The Kasai Procedure for Biliary Atresia | Surgery Indications & Types
At PACE Hospitals, the advanced OT is equipped with World's first universal AI surgical robotic system and world-class 3D HD laparoscopic and laser equipment to perform minimally invasive major and supra-major surgeries of gastrointestinal system.
Our team of the best surgical gastroenterologist in Hyderabad, Telangana and top liver transplant surgeons in India are having extensive experience in performing the Kasai procedure for biliary atresia treatment in a child.
Request Appointment for Kasai Procedure
Kasai procedure - appointment
Why Choose PACE Hospitals for Kasai Procedure?
100+ the Kasai procedure performed for biliary atersia
Team of the best surgical gastroenterologist with 30+ years of expertise
Cost-effective treatment with 99.9% success rate
All insurance accepted with No-cost EMI option
What is the Kasai Procedure?
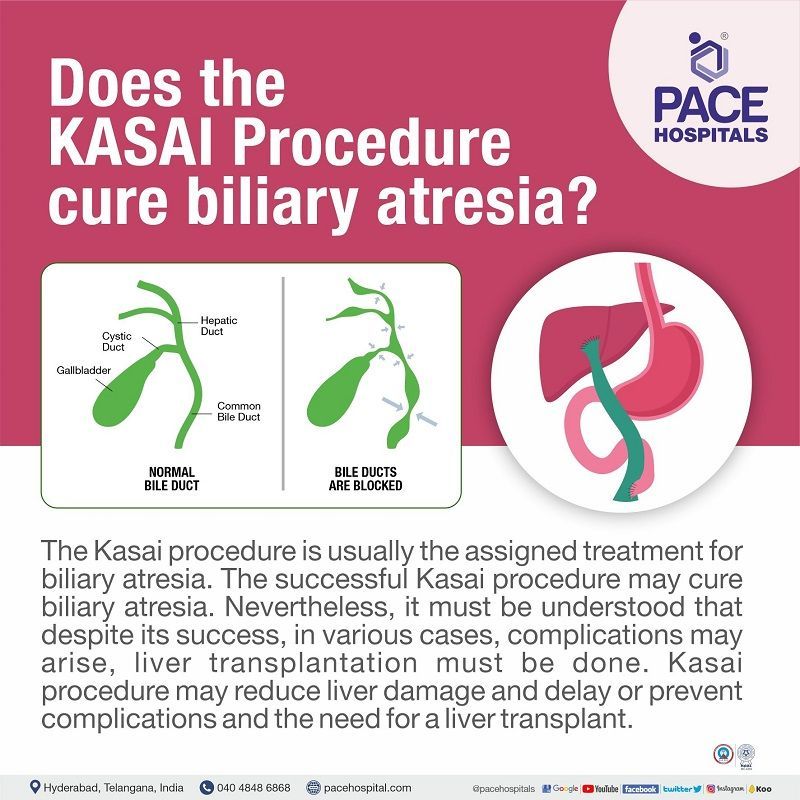
The Kasai procedure, also called Kasai portoenterostomy or hepaticoportoenterostomy, is a surgical procedure to facilitate bile drainage in neonates (newborn) suffering from biliary atresia.
Biliary atresia is a congenital disorder in which the tubes (ducts) that transport bile from the liver to the gallbladder are obstructed. It could be fatal if left untreated by damaging the liver and forming cirrhosis.
- Kasai surgery’s goal is to obtain a total biliary drainage (total bilirubin level < 2.0 mg/dL at any time during the first three months after the surgery)
- Kasai operation demands technical vigour, dexterity and precision. Too shallow cut can obstruct the other small bile ductules and a deep cut can bleed and scar the liver, leading to fibrosis.
What are the uses or indications of the Kasai procedure?
Biliary atresia is a progressive fibro-obliterative disease of the extrahepatic biliary tree that presents as direct hyperbilirubinemia in the neonatal period. In neonates suffering from biliary atresia, the flow of bile is obstructed, leading to various malnutritional complications. Biliary atresia may prognose into sclerosis, eventual liver fibrosis and failure.
Kasai hepaticoportoenterostomy remains the first treatment choice for biliary atresia in the
liver transplantation era to date. It has no contraindications.
Types of the Kasai Procedure
The potential variants of the Kasai procedure include the following:
- Gallbladder Kasai
- Kasai procedure with ostomy (an artificial opening through surgery)
- Kasai procedure with intussusception antireflux valve (intussusception is the infolding of intestine)
Goals the Kasai Procedure
The goal of the Kasai operation is to obtain total biliary drainage in patients who have biliary atresia. A total bilirubin level of less than 2.0 mg/dL at any time during the first three months after a Kasai procedure is considered a sign of good biliary drainage.
The Criticality of Surgical Expertise in Kasai Procedure
The Kasai procedure is rarely performed in the general paediatric surgical department and is definitely not a simple operation. It demands technical vigour, high levels of dexterity and precision for various steps in the process, such as the dissection of fibrous cone and portoenterostomy. This learning curve can be only obtained by hours of practice under the guidance of super specialist surgeons.
One of the main processes in which technical precision and polished dexterity are necessary is the dissection technique. If the dissection is made too shallow, then the freed fibrous tissue could obscure the other small bile ductules. On the other hand, if the dissection is made too deep into the parenchyma of the liver, bleeding and scarring may lead to fibrosis at the porta.
Kasai Procedure Steps
Before the Kasai Procedure
The parents present the newborn to the paediatric clinic with complaints of biliary atresia. One of the most common symptoms includes cholestatic jaundice. Through abdominal ultrasonography, the obstruction of bile ducts is discovered, which concludes most of the diagnostic process. With the established diagnosis, the doctors fix a date for the operation. Before the commencement of the procedure, the patient was kept fasting for at least 8 hours.
Prior to the procedure, a coagulogram may be executed, which displays the coagulation of blood over time, and vitamin K administration may not be necessary if a change was not noticed in the diagnostic.
During the Kasai Procedure
- The patient is positioned in dorsal decubitus (lying on the back) and in a reverse Trendelenburg (making the bed slanted at 30°, keeping the head in high position than the rest of the body) for better access to the liver.
- With appropriate aseptic, antiseptic and anaesthetic work, a transverse incision is done in the upper abdomen ("Chevron incision") of approximately 12-15 cm. This exposes the entire liver and biliary tree.
- With the exposed biliary tree, a final inspection of the liver and biliary tract is done, re-confirming the diagnosis.
- In most cases, due to the complete absence of an extrahepatic biliary tract, it was neither possible nor necessary to perform intraoperative cholangiography to confirm biliary atresia.
- In case the diagnosis is more obscure, the team may opt for an intraoperative trans-gallbladder cholangiography.
- An open or tru-cut liver biopsy is usually performed for histological examination to confirm the diagnosis and assess the stage of liver disease.
- Liver mobilisation is accomplished by severing the falciform, coronary, and right and left triangular ligaments. Through this step, the liver will be freed.
- Cutting from the remaining gallbladder exposes and isolates the extrahepatic bile duct.
- Hepatic arteries and the portal vein are identified, carefully isolated and dissected till to their entrance into the liver.
- The distal common bile duct is ligated and divided.
- Porta hepatis is now cut to obtain a bile extravasion (draining of bile).
- Although haemostasis through cauterisation must be avoided, eventual perforating branches of the portal vein can be ligated with 5/0 non-absorbable suture.
- The porta hepatis is then packed, and the liver is replaced into the abdominal cavity.
- The jejunum (a part of the small intestine) is divided at around 10-20 cm distal to the ligament of Treitz.
- A Roux loop is constructed at about 40 cm along the anti-mesenteric border, and the distal end is brought up to the porta hepatis through a right-sided window in the transverse mesocolon.
- To avoid an eventual internal hernia (either small or large intestine pushes through the mesentery (connective tissue holding the intestines in place), the mesenteric defect should be removed with absorbable interrupted sutures.
- The end-to-end or end-to-side anastomosis (connection or opening between two tubes) at the porta hepatis is then made.
- The mesocolic window is secured around the Roux loop, and the liver is finally relocated into the abdominal cavity.
- A drain may be introduced through the foramen of Winslow.
- The abdomen is closed in layers.
After the Kasai Procedure
A cholangiography can be performed at the end of the surgery to confirm the flow of bile in the bile duct from the gallbladder to the duodenum.
Outcome after Successful Kasai Procedure
The outcome after a successful Kasai operation can be measured by the
- successful restoration of bile flow
- normal coloured stools
- recovery from jaundice
This procedure might take a few weeks or months. The development of biliary cirrhosis is forestalled or possibly postponed; It has been reported that people with the native liver can live to adulthood.
Follow-up of the Kasai Procedure
The follow-up of the Kasai operation can measure once a month for six months and then quarterly indefinitely through the following tests:
- Blood pressure
- Alanine transaminase (ALT)
- Aspartate transaminase (AST)
- Alkaline phosphatase
- Gamma-glutamyltransferase
- Cholesterol
- Total protein and albumin
- Coagulogram
- Complete blood count
- Bilirubin
- Calcium
- Phosphor and
- Blood glucose
Benefits of the Kasai Procedure
The benefits of Kasai Procedure could include:
- Restoration of bile flow
- Assurance of proper nutrition (now oil foods can also be ingested)
- Cured cholestatic jaundice
- Proper development of the baby (now that the bile flow is restored)
History of the Kasai Procedure
The Kasai Procedure is developed by Dr Morio Kasai (1922–2008), and is one of the greatest innovators in the paediatric surgery field. He performed the first Kasai operation in 1955 as a treatment for a 72-day-old biliary atresia infant.
There are no extrahepatic bile ducts formed in the patient’s body. Dr Morio Kasai placed the duodenum over the porta hepatis (a deep, short, transverse fissure that passes across the left posterior aspect of the under surface of the right lobe of the liver) in the incised region where the bleeding appeared to originate, thus attaining haemostasis.
The postoperative follow-up demonstrated the normal coloured faeces, determining the bile flow. It is further reinforced by the eventual complete resolution of jaundice. The entire procedure was published in the Japanese journal - Shujutsu in 1959.
Kasai Procedure Complications
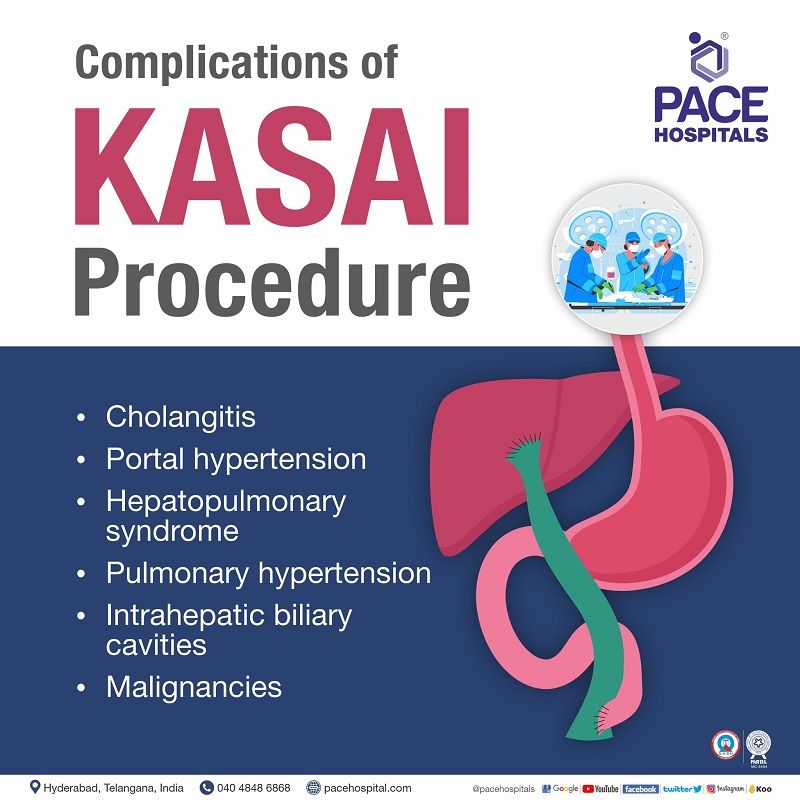
The most common complications which could be potentially seen after the Kasai operation include the following:
- Cholangitis (inflammation of the bile duct system)
- Portal hypertension (increased blood pressure in the portal venous system)
- Hepatopulmonary syndrome (low oxygen in the blood due to dilated intrapulmonary blood vessels)
- Pulmonary hypertension (increased pressure in the pulmonary artery)
- Intrahepatic biliary cavities
- Malignancies
Cholangitis: Bacterial cholangitis (inflammation of the bile duct system) can be caused by direct contact of the gut with the dystrophic intrahepatic bile ducts, as well as inadequate bile flow. It occurs in 30-60% of instances in the initial weeks/months following the Kasai operation.
Cholangitis can be serious and even fatal. Sepsis symptoms include:
- fever or hypothermia (reduced body temperature)
- impaired hemodynamic status (imbalance in blood flow)
- recurrent jaundice (yellowing of skin and eyes)
- acholic stools (clay-coloured stools due to lack of bile pigment), and maybe
- abdominal discomfort.
The healthcare personnel may prescribe interveinal antibiotics and successful interveinal resuscitation (fluids through the interveinal route) to treat cholangitis.
Portal hypertension: Portal hypertension (increased blood pressure in the portal venous system) is seen in at least two-thirds of children who underwent the procedure, even those with restored bile flow. Varices are often seen in the oesophagus, stomach, Roux loop, and anorectum (anal and rectal areas). The hepatologist may opt for pediatric liver transplantation in the case of failed Kasai procedure.
Hepatopulmonary syndrome: Hepatopulmonary (low oxygen in the blood due to dilated intrapulmonary blood vessels) syndrome often produces
- hypoxia (low oxygen levels in the blood)
- cyanosis (blue discolouration of the skin due to inadequate oxygenation)
- dyspnoea (difficulty in breathing), and
- digital clubbing (type of finger deformity).
Pulmonary scintigraphy (imaging test to see pulmonary arterial blood flow) confirms the diagnosis.
Pulmonary hypertension: Pulmonary hypertension (increased pressure in the pulmonary artery) can develop in cirrhotic youngsters, causing syncope (blacking out) or even death. Echocardiography is used to diagnose pulmonary hypertension. Paediatric liver transplantation can correct pulmonary shunts and pulmonary hypertension (particularly when detected early).
Intrahepatic biliary cavities: Despite jaundice clearance, large intrahepatic biliary cysts may form months to years following the Kasai procedure in the patients. These cavities may get infected or compress the portal vein requiring external drainage. Eventually, a cystoenterostomy or liver transplantation may be necessary.
Malignancies: Regular screening for malignancy must be performed among the patients who underwent a successful Kasai operation.
Outcome After Failed Kasai Procedure
In case the Kasai procedure falls short in the restoration of the bile flow resulting in the prognosis of biliary cirrhosis, liver transplantation may be necessary. Although liver transplantation is often performed in the second year of life, in many cases, it could be done as early as six months of age, depending upon the worsening of the liver condition.
Biliary atresia accounts for more than 50% of paediatric liver transplant indications. Recurrence of jaundice (next failure of the Kasai procedure) or consequences of cirrhosis (such as hepatopulmonary syndrome) may also need transplantation, despite the original success of the Kasai operation.
There are two sources of liver grafts:
- Cadaveric donor: The transplant is rarely a full-size liver from a size-matched paediatric donor. The transplant usually comprises the left liver (2+3+4) or left lobe (segments 2+3) acquired via reducing or dividing an adult liver graft.
- Living-related donor: usually from one of the parents of the child.
The research states that patient survival following liver transplantation present stands at more than 80% after five and ten years.
Kasai Procedure Success Rate
When procedure done within 60 days of birth, the Kasai surgery has an approximate 68% success rate. After 90 days, the response rate dramatically plummets to as low as 15%. Despite the underlying influence of the infant's age on prognosis, a late diagnosis (beyond 90 days) does not always indicate that the surgery will fail. The Kasai method has been utilised successfully on infants as young as seven months.
Recovery period
After hospitalisation, the liver and bile flow may take time to repair. Cholangitis may occur and regular oral antibiotics may be given for treatment which may continue for months. Handwashing, immunizations, and avoiding colds and flu are essential to prevent cholangitis.
Breastfeeding is necessary as it has liver-friendly fats.
Questions which the patients can ask to the healthcare team
- Is the Kasai Procedure safe?
- Is Kasai procedure the absolute treatment for Biliary Atresia?
- What will be the baby’s diet after the Kasai procedure?
- When can we see the outcomes of Kasai surgery?
- Can the baby lead a normal life after the Kasai operation?
Kasai Procedure Cost in Hyderabad, India
The cost of the Kasai Procedure in Hyderabad generally ranges from ₹1,80,000 to ₹4,50,000 (approx. US $2,160 – US $5,400).
The exact cost varies depending on the severity of biliary atresia, age of the infant, pre-operative stabilization, diagnostic evaluations (ultrasound, HIDA scan, liver function tests), surgical complexity, pediatric anesthesia, NICU stay, postoperative monitoring, and hospital facilities — including cashless insurance, TPA corporate tie-ups, and support with medical insurance documentation wherever applicable.
Cost Breakdown According to Type of Kasai Procedure–Related Care
- Pediatric Hepatologist / Pediatric Surgeon Consultation – ₹1,000 – ₹2,000 (US $12 – US $24)
- Basic Blood Tests (LFT, CBC, Coagulation Profile) – ₹1,200 – ₹3,500 (US $14 – US $42)
- Ultrasound Abdomen – ₹1,200 – ₹2,500 (US $14 – US $30)
- HIDA Scan (Biliary Atresia Evaluation) – ₹3,000 – ₹8,000 (US $36 – US $96)
- Pre-operative Stabilization (IV Fluids, Antibiotics, Supportive Care) – ₹5,000 – ₹18,000 (US $60 – US $215)
- Kasai Procedure (Hepatoportoenterostomy Surgery) – ₹1,80,000 – ₹3,80,000 (US $2,160 – US $4,560)
- NICU Stay (3–10 Days) – ₹25,000 – ₹70,000 (US $300 – US $840)
- Post-operative Monitoring & Medications – ₹10,000 – ₹30,000 (US $120 – US $360)
- Follow-Up Liver Function Monitoring – ₹2,000 – ₹6,000 (US $24 – US $72)
Frequently Asked Questions (FAQs) on Kasai Procedure
At what age is the Kasai procedure done?
Although late Kasai portoenterostomy or Kasai hepaticoportoenterostomy is frequently unsuccessful in re-establishing bile flow, the rate of success is greatest if done early, at younger than two months of age.
What is the Kasai procedure golden period?
The golden period to treat congenital biliary atresia in neonates is 100 days after birth; one day late, the kid's probability of success decreases by 1%, and after 100 days, the child may no longer have a chance.
When was the first Kasai procedure done?
Dr. Morio Kasai conducted the first Kasai surgery on a 72-day-old child with biliary atresia in 1955. The postoperative follow-up demonstrated the normal coloured faeces and eventual complete resolution of jaundice. The entire procedure was published in the Japanese journal - Shujutsu in 1959.
What is the Kasai procedure scar?
The provision for laparoscopic surgery is not feasible. Since this is an open surgery (unlike laparoscopic), the neonates do receive a Kasai procedure scar under the chest in the upper abdomen ("Chevron incision”). It is usually retained life-long.
What are the Anaesthetic concerns in the Kasai procedure?
The Kasai procedure anaesthesia includes blood loss and provision of adequate postoperative analgesia. Also, infection is seen due to the reduced immunity in these patients.
How long does the Kasai Procedure take?
The Kasai Procedure usually takes 4 to 5 hours to complete. Surgical Gastroenterologist will select the best and safest method such as laparoscopic surgery or open surgery before performing the surgery.