Prostatitis - Types, Causes, Symptoms, Risk Factors, Treatment, Prevention
PACE Hospitals
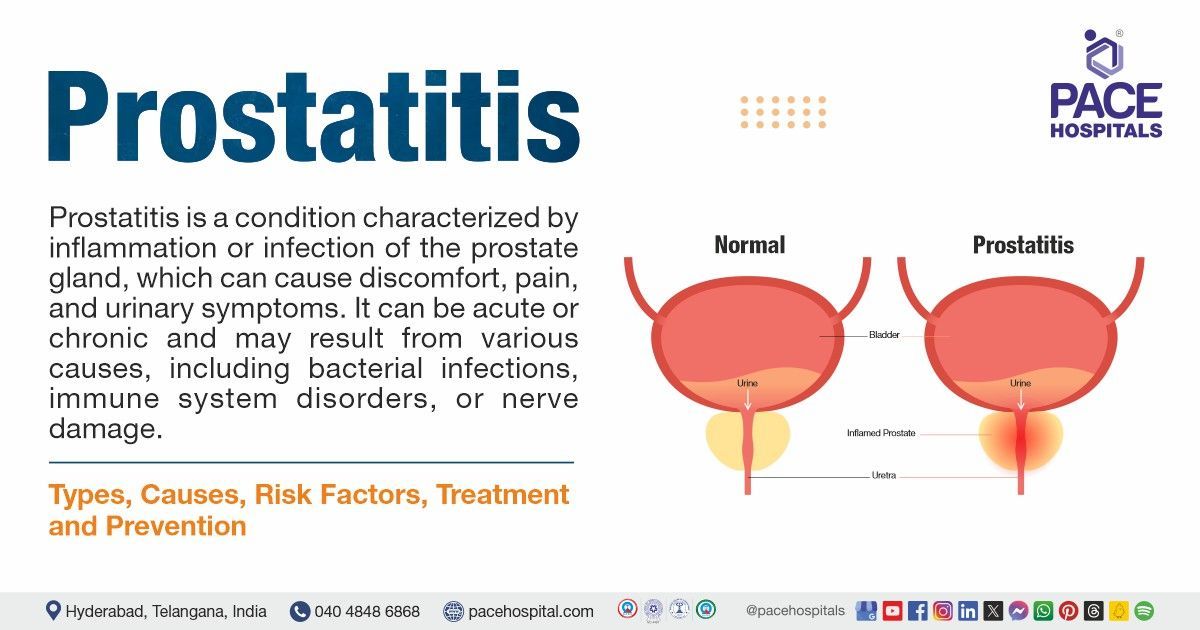
Prostatitis definition
Prostatitis is inflammation of the prostate gland and, in some cases, the surrounding tissue near the prostate gland. It's not a malignancy (cancer).
Prostatitis meaning
The term "prostatitis" is derived from the ancient Greek, which relates to an inflammatory condition. The prefix "prost-" denotes that the pathology affects the prostate gland. The word was first used in English in the 1840s, based on a French lexical item and the suffix "-itis" means inflammation.
Prostate meaning
The term "prostate" is derived from the Greek language which means "one who stands before," which characterizes the prostate gland's position. The prostate "stands before" the bladder when viewed from below, where the urethra exits the prostate gland.
What is prostate?
The prostate is a gland found underneath the bladder and adjacent to the rectum in people who are assigned male at birth (AMAB). It surrounds the urethra, which is a tube that transports urine from the bladder and through the penis. The prostate produces the fluid portion of semen.
The normal size of a prostate resembles the size of a walnut and is typically weighs around thirty grams, measuring four centimeters wide, three centimeters high, and two centimeters thick.
Prostate gland function
The primary function of the prostate gland is to produce a fluid, which, along with sperm cells from the testicles and fluids from other glands, forms semen. The prostate muscles also ensures that the semen is transported into the urethra before being ejected externally during ejaculation
Prevalence of prostatitis
Prevalence of prostatitis worldwide
According to research, the global prevalence of prostatitis among adult males is between 2% and 10%. This indicates that prostatitis is a global health concern.
The lifetime prevalence of prostatitis symptoms is 14.2%, and the chance of developing prostatitis increased with age. Men aged 40-49 are 1.7 times more likely to develop prostatitis than men aged 20-39, while men aged 50-59 are 3.1 times more likely to develop prostate inflammation. The incidence of prostatitis was 37.8 per 10,000 men.
Prostatitis symptoms may raise a man's chance of developing benign prostatic hypertrophy (enlarged prostate), lower urinary tract symptoms, and prostate cancer.

Types of prostatitis
Prostatitis is an uncomfortable condition that causes inflammation of the prostate and its surrounding tissues. Prostatitis is classified into different types, which include:
Chronic prostatitis (chronic pelvic pain syndrome)
This is the most frequent form of prostatitis. Symptoms may improve and then return without warning. Urologists do not understand why this occurs. There is no cure, but symptoms can be controlled.
Acute bacterial prostatitis
This is the least common form of prostatitis. It occurs at any age. It usually develops abruptly and creates significant symptoms. It's critical to get medical care straight away. Patients may find it difficult and painful to urinate. Other symptoms include fever, chills, lower back discomfort, genital pain, frequent urination, a burning sensation when urinating, or urine urgency at night. Patients may also experience aches and pains throughout the body.
Chronic bacterial prostatitis
This type is unusual and recurring infection that is difficult to treat. Symptoms are similar to a moderate case of acute bacterial prostatitis. However, they last much longer.
Asymptomatic inflammatory prostatitis
This is prostatitis without symptoms. The urologist will most likely diagnose it during a checkup or test such as a prostate biopsy for another health issue. They may identify it if they find infection-fighting cells in the prostatic fluid or Semen.
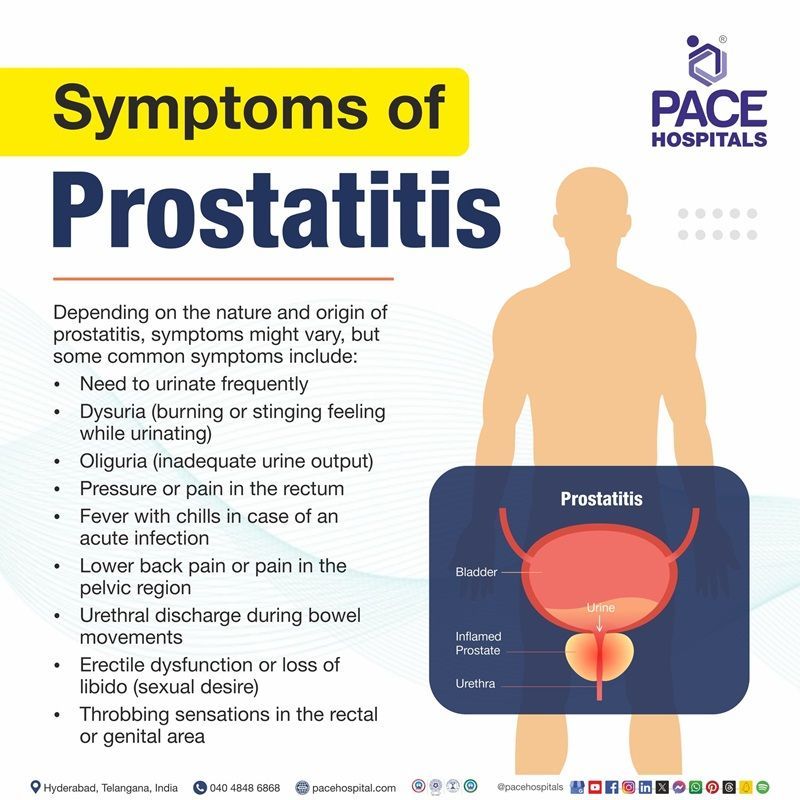
Prostatitis symptoms
Depending on the nature and origin of prostatitis, symptoms might vary, but some common symptoms include:
- Need to urinate frequently
- Dysuria (burning or stinging feeling while urinating)
- Oliguria (inadequate urine output)
- Pressure or pain in the rectum
- Fever with chills in case of an acute infection
- Lower back pain or pain in the pelvic region
- Urethral discharge during bowel movements
- Erectile dysfunction or loss of libido (sexual desire)
- Throbbing sensations in the rectal or genital area
The symptoms of prostatitis may look like other health conditions or problems. Always consult a urologist for a diagnosis.
Prostatitis causes
The causes of prostatitis vary depending on the type. Sometimes it's obvious that a bacterial infection is the offender, while in other cases the cause is unknown. Common causes of prostatitis include:
- Bacterial infections: Bacteria like Escherichia coli and Enterococcus frequently cause acute bacterial prostatitis. These bacteria can enter the body via the urethra or through medical procedures such as transrectal prostate biopsies.
- Urinary tract issues: Urinary stasis, distal urethral stricture, and benign prostatic hyperplasia are among the conditions that might lead to ascending infections and thereby raise the risk of prostatitis.
- Immune system dysfunction: Chronic prostatitis can result from immune system disorders, in which the body's immunological reaction may lead to inflammation of the prostate.
- Nervous system dysfunction: Prostatitis can also develop due to neural system dysfunction, especially when persistent pelvic pain syndrome is present.
- Lifestyle factors: Risk factors include lifestyle factors such as unprotected sexual intercourse, use of indwelling urethral catheters, and urinary tract instrumentation.
- Psychological stress and hormonal imbalances: Prostatitis has been related to both abnormal hormone activity and psychological stress.
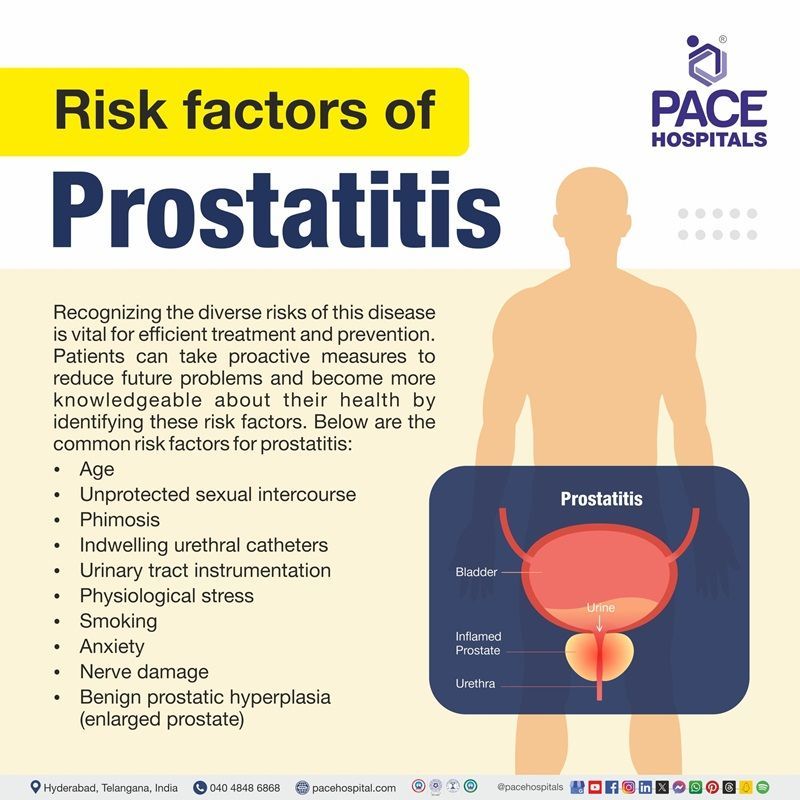
Prostatitis risk factors
Recognizing the diverse risks of this disease is vital for efficient treatment and prevention. Patients can take proactive measures to reduce future problems and become more knowledgeable about their health by identifying these risk factors. Below are the common risk factors for prostatitis:
- Age: In men under fifty years of age, prostatitis is the most prevalent urinary tract issue.
- Unprotected sexual intercourse: Following unprotected sexual practices may introduce bacteria into the urinary tract, which may eventually lead to inflammation of the prostate gland.
- Phimosis: According to a study, males who have longer foreskins or foreskins that completely enclose their glans penis are more likely to acquire chronic prostatitis.
- Indwelling urethral catheters: Using urinary catheters may allow bacteria to enter the urinary tract, leading to bacterial prostatitis.
- Urinary tract instrumentation: Urinary tract instrumentation can pose a risk for bacterial prostatitis.
- Physiological stress: Psychological stress may also increase a man’s chances of developing the condition.
- Smoking: A research study of males who underwent prostate biopsies discovered that smokers were more likely to experience acute inflammation than non-smokers.
- Anxiety: When men are anxious, the body produces a hormone called cortisol, which can trigger inflammation in the prostate gland. This inflammation can exacerbate prostatitis symptoms, such as pain and discomfort while urinating.
- Nerve damage: Chronic prostatitis/chronic pelvic pain syndrome may be more common in men who have had surgery or trauma that damages nerves in the lower urinary tract.
- Benign prostatic hyperplasia (enlarged prostate): Men over 50 with an enlarged prostate are more likely to develop prostatitis. The prostate gland may get obstructed. This facilitates bacterial growth. Chronic prostatitis symptoms can be similar to those associated with an enlarged prostate gland.
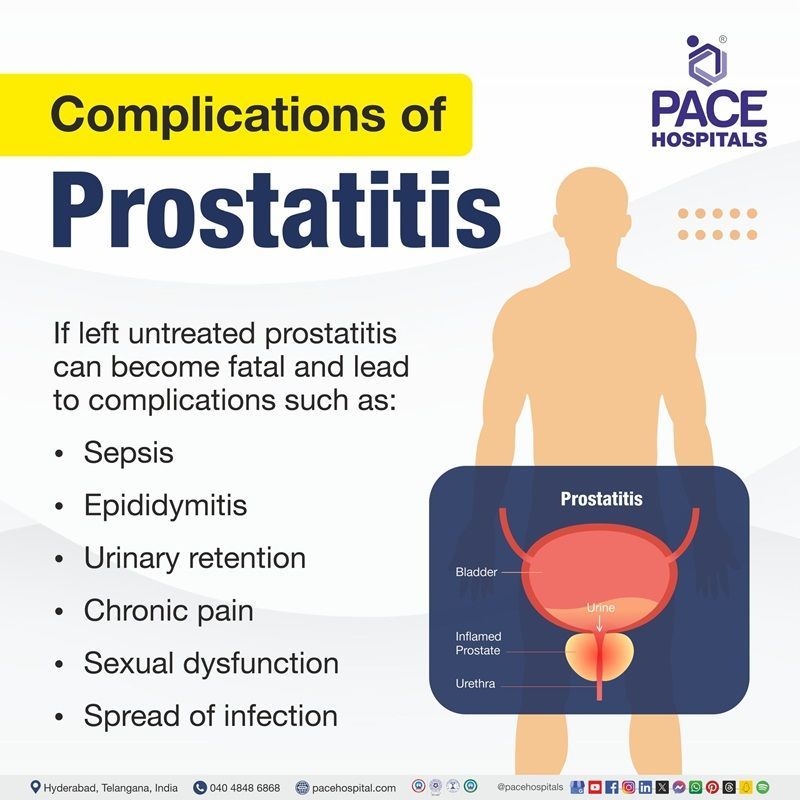
Complications of prostatitis
If left untreated, prostatitis can become fatal and lead to complications such as:
- Sepsis: An infection that can be fatal that spreads throughout the body that needs to be treated right away
- Epididymitis: An illness that results in inflammation of the epididymis, the coiled tube that stores and transports sperm from the testicles
- Urinary retention: The Inability of a man to urinate
- Chronic pain: Chronic pelvic pain or discomfort
- Sexual dysfunction: An inability to be involved in sexual intercourse
- Spread of infection: Infection that extends to the lower spine or higher pelvic bone
Prostatitis diagnosis
Initially, the patient may visit the general physician with the worrying symptoms. The general physician then refers the patient to a urologist for further evaluation.
The urologist diagnoses prostatitis based on:
- Personal and family medical history of the patient
- Physical examination
- Medical tests
Before diagnosing prostatitis, a urologist may need to rule out other illnesses that may present with similar signs and symptoms.
Personal and Family Medical History
Taking a personal and family medical history is one of the first things a urologist may do to help diagnose prostatitis.
Physical Exam
During a physical exam, a urologist usually examines a patient’s body, which can include checking for:
- Discharge from the urethra
- Enlarged or tender lymph nodes in the groin
- A swollen or tender scrotum
- Performs a digital rectal exam
Medical Tests
A urologist uses medical tests to help diagnose lower urinary tract problems related to prostatitis and recommend treatment. Medical tests may include:
- Blood tests
- Urinalysis
- Cystoscopy
- Urodynamic tests
- Transrectal ultrasound
- Semen analysis
- Biopsy
Prostatitis treatment
Treatment of prostatitis varies depending on the type of prostatitis.
Chronic prostatitis/chronic pelvic pain syndrome
The goal of treating chronic prostatitis/chronic pelvic pain syndrome is to reduce pain, discomfort, and inflammation. There are several symptoms, and no single treatment is effective for all men. Although antibiotics will not treat nonbacterial prostatitis, a urologist may prescribe them initially to rule out a bacterial infection. A urologist may prescribe additional medications which include:
- Alpha blockers
- 5-alpha reductase inhibitors
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Muscle relaxants
- Neuromodulators
Alternative treatments may include:
- Warm baths, called sitz baths
- Local heat therapy with hot water bottles or heating pads
- Physical therapy, such as:
- Kegel exercises—tightening and relaxing the muscles that hold urine in the bladder and hold the bladder in its proper position. Also called pelvic muscle exercises.
- Myofascial release—pressing and stretching, sometimes with cooling and warming, of the muscles and soft tissues in the lower back, pelvic region, and upper legs. Also known as myofascial trigger point release.
- Relaxation exercises
- Biofeedback
- Phytotherapy with plant extracts such as quercetin, bee pollen, and saw palmetto
- Acupuncture (insertion of fine needles into the skin to treat health conditions)
Acute bacterial prostatitis
A urologist uses antibiotics to treat acute bacterial prostatitis. The antibiotic prescription may vary according to the type of bacteria causing the infection. Urologists typically prescribe oral antibiotics for at least two weeks. Some urologists recommend taking oral antibiotics for 6 to 8 weeks because the infection may reoccur. Severe cases of acute prostatitis may necessitate a brief hospital stay for men to receive fluids and antibiotics via an intravenous (IV) tube. Following the IV therapy, men will have to take oral antibiotics for 2 to 4 weeks.
Many instances of acute bacterial prostatitis resolve entirely with medication and minor dietary adjustments. The urologist may advise avoiding bladder irritants including alcohol, caffeinated beverages, and acidic and spicy meals, as well as increasing fluid consumption (64 to 128 ounces per day) to promote frequent urination and eliminate bacteria.
Chronic bacterial prostatitis
A urologist uses antibiotics to treat chronic bacterial prostatitis, however, treatment needs a bit more time to avoid recurring infections. The urologist may give low-dose antibiotics for up to 6 months. If the infection persists, the urologist may prescribe another antibiotic or a combination of medications. The urologist may advise the patients to drink more fluids and avoid or limit intake of bladder-irritating substances.
A urologist may prescribe alpha blockers to treat urinary retention caused by persistent bacterial prostatitis. Men may need surgery to relieve urinary retention caused by persistent bacterial prostatitis. Surgically eliminating scar tissue from the urethra can often enhance urine flow and lessen urinary retention.
Prostatitis prevention
Although there's no absolute way to avoid this condition, individuals can maintain the health of the prostate by making numerous minor lifestyle adjustments. The lifestyle modifications that help to prevent prostate issues and ensure prostate health include:
- Maintaining good hygiene: Ensuring that the area around the penis is clean and hygienic, may help prevent the occurrence of bacterial infection that can eventually cause bacterial prostatitis (inflammation of the prostate gland due to bacterial infection).
- Avoiding prolonged sitting: Long periods of sitting exert pressure on the prostate gland, which eventually causes inflammation. To prevent prostate issues, staying away from frequent long bike rides and extended periods of sitting.
- Indulging in a workout: It is highly recommended to exercise at least three or more times per week. Physical activity helps alleviate anxiety, which has been linked to certain kinds of prostatitis. Men with an irritated prostate have also reported that doing workouts helps them feel better.
- Maintaining good hydration: Some types of prostatitis develop when bacteria in the urinary tract enter the prostate and produce an infection. Staying hydrated to keep the urine diluted and the bladder flushed out. In case of a pre-existing medical condition, such as chronic kidney disease or congestive heart failure, consult a urologist promptly to get some advice regarding the safety measures.
- Consuming a nutritious diet: Eating an highly nutritious diet can help prevent infections and inflammation in the body by ensuring overall health.
- Avoiding foods that worsen prostatitis: Nothing in the data that supports the claim that a certain diet helps prevent prostatitis. However, spicier meals, chili, and hot peppers might irritate the bladder and exacerbate the symptoms of prostatitis.
- Limiting caffeine and alcohol abstinence: Consuming excess amounts of caffeine and alcohol can inflame and irritate the urinary tract and the prostate.
- Maintaining healthy weight: Prostate health is negatively impacted by obesity (overweight). A balanced diet, regular exercise, and adequate sleep could help to reduce extra weight.
- Managing stress: Prostatitis is more common in men who experience extreme stress at work or in their personal lives. Seeking therapy may assist in managing the emotions. Patients can also pick up skills like total body relaxation or meditation to ease the stress.
- Practicing safe sex practices: Prostatitis can occasionally result from sexually transmitted infections (STIs). Bacteria can enter the urethra during intercourse with an infected partner if the safety measures are not followed. The bacteria may end up infecting the prostate eventually. Using a condom every time during intercourse prevents the bacteria from entering the urinary tract.
Differences between Enlarged prostate and Prostate inflammation
Although both conditions affect the prostate gland, prostatitis and an enlarged prostate differ in their clinical presentation. The table below contains the basic differences between the two conditions:
| Feature | Prostate enlargement (BPH-Benign prostatic hyperplasia) | Prostate Inflammation (Prostatitis) |
|---|---|---|
| Definition | Noncancerous enlargement of the prostate gland | Inflammation of the prostate gland |
| Common Age Group | Men over 50 years old | Men under 50 years old |
| Causes | Aging, hormonal changes | Bacterial infection, stress, other unknown factors |
| Symptoms | Difficulty urinating, weak urine flow, nocturia | Pain in pelvis, painful urination, fever, chills |
| Onset | Gradual | Can be sudden (acute) or gradual (chronic) |
| Diagnosis | Digital rectal exam, urine tests, PSA blood test | Urine tests, blood tests, prostate fluid tests |
| Treatment | Medications, lifestyle changes, surgery | Antibiotics, pain relievers, alpha-blockers |
| Complications | Urinary retention, bladder stones, kidney damage | Chronic pain, reduced libido, fertility issues |
Frequently Asked Questions (FAQs) on Prostatitis
What is the main cause of prostatitis?
Bacteria are the most common cause of prostatitis. They spread from the rectum or by contaminated urine. Men cannot get prostatitis from another individual as it is not a sexually transmitted infection (STI). However, it can occur due to the bacteria that gets transmitted through intercourse with an infected person.
What are the first signs of prostate problems?
The initial signs of prostate problems might vary, but frequent ones include frequent urination especially during the night (nocturia), urgency to urinate, feeling a sudden and strong urge to urinate, difficulty in starting to urinate, blood in urine (haematuria) or semen (hematospermia). pain or discomfort in the pelvic area, lower back, or during urination or ejaculation.
Over time, poor diabetes control may cause more damage to the nerves and circulation that control blood flow to the penis. Keeping blood glucose levels within the usual range will help lessen the likelihood of these problems arising.
Can someone live a normal life with prostatitis?
Yes, it is possible to live a somewhat normal life with prostatitis, which is an inflammation or infection of the prostate gland. However, long-term prostatitis can be difficult to manage, and the pain or discomfort might make it difficult to complete daily duties. One may also encounter flare-ups without warning.
What diet causes prostatitis?
A research study has found that certain foods do aggravate prostatitis symptoms with the most aggravating being the spicy foods, coffee, hot peppers, alcoholic beverages, tea, and chili. On the contrary, the foods that may alleviate the symptoms the most include docusate, psyllium, water, herbal teas, and polycarbophil.
Can prostatitis clear itself?
No. If prostatitis is caused by a bacterial infection, it will not resolve itself. Patients require medication to treat the infection. However, if the patient has nonbacterial prostatitis, the inflammation and tenderness may go away without treatment.
Where is the prostate located?
The prostate gland is located right below the bladder and above the pelvic floor muscles. The rectum is behind the prostate, so that urologist may feel the gland with their finger. The ducts in the prostate gland drain into the urethra, which runs through the prostate.
Is prostatitis life threatening?
Prostate gland inflammation, often known as prostatitis, is rarely fatal. However, it can be both uncomfortable and difficult to diagnose. Prostatitis can be caused by infection or inflammation, and it occurs in a variety of types and cause severe complications if left untreated.
How long can prostatitis last?
Bacterial prostatitis occurs when the prostate is infected with bacteria. The acute kind occurs suddenly and lasts only a short period, but the chronic type develops gradually and lasts for many years.
Is prostatitis common?
Yes, prostatitis is common, and many men will have it at some point in their life. It is the most frequent urinary tract condition in males under 50, and the third most prevalent in men over 50. In fact, up to 50% of men can suffer symptoms of prostatitis at some point.
What is prostate cancer?
Prostate cancer is cancer that affects the prostate gland. Cancer occurs when abnormal cells begin to divide and develop in an uncontrolled manner. The cells have the ability to expand into surrounding tissues or organs and spread throughout the body.
What size of the prostate is dangerous?
In some people, a small enlargement might cause major symptoms, but others may have lemon-sized prostates with few consequences. In general, the American Urological Association recommends surgical intervention for prostates with a volume of 30 cc or more with significantly lower urinary symptoms.
What are the prostate-specific antigen (PSA) levels for prostatitis?
There is ongoing debate over prostatitis' effect on semen parameters. It has been demonstrated that bacterial infections of the male reproductive system, such as chronic bacterial prostatitis have an adverse impact on sperm quality. Numerous investigations have demonstrated that both sperm motility and morphology are negatively impacted by chronic non-bacterial prostatitis.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868