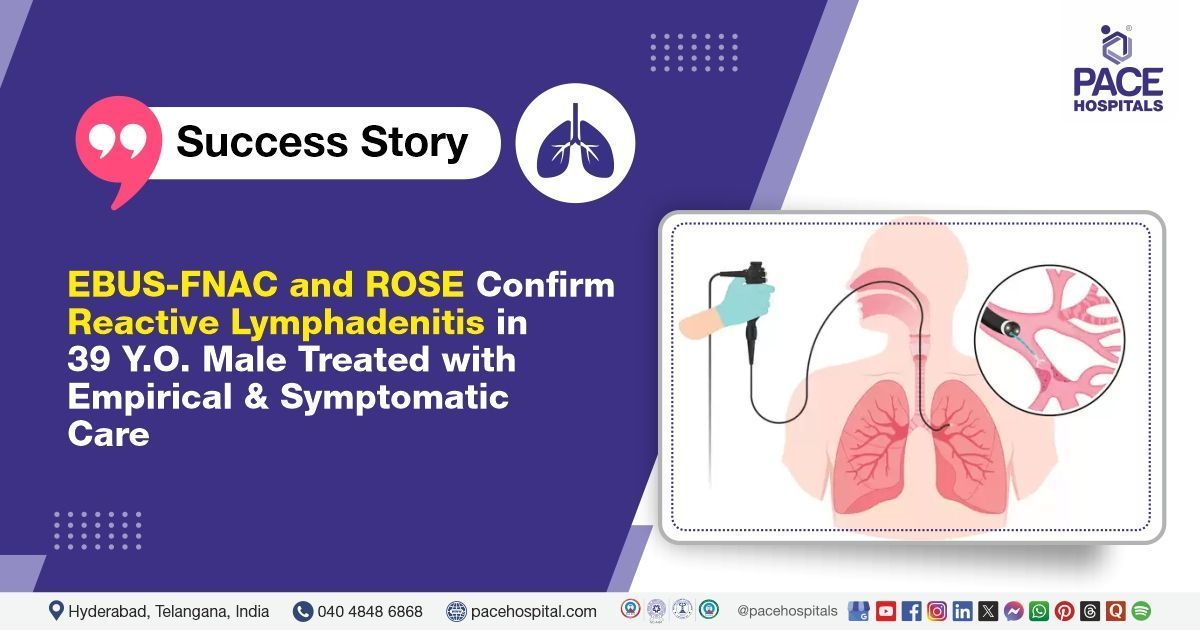
EBUS-FNAC and ROSE Confirm Reactive Lymphadenitis in 39 Y.O. Treated with Empirical and Symptomatic Care
PACE Hospitals
PACE Hospitals' expert pulmonology team successfully performed an endobronchial ultrasound (EBUS)-guided fine needle aspiration cytology (FNAC) on a 39-year-old male patient who had been experiencing a cough with scanty expectoration for the past few days. The procedure was undertaken to diagnose the condition & alleviate his symptoms, reduce the risk of future complications, and support optimal recovery.
Chief Complaints
A 39-year-old male patient with a body mass index (BMI) of 23.1 presented to the Pulmonology Department at PACE Hospitals, Hitech City, Hyderabad, with complaints of cold, nasal blockage, and a cough with scanty expectoration for the past few days. The cough worsened on bending forward and during meals and was associated with regurgitation, throat irritation, and postnasal drip. He also experienced shortness of breath on exertion, which subsided with rest. Additionally, he reported left-sided chest pain that had been increasing with movement over the past two days. The patient had a recent episode of streaky hemoptysis (Coughing up blood) and low-grade fever. He also complained about tinnitus in the left ear.
These symptoms pointed towards a possible upper and lower respiratory tract involvement, potentially exacerbated by gastroesophageal reflux. The presence of hemoptysis and exertional symptoms warranted further diagnostic evaluation to rule out infectious, inflammatory, or structural pulmonary conditions.
Past Medical History
The patient had a history of
hypertension, which was well-managed with regular antihypertensive medication. He also reported similar episodes of cold, and cough associated with seasonal changes over a long period. Additionally, he had a known allergy to dust, which likely contributed to his nasal blockage, postnasal drip, and throat irritation. These allergic tendencies, along with symptoms of
gastroesophageal reflux, may have played a significant role in aggravating his current cough and respiratory discomfort.
On Examination
Upon admission to PACE Hospitals, the patient’s vital signs were stable, and he was hemodynamically stable. On general examination, he was conscious, coherent, and cooperative, showing no signs of respiratory distress. There was no peripheral lymphadenopathy or paranasal sinus tenderness. Examination of the posterior pharyngeal wall revealed congestion and a granular appearance. Systemic examination showed normal cardiovascular findings with S1 and S2 heart sounds present. Chest auscultation revealed bilateral vesicular breath sounds, and the abdomen was soft with a positive percussion note.
Diagnosis
After the initial examination, the pulmonology team conducted a thorough evaluation, reviewing the patient’s medical history and symptoms. They aimed to identify any underlying causes of his respiratory issues and planned further tests to assess his cough, chest pain, and hemoptysis.
His investigations revealed normal complete blood picture (CBP), renal function tests (RFT), liver function tests (LFTs), immunoglobulin E (IgE) levels, absolute eosinophil count (AEC), hemoglobin A1C (HbA1C), serum calcium, prothrombin time (PT), international normalized ratio (INR), and activated partial thromboplastin time (APTT). Viral screening and multiplex flu PCR tests were negative, ruling out common viral infections. His blood group was identified as O-positive. Ultrasound of the abdomen showed Grade I fatty changes in the liver, indicating mild hepatic steatosis. A contrast-enhanced CT (CECT) of the chest revealed a few sub-centimeters calcified mediastinal lymph nodes but no evidence of any acute cardiopulmonary process, which helped exclude active infection or malignancy. The CT scan of the paranasal sinuses (CT PNS) demonstrated a minimally deviated nasal septum to the left side with a septal spur and mild hypertrophy of bilateral inferior turbinate’s, findings that could contribute to his nasal congestion and postnasal drip symptoms. These findings, combined with the clinical suspicion, led to the decision to proceed with an EBUS-guided FNAC procedure to further investigate the cause of the patient's symptoms.
Based on the patient's current condition, the doctors recommended performing an EBUS-FNAC (Endobronchial Ultrasound-Guided Fine Needle Aspiration Cytology) to investigate the underlying cause of the patient's condition, which was suspected to be tuberculosis.
The procedure was carried out as part of the patient's mediastinal lymphadenopathy treatment in Hyderabad, India, under the care of the Pulmonology Department ensuring comprehensive management.
Medical Decision Making (MDM)
After being admitted to PACE Hospitals, Dr. Pradeep Kiran, Consultant Interventional Pulmonologist, thoroughly reviewed the patient’s medical history and conducted a detailed clinical examination. Laboratory investigations and imaging studies, combined with clinical suspicion, indicated the need for further evaluation.
Based on the findings, an EBUS-guided FNAC procedure was performed to investigate the underlying cause of the patient’s persistent respiratory symptoms.
The patient and his family were thoroughly counseled about his condition, including the need for the EBUS-guided FNAC procedure, along with its potential benefits and associated risks. The discussion emphasized how the procedure would aid in accurately diagnosing the underlying cause of his symptoms and guide appropriate treatment, particularly considering the clinical suspicion of tuberculosis.
Surgical Procedure
Following the decision, the patient was scheduled to undergo an endobronchial ultrasound (EBUS)-guided fine needle aspiration cytology (FNAC) in Hyderabad at PACE Hospitals under the expert supervision of the pulmonology Department.
The patient was taken for an EBUS-guided FNAC under general anesthesia as part of the diagnostic workup for his persistent respiratory symptoms and clinical suspicion of tuberculosis. The procedure began with a bronchoscopy, which revealed normal airways. Bronchoalveolar lavage (BAL) was collected from both lungs for microbiological and cytological analysis. Endobronchial biopsies were also taken from multiple sites and sent for further investigation.
Subsequently, endobronchial ultrasound (EBUS) was performed, which identified a Station 7 mediastinal lymph node measuring 8.1 × 10.2 mm, showing vascularity and multiple calcifications—features often associated with chronic granulomatous conditions such as tuberculosis. A total of five needle passes were made into the Station 7 node, and the aspirated material was sent for cytological, microbiological, and molecular analysis.
Rapid on-site evaluation (ROSE) was conducted during the procedure, which was suggestive of reactive lymphadenitis. These findings supported further investigation to confirm the diagnosis and guide appropriate treatment.
Postoperative Care
The procedure was uneventful, and the patient was extubated on the table and shifted to the Medical Intensive Care Unit (MICU) for observation for six hours. Following stable post-procedural vitals and recovery, he was transferred to the ward. During his hospital stay, the patient was treated with intravenous antibiotics, nebulization, antihypertensive medications, and other supportive treatments tailored to his clinical condition. A Mantoux test was performed, which showed a negative result.
Once his condition stabilized, the patient was prepared for discharge with detailed instructions on home care and scheduled follow-up appointments to monitor his progress and ensure treatment adherence.
Discharge Medications
Upon discharge, the patient was prescribed a combination of oral antibiotics to address any residual or secondary bacterial infection, along with nebulization to relieve airway inflammation and improve respiratory function. Antihistamines were included to manage allergic symptoms such as nasal congestion and postnasal drip, which were contributing to his cough and throat irritation. Antihypertensive medications continued to ensure stable blood pressure control. Proton pump inhibitors were prescribed to manage gastroesophageal reflux, which was likely exacerbating his respiratory symptoms. Additional supportive treatments were advised to aid recovery and enhance overall symptom relief.
Advice on Discharge
The patient was given specific instructions to consult a Medical Gastroenterologist and get evaluated for Upper GI causes of persistent cough (to check GERD).
Emergency Care
The patient was informed to contact the Emergency ward at PACE Hospitals in case of any emergency or development of symptoms like fever, abdominal pain, persistent cough, and vomiting.
Review and Follow-Up
The patient was advised to return for a follow-up visit with the pulmonology Department at PACE Hospitals after 7 days with Bronchoalveolar lavage (BAL), Endobronchial Biopsy, and EBUS FNAC reports.
Conclusion
This case highlights the importance of a multidisciplinary approach in diagnosing and managing mediastinal lymphadenopathy and suspected pulmonary tuberculosis, especially in patients with complex symptoms. Collaboration among specialists was crucial for accurate diagnosis and effective treatment in Hyderabad, India.
The Role of Rapid On-Site Evaluation (ROSE) in Interventional Pulmonology
Rapid On-Site Evaluation (ROSE) is a real-time cytological examination technique used in diagnostic interventional pulmonology to enhance the efficiency and accuracy of procedures such as transbronchial needle aspiration (TBNA). It involves the immediate assessment of tissue samples under a microscope by a pathologist or trained professional, providing instant feedback to the pulmonologist/ pulmonology doctor performing the procedure. This real-time guidance helps minimize the number of biopsies required and reduces the overall procedure time. However, implementing ROSE demands dedicated resources, including trained personnel, specialized equipment, and a suitable environment, which can pose challenges for some institutions.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868