Celiac Disease - Symptoms, Causes, Risk Factors and Complications
PACE Hospitals
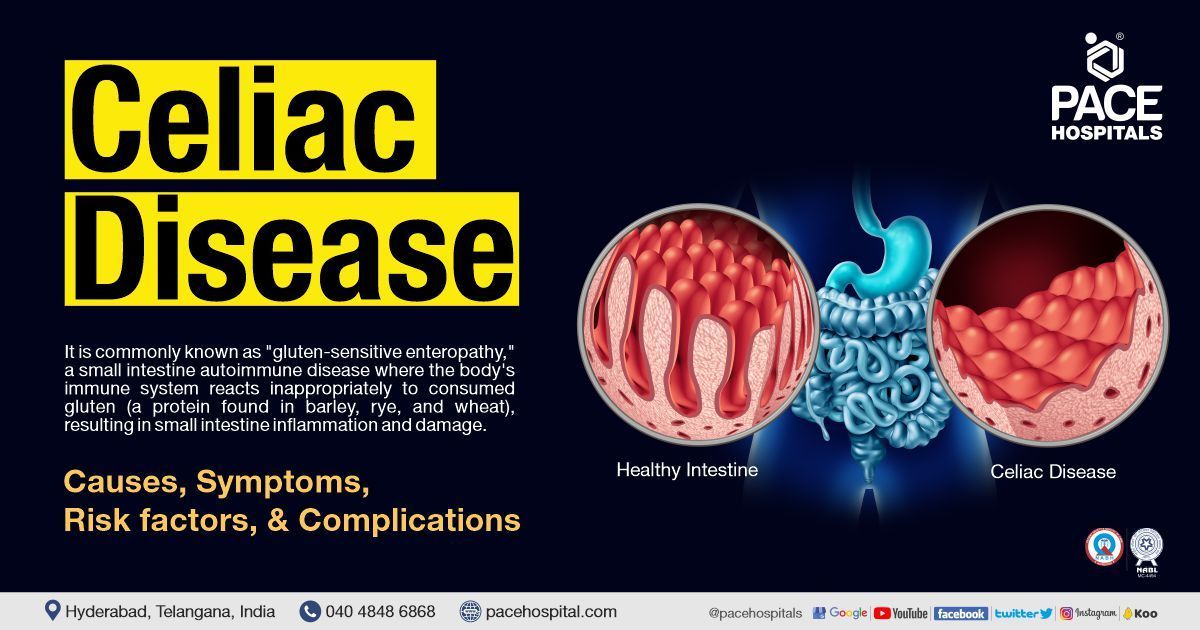
Celiac disease meaning
Celiac disease, commonly known as "gluten-sensitive enteropathy," is a small intestine autoimmune disease where the body's immune system reacts inappropriately to consumed gluten (a protein found in barley, rye, and wheat), resulting in small intestine inflammation and damage. This is a chronic condition, and patients with celiac disease can present with severe diarrhoea and failure to thrive, and some may be asymptomatic.
Celiac disease affects roughly 0.5 -1 % of the overall population. People suffering from autoimmune diseases, such as Addison's disease, type 1 diabetes, and microscopic colitis, have a higher risk. Avoid eating anything containing gluten is the only cure for celiac disease. The risk for nutritional deficiency and complications of celiac disease, as well as the required degree and duration of adherence to a gluten-free diet, can be identified by distinguishing between celiac disease and non-celiac gluten sensitivity.
Celiac Disease Causes
An individual with HLA-dominant DQ2 or DQ8 genes who is genetically predisposed has a higher chance of developing Celiac disease. The other possible contributors include infant feeding methods, gastrointestinal illnesses, and gut microorganisms. Surgery, pregnancy, childbirth, a virus (enterovirus and adenovirus infections), or extreme emotional stress can sometimes activate the celiac disease.
The condition is caused by the immune system's abnormal reaction to gluten. The glycoprotein gliadin (found in gluten) directly harms enterocytes (cells of the intestine) via increasing IL-15 production, leading to inflammation and the destruction of small intestinal villi.
Vili (a finger-like projection) presents in the inner lining of the small intestine and aids in the absorption of nutrients. The destruction of small intestinal villi results in diminished gut surface functionality and malabsorption. The lack of nutritional absorption has an immediate influence on the digestive system, in addition to an indirect impact on all of the body's systems.
Celiac Disease Symptoms
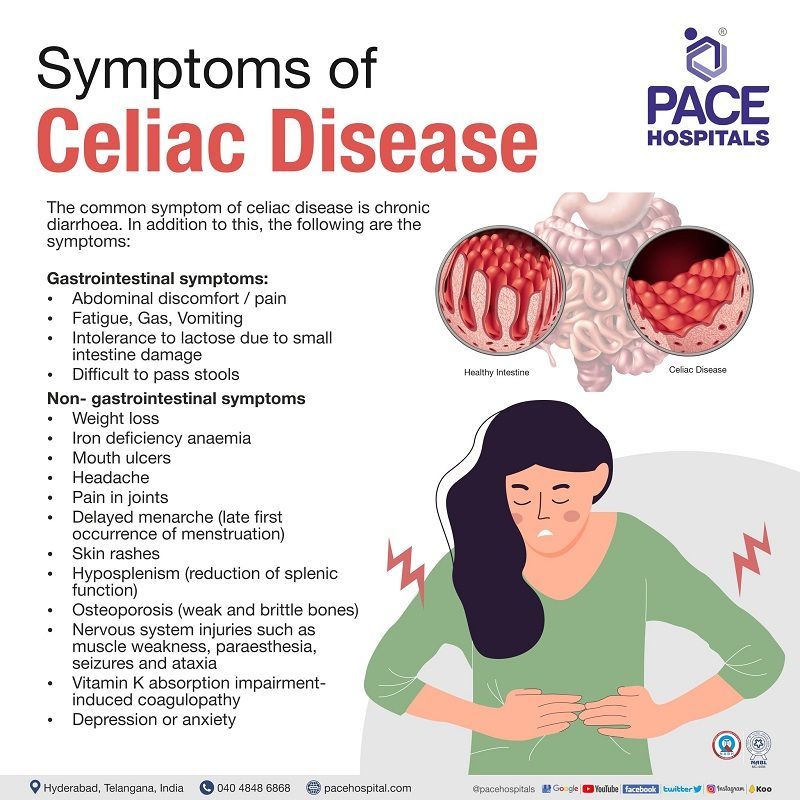
The common symptom of celiac disease is chronic diarrhoea (loose, watery, frequent bowel moments). In addition to this, the following are the symptoms:
Gastrointestinal symptoms:
- Abdominal discomfort/pain
- Fatigue
- Gas
- Vomiting
- Intolerance to lactose due to small intestine damage
- Difficult to pass stools
Non- gastrointestinal symptoms
- Weight loss
- Iron deficiency anaemia
- Mouth ulcers
- Headache
- Pain in joints
- Delayed menarche (late first occurrence of menstruation)
- Skin rashes
- Hyposplenism (reduction of splenic function)
- Osteoporosis (weak and brittle bones)
- Nervous system injuries such as muscle weakness, paraesthesia, seizures and ataxia
- Vitamin K absorption impairment-induced coagulopathy
- Depression or anxiety
Celiac disease symptoms in children
- Difficult to pass the stools
- Gas
- Chronic diarrhoea
- Delayed puberty
- Foul smelling stools
- Nausea & vomiting
- Abdominal swelling
- Loss of weight
- Anaemia
- Damage of tooth enamel
- Failure to thrive in infants
- Low height
- Neurological symptoms include attention-deficit hyperactivity disorder, seizures and lack of muscle coordination
- Irritability
Celiac Disease Risk Factors
As celiac disease (CD) is an autoimmune, people with the following autoimmune diseases and chromosomal abnormalities are at high risk of having celiac disease, such as:
Autoimmune diseases
- Type 1 diabetes
- Thyroid disease
- Addison's disease
Chromosomal abnormalities
- Down syndrome
- Williams-Beuren syndrome
- Turner syndrome
In addition to the above, people with dermatitis herpetiformis and a family history of celiac disease are also at increased risk for celiac disease.
Celiac Disease Complications
The following are the complications of celiac disease if it is not treated:
- Lymphomas
- Small bowel adenocarcinomas
- Miscarriage or newborn with congenital birth defects
- Short height and failing to thrive in children
- Secondary lactose intolerance
The consequences of poor nutrient absorption include:
- Decrease in bone mineral density
- Anaemia
- Malnutrition
- Seizures
- Bleeding diathesis (increased tendency to bleed)
Celiac Disease Screening
The celiac disease screening test is beneficial in patients with asymptomatic first-degree relatives of patients with a confirmed diagnosis of celiac disease. Serology tests to check for celiac disease antibodies should be performed on people who exhibit celiac disease symptoms.
Celiac Disease Diagnosis
The gastroenterologist will perform a physical exam and check the patient's medical and family history to determine the need to go for the following diagnostic tests.
- Serological tests for Immunoglobulin antibodies
- Biopsy of skin in individuals in case of Dermatitis Herpetiformis
- Genetic test
If the serologic tests are positive for celiac disease, the gastroenterologist may recommend further testing such as:
- Endoscopy biopsy of the small intestine
- Capsule endoscopy
Celiac Disease Treatment
Celiac disease treatment typically entails abstaining from gluten, as onlya strict, lifelong healthy gluten-free diet can aid in controlling the disease. In addition to this, the patient’s symptoms can be managed with gluten-free supplements
- Copper, folate, iron, zinc and vitamin supplements to manage anaemic, malabsorption and malnutrition condition
- Anti-acne agents to manage dermatitis herpetiformis
In addition to the above supplements, anti-inflammatory agents can be prescribed to reduce bowel inflammation.
Foods that contain gluten:
Wheat, barley, and rye are common constituents in various other eatable or consumable products in addition to a daily diet. Additionally, wheat is included as a flavour, colouring, or thickening ingredient. The following foods should be avoided if they are not labelled or mentioned as “gluten-free”.
- Processed foods like Pastas, French fries, Hot dogs and processed lunchmeats
- Liquid or semi-solid foods such as Salad dressings, Beer, Soups, Soya sauces
- Seasoned snack foods
- Crackers and croutons
- Sugar candies
- Cakes
- Cereals
- Seafood or meat flavoured
- Bread
Refractory celiac disease
In some rare instances, even while adhering to a gluten-free diet, symptoms and damage to the small intestine can persist or recur, a condition known as a refractory celiac disease that might cause serious complications such as cancer (T-cell lymphoma) conditions and malnutrition.
Frequently Asked Questions (FAQs) on Celiac Disease
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles