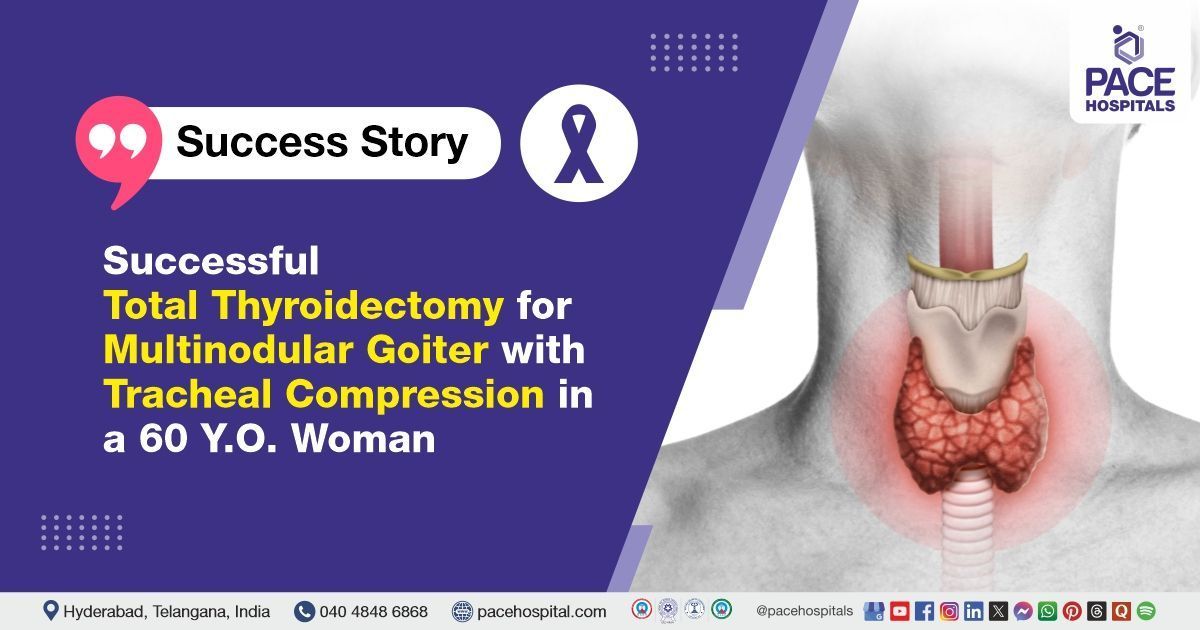
Successful Total Thyroidectomy for Multinodular Goiter with Tracheal Compression in a 60-Year-Old Woman
PACE Hospitals
PACE Hospitals' expert Oncology team successfully performed a
total thyroidectomy surgery on a 60-year-old female patient who presented with shortness of breath, cough, chest heaviness, and mild neck pain for a month. The surgery was performed to prevent further complications, reduce the patient’s symptoms, and improve her overall quality of life.
Chief complaints
A 60-year-old female patient with a
body mass index (BMI) of 25 presented to the Oncology Department at
PACE Hospitals, Hitech City, Hyderabad, with chief complaints of shortness of breath, cough, chest heaviness and mild neck pain for a month which had started to interfere with her daily activities.
Past Medical History
The patient had no history of chronic illnesses or drug allergies. The absence of comorbid conditions was considered clinically favourable, as it minimized the risk of intraoperative and postoperative complications and supported a smoother, more stable recovery.
On Examination
Upon admission to PACE hospitals, the patient was hemodynamically stable with stable vital signs. On cardiovascular examination, S1 and S2 heart sounds were present. Central nervous system examination revealed no focal neurological deficits. Respiratory system examination showed bilateral air entry with normal vesicular breath sounds. Abdominal examination revealed that the abdomen was soft and non-tender, with no evidence of organomegaly.
Diagnosis
After the initial examination, the patient underwent a comprehensive assessment by the oncology team, which included detailed clinical evaluation, laboratory investigations and imaging studies, including:
Ultrasonography: It was performed on the patient, revealing multiple nodules within the thyroid gland, which confirming the diagnosis of multinodular goiter.
Computed Tomography (CT) scan: It was subsequently conducted, which provided detailed imaging that showed the extent of the goiter, accurately defined the size and position of the thyroid nodules and demonstrated compression and displacement of the trachea.
Simple cervicothoracic radiography (X-ray): It was used as an initial screening tool in this patient and revealed evidence of tracheal compression.
Lung function tests: This includes flow-volume loops, which were performed due to the patient’s respiratory symptoms. These tests provided additional evidence that showed the presence of tracheal compression caused by the enlarged thyroid.
These radiographic findings correlated with the patient’s symptoms and confirmed the provisional diagnosis, guiding the team toward planning appropriate surgical intervention.
Based on the comprehensive evaluation, the patient was advised to undergo Multinodular goiter with tracheal compression treatment in Hyderabad, India, under the expert care of the Oncology Department to ensure complete management of her condition, symptom relief, and prevention of further complications.
Medical Decision Making
After consulting with the surgical oncologist, Dr. Ramesh Parimi, along with other consultants, Dr. Sashi Vardhan Janjirala and Dr. Pradeep Kiran Panchadi, a comprehensive evaluation was conducted to determine the appropriate course of treatment for the patient.
Their collective expertise led to the conclusion that total thyroidectomy would be the most appropriate surgical intervention for managing the bilateral thyroid space-occupying lesions, specifically the multinodular goiter. This decision was based on a thorough clinical assessment and aimed at ensuring optimal outcomes through timely and definitive treatment.
The patient and her family were counselled about the patient's condition, including the associated risks, complications, and benefits. They were also informed about the necessity of surgical intervention to prevent future complications and ensure optimal outcomes.
Surgical Procedure
Following the decision, the patient was scheduled to undergo Total thyroidectomy Surgery in Hyderabad at PACE Hospitals under the expert supervision of the Oncology Department.
The following steps were carried out during the procedure:
Preoperative preparation and anaesthesia: The patient was positioned supine with neck extended and general anaesthesia was administered with the airway secured; the patient’s neck and chest were cleaned and draped in a sterile manner.
Surgical exposure: A transverse incision was made in the lower neck to access the thyroid gland, likely for a thyroid-related condition (such as goiter, thyroid nodule, or cancer). Subplatysmal flaps were elevated, and the strap muscles were retracted to expose the thyroid gland. Dividing the midline fascia allowed direct visualization of the thyroid and trachea, facilitating safe and effective surgical management of the patient's thyroid pathology.
Thyroid gland mobilization: The thyroid lobe was gently mobilized, and the middle thyroid vein was identified, ligated, and divided to facilitate further exposure; the superior pole of the thyroid was dissected, and the superior thyroid vessels were ligated near the gland to minimize risk to the external branch of the superior laryngeal nerve.
Protection of vital structures: The superior parathyroid glands were preserved to prevent postoperative hypocalcaemia, and the inferior thyroid vessels were ligated near the gland to maintain parathyroid blood supply. The recurrent laryngeal nerve was carefully identified and protected throughout the procedure to avoid vocal cord paralysis, ensuring patient safety during thyroid surgery.
Gland Removal: The thyroid gland was carefully separated from the trachea, with meticulous control of vessels and division of the ligament of Berry. The procedure was repeated on the opposite side to achieve complete removal of the gland, as required for the patient's condition.
Haemostasis and closure: Haemostasis (bleeding control) was secured, and the wound was closed in layers, with a drain placed as needed, to minimise post-operative complications and promote optimal recovery for the patient.
Postoperative Care
After surgery, the patient's postoperative recovery was uneventful, and she was monitored closely in the surgical intensive care unit to ensure stability. She was transferred to the general ward once her condition was stable. During her hospital stay, she received intravenous antibiotics to prevent infection, analgesics for pain relief, antiemetics to control nausea, and gastric protectants.
Discharge Medications
Upon discharge, the patient was prescribed a comprehensive medication regimen to support postoperative recovery and minimize complications. This included antibiotics to reduce the risk of surgical site infection, proton pump inhibitors (PPIs) to prevent gastrointestinal irritation, a mucolytic agent to facilitate the clearance of respiratory secretions, and glucocorticoids to suppress immune responses.
Advice on Discharge
The patient was advised to follow a balanced diet tailored to her condition, emphasizing adequate intake of proteins, carbohydrates, healthy fats, vitamins, and minerals. The diet was intended to support recovery, maintain overall health, and prevent nutritional deficiencies.
Emergency Care
The patient was informed to contact the Emergency ward at PACE Hospitals in case of any emergency or development of symptoms such as fever, abdominal pain, and vomiting.
Review and Follow-Up
The patient was advised to schedule a follow-up appointment with the Oncologist in Hyderabad at PACE Hospitals one week after discharge. During this visit, the patient’s recovery was to be evaluated to determine the need for any further management.
Conclusion
This case highlights the effectiveness of total thyroidectomy in managing multinodular goiter with tracheal compression, demonstrating prompt relief of airway obstruction, significant improvement in respiratory function, and successful prevention of disease recurrence.
The crucial role of CT (computed tomography) in the evaluation and management of multinodular goiter with tracheal compression.
CT was crucial in evaluating and managing multinodular goiter with tracheal compression, as it provided an accurate assessment of the goiter's size, extent, and anatomical relationships, detected and quantified tracheal compression, and aided in preoperative planning. CT distinguished multinodular goiter from other neck masses or airway obstructions and guided Oncologist/cancer specialist decision-making by predicting postoperative improvement in symptoms. Overall, CT imaging was essential for a comprehensive evaluation, risk assessment, and surgical planning in patients with multinodular goiter and tracheal compression. Both CT scan and ultrasound were the most sensitive and informative tests for confirming the multinodular nature of the goiter and its compressive effect on the trachea.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868