor immediately if you suspect Necrotizing Pancreatitis (NP), as it is a serious and potentially life-threatening complication of acute pancreatitis. In this condition, parts of the pancreas become inflamed and start to die due to reduced blood supply, infection, or severe tissue damage. Without urgent medical care, it can lead to organ failure, sepsis, and even death.
Key warning signs include:
- Severe, persistent abdominal pain (often radiating to the back)
- Nausea, vomiting, and inability to eat
- High fever, chills, or signs of infection
- Swelling or tenderness in the abdomen
- Rapid heart rate, low blood pressure, or difficulty breathing (severe cases)
If these symptoms are present, a gastroenterologist or a necrotizing pancreatitis specialist can confirm the diagnosis using blood tests, CT scans, or MRI to assess the extent of pancreatic necrosis.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles