What Is the Role of Gastroenterology in Digestive Health?
PACE Hospitals
Written by: Editorial Team
Medically reviewed by: Dr. Govind Verma - Interventional Gastroenterologist and Hepatologist
Understanding Gastroenterology and Its Importance
Gastroenterology focuses on diagnosing, preventing, and treating digestive system disorders to protect nutrition, immunity, and long-term gastrointestinal health.
Gastroenterology is an important and specialized branch of medicine dedicated to the diagnosis, treatment, and prevention of diseases affecting the digestive system. This medical specialty encompasses the entire gastrointestinal (GI) tract, from the mouth to the anus, including the esophagus, stomach, small intestine, large intestine (colon), liver, gallbladder, pancreas, and bile ducts.
The digestive system plays a pivotal role in overall health and well-being of an individual through processing nutrients, eliminating waste, and housing approximately 70% of the immune system. When gut health deteriorates, it can have an impact on almost every area of physical well-being, including nutrient absorption and mental health.
In India, digestive disorders represent a significant healthcare burden, with gastroenterological conditions accounting for nearly 20-30% of all medical consultations. The prevalence of conditions like inflammatory bowel disease, peptic ulcers, and liver diseases continues to rise, making gastroenterology an increasingly vital medical specialty.
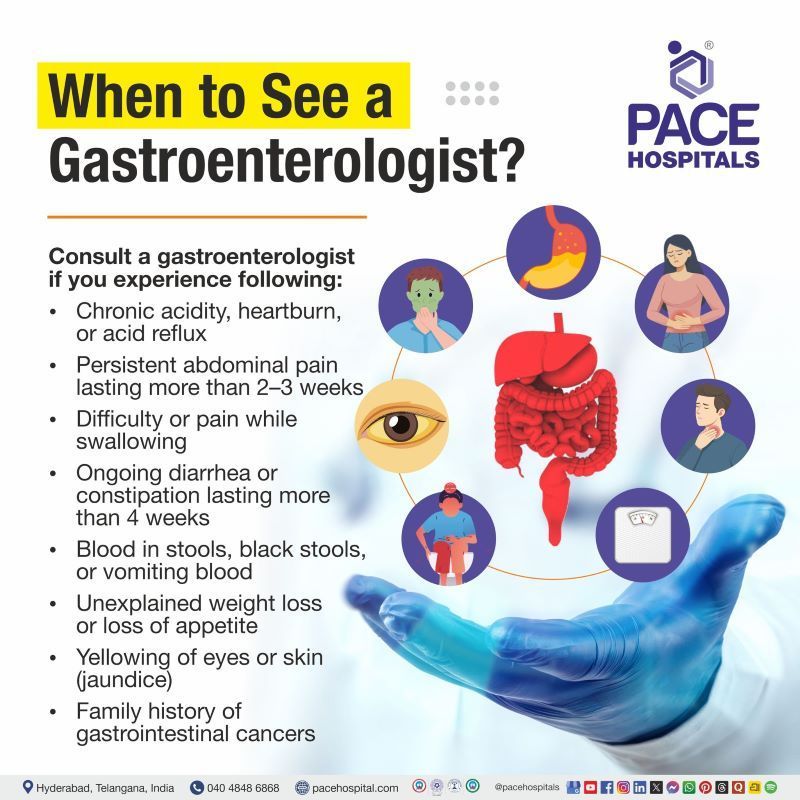
Quick Guide: When to See a Gastroenterologist?
Consult a gastroenterologist if you experience following:
- Chronic acidity, heartburn, or acid reflux
- Persistent abdominal pain lasting more than 2–3 weeks
- Difficulty or pain while swallowing
- Ongoing diarrhea or constipation lasting more than 4 weeks
- Blood in stools, black stools, or vomiting blood
- Unexplained weight loss or loss of appetite
- Yellowing of eyes or skin (jaundice)
- Family history of gastrointestinal cancers
Early specialist evaluation helps prevent complications and enables timely treatment.
The Comprehensive Scope of Gastroenterology
Organs and Systems Under Gastroenterological Care
Gastroenterologists specialize in managing conditions affecting:
Upper Digestive Tract:
- Esophagus: It is a hollow, fibromuscular tube connecting the throat to the stomach, commonly affected by Barrett's esophagus, acid reflux, and swallowing disorders
- Stomach: It is a large, muscular, and hollow organ responsible for holding food and it is the place where initial protein digestion occurs, susceptible to stomach (peptic) ulcers, gastritis, and functional disorders
- Duodenum: The first section of the small intestine, where most chemical digestion happens
Lower Digestive Tract:
- Small Intestine: It is responsible for nutrient absorption, can be affected by celiac disease, Crohn's disease, and bacterial overgrowth
- Large Intestine (Colon): Manages water absorption and waste formation, prone to inflammatory bowel disease, polyps, and diverticular disease
- Rectum and Anus: The terminal portions of the GI tract, where hemorrhoids (piles), fissures, and fistulas commonly develop
Accessory Digestive Organs:
- Pancreas: It is responsible to generate digestive enzymes and regulates blood sugar through insulin production
- Liver: It is the body's primary detoxification organ, filtering blood to neutralize toxins and producing bile for fat digestion
- Gallbladder: It is the GI organ responsible to store and concentrate bile from the liver, commonly affected by gallstones and inflammation
Pediatric Gastroenterology Care
Gastroenterologists also manage digestive conditions in children, teenagers, and adolescents. Common pediatric concerns include recurrent abdominal pain, food allergies, poor weight gain, chronic diarrhea, celiac disease, inflammatory bowel disease, liver disorders, and congenital digestive abnormalities. Early diagnosis in children is needed to ensure proper growth, nutrition, and long-term digestive health.
Digestive Health Concerns in Women
Women may experience unique and distinct digestive issues influenced by pregnancy, hormonal changes, and gynecological conditions. Some disorders such as irritable bowel syndrome (IBS), gallbladder disease, constipation, acid reflux during pregnancy, and functional bowel disorders are more common in women. Gastroenterologists often work closely with gynecologists to ensure accurate diagnosis and safe, coordinated care to rule out the complications.
Digestive Symptoms That Require Emergency Care
Seek immediate medical attention if you experience following signs:
- Severe abdominal pain with fever
- Persistent vomiting or inability to tolerate fluids
- Sudden or heavy rectal bleeding
- Black, tarry stools with dizziness or weakness
- Severe jaundice with confusion
- Abdominal pain accompanied by chest pain or breathlessness
- Prompt emergency evaluation can be lifesaving in these situations.
Common Digestive Conditions Managed by Gastroenterologists
Functional Digestive Disorders
Irritable Bowel Syndrome (IBS): Affecting an estimated 8-12% of India's population, IBS causes chronic abdominal pain, bloating, and altered bowel habits without visible structural damage. Gastroenterologists play an important and key role in determining and identifying triggers, recommending dietary changes, and developing comprehensive treatment plans in accordance to individuals.
Functional Dyspepsia: Characterized by persistent upper abdominal discomfort, early satiety, and bloating, this condition requires careful evaluation to rule out structural causes and implement effective lifestyle interventions so that affected individual can lead a comfortable life.
Inflammatory Digestive Diseases
Inflammatory Bowel Disease (IBD): Including Crohn's disease and ulcerative colitis, IBD involves chronic inflammation of the digestive tract. India has seen a rising incidence of IBD among its general population and particularly in urban city population, with prevalence rates increasing from 0.4 to 6.0 per 100,000 individuals over recent decades displaying it as a concern.
Gastroesophageal Reflux Disease (GERD): Extremely common in India, with prevalence rates of 7-22% in different regions, GERD occurs when stomach acid frequently flows back into the esophagus, causing heartburn and potential complications like esophagitis or Barrett's esophagus.
Liver and Pancreatic Conditions
Fatty Liver Disease: Non-alcoholic fatty liver disease (NAFLD) affects approximately 9-32% of the Indian population, with higher prevalence in urban areas. This condition can progress to cirrhosis if left unmanaged.
Chronic Pancreatitis: Particularly relevant in India where tropical pancreatitis is endemic in certain regions, this condition causes persistent pancreatic inflammation leading to digestive enzyme deficiency and pain.
Structural Abnormalities
Peptic Ulcer Disease: Affecting 5-10% of Indians at some point in their lives, peptic ulcers create painful sores in the stomach or duodenal lining, often associated with H. pylori infection or prolonged Nonsteroidal anti-inflammatory drugs (NSAIDs) use.
Polyps and Precancerous Lesions: Gastroenterologists identify and remove polyps during screening procedures, preventing their progression to colorectal cancer.
Advanced Diagnostic Capabilities in Gastroenterology
Endoscopic Procedures
Upper GI Endoscopy (Esophagogastroduodenoscopy - EGD): This procedure allows direct visualization of the upper digestive tract, enabling biopsies, treatment of bleeding sources, removal of polyps, and dilation of strictures. It is considered as the gold standard for diagnosing conditions affecting the esophagus, stomach, and duodenum.
Colonoscopy: The procedure is essential for colorectal cancer screening, colonoscopy examines the entire colon and rectum. In India, where colorectal cancer incidence is rising (representing 6-8% of all cancers), regular screening beginning at age 45-50 can significantly reduce mortality.
Flexible Sigmoidoscopy: Examining the lower portion of the colon, this procedure offers a less invasive alternative for specific indications, though it doesn't visualize the entire colon.
Capsule Endoscopy: This innovative technique uses a pill-sized camera to photograph the small intestine, areas traditionally difficult to examine. It's particularly useful for detecting obscure bleeding sources and small bowel Crohn's disease.
Specialized Diagnostic Techniques
Endoscopic Ultrasound (EUS): It is a minimally invasive procedure, combining endoscopy with ultrasound imaging, EUS provides detailed views of the digestive tract walls and surrounding structures, crucial for staging GI cancers detecting and evaluating pancreatic and biliary diseases.
ERCP (Endoscopic Retrograde Cholangiopancreatography): This advanced procedure combines endoscopy and fluoroscopy to diagnose and treat conditions of the bile ducts and pancreatic ducts, including gallstone removal and stent placement.
Manometry Studies: It involves measuring pressure and muscle contractions in the esophagus, stomach, or rectum helps diagnose motility disorders affecting swallowing and bowel function.
pH Monitoring:
This 24-hour test measures acid levels in the esophagus, definitively diagnosing GERD and assessing treatment effectiveness.
Laboratory and Imaging Studies
Gastroenterologists interpret various tests including:
- Complete blood counts to detect anemia condition arised from GI bleeding
- Liver function tests (LFT) to assess hepatic (liver) health
- Stool studies for infection, inflammation, and occult blood
- Breath tests for H. pylori and small intestinal bacterial overgrowth (SIBO)
- Imaging studies like CT enterography, MRI, and ultrasound
The Role of Gastroenterology in Preventive Healthcare
Cancer Screening and Early Detection
Colorectal Cancer Prevention: Colonoscopy remains the most effective colorectal cancer screening method, with the ability to detect and remove precancerous polyps before they develop into malignant form. Given India's increasing colorectal cancer rates, screening should begin at age 45 for average-risk individuals, or earlier for those with family history.
Esophageal Cancer Surveillance: For patients with Barrett's esophagus (a precancerous condition), regular endoscopic surveillance with biopsies enables early detection and intervention before cancer develops and becomes riskier.
Liver Cancer Screening: Patients with chronic liver disease, particularly cirrhosis, require regular ultrasound surveillance and blood tests (AFP levels) to detect hepatocellular carcinoma at treatable stages and eliminate future problem.
Lifestyle and Dietary Counseling
Gastroenterologists provide evidence-based guidance on:
- Alcohol consumption counseling to protect liver health
- Dietary modifications for conditions like Irritable Bowel Syndrome (IBS), celiac disease, and lactose intolerance
- Weight management strategies to prevent
- health issues such as fatty liver disease
- Smoking cessation to reduce cancer risk and improve healing process
Vaccination and Infection Prevention
Gastroenterologists recommend appropriate vaccinations including:
- Hepatitis A and B vaccines to prevent viral liver infections
- Pneumococcal and influenza vaccines for patients with chronic liver disease
- Preventive strategies against H. pylori infection
Therapeutic Interventions Performed by Gastroenterologists
Endoscopic Treatments
Polyp Removal (Polypectomy): Removing polyps during colonoscopy prevents colorectal cancer development, with advanced techniques allowing removal of large polyps that previously required surgery.
Variceal Band Ligation: For patients with liver cirrhosis and esophageal varices (enlarged veins prone to life-threatening bleeding), gastroenterologists place bands to prevent or control bleeding episodes.
Endoscopic Mucosal Resection (EMR) and Endoscopic Submucosal Dissection (ESD): These advanced techniques remove early-stage cancers and large precancerous lesions in the gastrointestinal (GI) tract without need of surgery, preserving organ function and reducing recovery time.
Stricture Dilation: Narrowed areas in the esophagus or colon can be dilated endoscopically, restoring normal function and alleviating swallowing difficulties or bowel obstruction.
Stent Placement: Metallic or plastic stents can be placed to maintain open passages in the esophagus, bile ducts, or colon when strictures cannot be permanently resolved in conditions such as inoperable malignant common bile duct strictures.
Bleeding Control: Gastroenterologists use various endoscopic techniques including clips, cauterization, and injection therapy to stop GI bleeding from ulcers, vascular malformations, or other sources.
Nutritional Support
For patients unable to eat normally, gastroenterologists place:
- Percutaneous Endoscopic Gastrostomy (PEG) tubes: Providing direct access to the stomach for long-term feeding
- Nasogastric tubes: Offering necessary temporary nutritional support for the patients incapable of consuming calories orally
When to Consult a Gastroenterologist?
Persistent Digestive Symptoms Requiring Specialist Evaluation
Chronic Abdominal Pain: If pain lasting more than 3 months, recurrent pain episodes, or pain accompanied by warning signs (bleeding, weight loss, fever) requires prompt gastroenterological evaluation to identify underlying causes.
Altered Bowel Habits: Persistent diarrhea (lasting beyond 4 weeks), chronic constipation, or sudden changes in bowel patterns, particularly after age 45, require investigation to rule out serious conditions.
Difficulty Swallowing (Dysphagia): Any persistent trouble swallowing solid foods or liquids demands prompt assesment, as it may indicate strictures, motility disorders, or malignancy.
Unexplained Weight Loss: If having unintentional weight loss exceeding 5% of body weight within 6 months, especially with digestive symptoms, requires comprehensive gastroenterological assessment and consideration.
Gastrointestinal Bleeding: Blood in vomit (hematemesis), black tarry stools (melena), or bright red rectal bleeding (hematochezia) necessitates urgent gastroenterological consultation.
Screening and Surveillance Indications
Age-Appropriate Cancer Screening:
- Individuals aged 45-50 and above should undergo colorectal cancer screening via colonoscopy
- Those with family history of GI cancers should begin screening 10 years before the youngest affected relative's diagnosis age
High-Risk Populations:
- Patients with chronic hepatitis B or C require regular liver monitoring
- Individuals with inflammatory bowel disease need surveillance colonoscopies
- Those with Barrett's esophagus require periodic endoscopic evaluation
Abnormal Test Results: Abnormal liver function tests, positive stool occult blood tests, or concerning imaging findings necessitate gastroenterological follow-up.
Gastroenterology in the Indian Healthcare Context
Gastroenterology in India is influenced by a combination of infectious illnesses, changing lifestyles, dietary habits, and differences in healthcare access, which affect how digestive disorders are diagnosed, treated, and prevented nationwide.
Together, these factors result in distinct disease trends, unequal access to care, and persistent gaps in preventive awareness, as described below.
Unique Epidemiological Patterns
Infectious Causes: India has higher rates of infectious gastroenteritis, including:
- Helicobacter pylori infection affecting 50-70% of the population as a whole
- Tropical pancreatitis occurring predominantly in southern states of India
- Hepatitis A and E being endemic in many regions
- Tuberculosis affecting the intestinal tract in immunocompromised patients
Dietary Factors: Traditional Indian diets, while often healthy, can contribute to specific conditions:
- High-carbohydrate diets potentially increasing fatty liver disease risk in individuals completely depending on high-carb
- Spicy foods possibly exacerbating Gastroesophageal reflux disease (GERD) and peptic ulcers in susceptible individuals
- Regional dietary variations affecting disease prevalence patterns
Rising Lifestyle Diseases: Urbanization and lifestyle changes have increased rates of:
- Obesity-related digestive conditions
- Non-alcoholic fatty liver disease, particularly in metropolitan areas
- Inflammatory bowel disease showing rising incidence
Access and Cost Considerations
Diagnostic Procedure Costs in India:
- Upper GI endoscopy: Usually the cost ranges from ₹2,000- ₹8,000 (approx.) in government facilities; ₹5,000- ₹20,000 in private hospitals/organizations
- Colonoscopy: Usually the cost ranges from ₹3,000- ₹10,000 (approx.) in government settings; ₹8,000- ₹30,000 privately settings
- Advanced procedures like ERCP: The cost is higher around ₹15,000- ₹80,000 (approx.) depending on facility and complexity
Healthcare Accessibility: While major cities in urban areas have excellent gastroenterological services, rural areas face significant challenges and shortcomings in medical services:
- Limited highly experienced gastroenterology specialists availability in tier-2 and tier-3 cities
- Delayed diagnosis due to lack of endoscopic facilities
- Growing telemedicine initiatives helping bridge consultation gaps
Preventive Healthcare Awareness
Despite increasing awareness, significant gaps remain:
- Low colorectal cancer screening rates compared to Western countries
- Limited public knowledge about liver disease and about its prevention
- Need for enhanced education about warning signs requiring specialists’ consultation
The Multidisciplinary Approach in Gastroenterology
Collaboration with Other Specialties
Surgical Coordination: Gastroenterologists work closely with general and GI surgeons, managing patients conservatively when possible and coordinating surgical intervention when necessary for conditions like cancer, complicated inflammatory bowel disease, or acute complications.
Nutritionist Partnership: Dietary management forms a cornerstone of treating many digestive disorders. Gastroenterologists collaborate with other department specialist such as clinical nutritionists to create personalized nutrition plans for conditions ranging from celiac disease to IBD to liver cirrhosis.
Oncology Integration: For GI malignancies, gastroenterologists participate in multidisciplinary tumor boards association, providing diagnostic expertise, performing staging procedures, and managing treatment-related complications in an effective way.
Radiology Collaboration: Interpreting complex imaging studies and planning interventional procedures requires close radiologist-gastroenterologist collaboration, particularly for advanced techniques like Endoscopic Ultrasonography (EUS) and Endoscopic Retrograde Cholangiopancreatography (ERCP) brings better outcomes.
Primary Care Coordination: Effective gastroenterological care requires prompt ongoing communication with primary care physicians who monitor chronic conditions and recognize when specialist consultation becomes topmost priority.
The Future of Gastroenterology in Digestive Health
Emerging Technologies
Artificial Intelligence Integration: AI-assisted endoscopy improves polyp detection rates, potentially revolutionizing colorectal cancer prevention with a futuristic approach. Machine learning algorithms analyze endoscopic images in real-time, highlighting suspicious lesions and improving diagnostic accuracy in an effective manner encompassing advancement of future technology.
Advanced Imaging: High-definition endoscopy, narrow-band imaging, and confocal laser endomicroscopy provide unprecedented detail, enabling "optical biopsies" and more precise targeting of abnormal tissue of GI system.
Minimally Invasive Approaches: Endoscopic sleeve gastroplasty,
peroral endoscopic myotomy (POEM), and other innovative techniques offer surgical-level results through endoscopic approaches, reducing recovery time and complications to help out both gastroenterologists and patients for better outcomes in treatment.
Personalized Medicine
Microbiome Research: Understanding the gut microbiome's role in health and disease opens new therapeutic strategies:
- Fecal microbiota transplantation for recurrent C. difficile infection
- Microbiome-based diagnostics for various GI conditions
- Probiotic and prebiotic interventions tailored to individual microbiome composition
Genetic Testing: Identifying genetic predispositions helps:
- Guide treatment selection in inflammatory bowel disease (IBD)
- Determine cancer risk and appropriate screening intervals
- Predict medication responses and side effects
Precision Treatment: Moving beyond one-size-fits-all approaches, gastroenterology increasingly uses biomarkers, genetic profiles, and disease characteristics to select optimal therapies for individual patients.
Maintaining Digestive Health: The Gastroenterologist's Recommendations
Dietary Strategies
Fiber Intake: Consuming 25-35 grams of dietary fiber daily supports bowel regularity, feeds beneficial gut bacteria, and reduces colorectal cancer risk in some individuals. Food sources include vegetables, whole grains, fruits, and legumes.
Hydration: Adequate water intake (8-10 glasses daily) facilitates digestion, prevents constipation, and supports overall GI function in a better way.
Mindful Eating: Chewing thoroughly, eating slowly, and avoiding large meals before bedtime improves digestion and reduces acid reflux symptoms in individual.
Identifying Triggers: Keeping a food diary and maintaining it helps identify personal triggers for conditions like IBS, allowing targeted dietary modifications rather than restrictive elimination diets.
Lifestyle Modifications
Regular Physical Activity: Exercise helps healthy bowel function, supports weight management, and reduces risk of digestive diseases including colon cancer and fatty liver disease.
Stress Management: The gut-brain connection means stress significantly impacts digestive health. Some healing techniques like yoga, meditation, and adequate sleep improve GI symptoms, particularly in functional disorders.
Limiting Harmful Substances:
- Alcohol limitation protects liver health and reduces esophageal cancer risk
- Avoiding tobacco products decreases risk of multiple GI cancers
- Limiting Nonsteroidal anti-inflammatory drugs (NSAIDs) use prevents peptic ulcers and small intestinal damage
Proactive Health Monitoring
Regular Check-ups: Annual primary care visits should include discussion of digestive symptoms with gastroenterologists and age-appropriate screening recommendations.
Responding to Warning Signs: Never ignoring persistent symptoms like difficulty swallowing, blood in stool, unexplained weight loss, or chronic abdominal pain ensures early detection of serious conditions to eliminate future risks.
Family History Awareness: Understanding family history of GI conditions guides screening timing and frequency, particularly for hereditary conditions like familial adenomatous polyposis or Lynch syndrome.
Gastroenterology Care at PACE Hospitals
PACE Hospitals offers comprehensive gastroenterology treatment and care focused on accurate diagnosis, early intervention, and long-term digestive health. Our approach combines clinical expertise, advanced diagnostics, and coordinated gastroenterology specialists care to manage the full spectrum of digestive system disorders.
Experienced Gastroenterology Specialists
Our gastroenterologists are trained in managing complex conditions of the esophagus, stomach, intestines, liver, pancreas, and biliary system. From common digestive complaints to advanced gastrointestinal and liver diseases, our specialists provide evidence-based, patient-focused care.
Advanced Endoscopy and Diagnostic Services
PACE Hospitals is equipped with latest, advanced endoscopic and imaging facilities that enable precise evaluation of digestive disorders. Procedures such as upper endoscopy, colonoscopy, advanced imaging-guided evaluations, and functional testing are performed with a strong focus on safety, accuracy, and patient comfort.
Comprehensive Care for Liver, Pancreatic, and Bowel Disorders
We provide integrated care for conditions such as fatty liver disease, chronic liver disorders, inflammatory bowel disease, gastrointestinal bleeding, and pancreatic conditions. Early detection and continuous monitoring help prevent complications and disease progression.
Preventive Gastroenterology and Cancer Screening
PACE Hospitals emphasizes preventive care through structured screening programs for colorectal cancer, liver disease surveillance, and early detection of precancerous conditions. Preventive gastroenterology plays an important and key role in reducing long-term disease burden and improving outcomes.
Multidisciplinary Approach for Complex Conditions
Digestive diseases often involve multiple organ systems. Our gastroenterologists work closely with well-renowned GI surgeons, oncologists, radiologists, nutritionists, anesthesiologists, and critical care teams to deliver coordinated and seamless care.
Patient-Centered and Ethical Care
We prioritize patient education, transparent communication, and ethical medical practices. Each care plan is tailored in accordance with individual needs, ensuring informed decision-making and active patient participation throughout the treatment journey to find better outcomes.
Focus on Comfort, Safety, and Recovery
All diagnostic and therapeutic procedures are performed following strict safety protocols, with careful consideration and attention to patient comfort, recovery, and follow-up care. Our goal is to deliver effective treatment while minimizing disruption to daily life.
Frequently Asked Questions on Gastroenterology & Digestive Health
Whom to consult for Digestive Problems?
General Physician: Initial evaluation of mild or short-term digestive symptoms
Gastroenterologist: Need to be consulted as they are Specialist for persistent, complex, inflammatory, liver, pancreatic, or bowel disorders and all endoscopic procedures
Gastrointestinal Surgeon: Required when surgical intervention is needed for cancers, obstruction, perforation, or advanced complications
Most patients benefit from early gastroenterologist involvement, which reduces delayed diagnosis and prevents disease progression.
What is the difference between a gastroenterologist and a general physician?
Although a general physician (MBBS with MD in General Medicine) provides comprehensive primary care for various medical conditions, while a gastroenterologist is a specialist who has completed additional 2-3 years of fellowship training specifically in digestive system diseases.
A gastroenterologists perform specialized diagnostic procedures like endoscopy and colonoscopy, interpret complex GI test results, and manage complicated digestive disorders and related digestive problems that require advanced expertise. For simple digestive issues like occasional heartburn or mild constipation, a general physician is appropriate, but persistent symptoms, abnormal test results, or conditions requiring endoscopic procedures necessitate highly experienced gastroenterological consultation and guidance.
Can digestive problems affect my overall health and immunity?
Yes, digestive health profoundly impacts overall wellbeing. The gut contains approximately 70% of the immune system, so digestive disorders can compromise immune function.
Certain conditions like inflammatory bowel disease, celiac disease, or chronic malabsorption prevent proper nutrient absorption, leading to deficiencies in vitamins (B12, D, K), minerals (iron, calcium, zinc), and proteins essential for immune function.
The gut microbiome—trillions of beneficial bacteria in the digestive tract—influences several mechanisms such as metabolism, mood, inflammation levels, and disease resistance. Disrupted gut health contributes to systemic inflammation linked to conditions beyond the digestive system, including arthritis, skin problems, and mental health disorders through the gut-brain axis.
What are the warning signs that I should see a gastroenterologist immediately?
Seek immediate gastroenterological consultation for: vomiting blood or coffee-ground material, passing black tarry stools or large amounts of bright red blood rectally, severe abdominal pain especially with difficulty swallowing or sensation of food getting stuck, fever or vomiting, unexplained weight loss exceeding 5% of body weight within 6 months, persistent vomiting preventing fluid intake, jaundice (yellowing of eyes or skin), or sudden changes in bowel habits after age 45.
Additionally, consult an experienced and well-renowned gastroenterologist within 1-2 weeks if you experience chronic heartburn not relieved by antacids, persistent abdominal pain lasting beyond 2 weeks, ongoing diarrhea exceeding 4 weeks, new onset constipation with bloating, or family history of GI cancers combined with concerning symptoms.
Can stress and anxiety cause real digestive problems?
Absolutely. The gut-brain axis—a bidirectional communication network between the digestive system and brain—means stress and anxiety directly impact digestive function. Stress triggers the release of hormones and neurotransmitters that alter gut motility, increase intestinal sensitivity, change digestive secretions, and disrupt the gut microbiome.
This explains why anxiety commonly causes or worsens symptoms like diarrhea, constipation, nausea, abdominal pain, and bloating. Functional disorders like irritable bowel syndrome demonstrate strong stress-symptom correlations. Chronic stress may also increase risk of inflammatory conditions and impair healing of existing digestive diseases.
In addition to medical treatment, stress management approaches such as meditation, cognitive behavioral therapy, yoga, and appropriate sleep can greatly alleviate stomach problems.
How is fatty liver disease diagnosed and managed without medications?
Fatty liver disease is typically discovered through routine ultrasound examinations or abnormal liver function tests. Diagnosis is confirmed through imaging (ultrasound, CT, or MRI showing fat accumulation in the liver) and exclusion of other liver diseases.
FibroScan—a specialized ultrasound technique—can assess both fat content and liver stiffness (indicating fibrosis). Lifestyle modification forms the cornerstone of non-alcoholic fatty liver disease management: A steady weight loss of 7-10% through balanced calorie reduction and increased physical exercise has a substantial impact on liver function.
Aim for 150 minutes of moderate-intensity exercise weekly. Need to follow a Mediterranean-style diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting refined carbohydrates, added sugars, and saturated fats. Avoid alcohol completely. Disease progression or improvement is tracked through regular monitoring using blood tests and imaging.
What dietary changes help manage acid reflux and GERD naturally?
Diet and eating habits play a major role in controlling acid reflux and GERD symptoms. Eating smaller, more frequent meals in intervals helps reduce pressure on the stomach and lowers the chance of acid flowing back into the esophagus. It is required to keep in mind to not go for lying down for at least 2–3 hours after meals and to stay upright after eating.
Identifying and avoiding individual trigger foods is an important point to consider, as triggers vary from person to person. Common triggers include citrus fruits, spicy foods, tomatoes, chocolate, mint, caffeine, fried or fatty foods, and carbonated beverages. Maintaining a healthy body weight is especially important, as excess abdominal fat enhances pressure on the stomach and worsens reflux.
Additional helpful practices include eating slowly, chewing food thoroughly, stopping meals well before bedtime, and limiting alcohol intake. Elevating the head end of the bed by 6–8 inches using blocks can significantly reduce nighttime reflux. Keeping a food diary helps recognize personal triggers and patterns. Some individuals find relief with foods that are gentle on digestion, such as melons, bananas, oatmeal, ginger, and green vegetables. It is required to avoid tight clothing around the abdomen also helps reduce pressure that can aggravate reflux symptoms.
How do I choose between different types of gastroenterological procedures?
The choice of a gastroenterological procedure depends on an individual symptom, medical history, age, and the part of the digestive system that needs evaluation. The gastroenterologist recommends the most appropriate test after a detailed clinical assessment to ensure accurate diagnosis while minimizing risk.
Upper endoscopy is used to examine and visualize the esophagus, stomach, and upper small intestine and is commonly advised for symptoms such as upper abdominal pain, persistent heartburn, difficulty swallowing, nausea, or suspected ulcers. Colonoscopy allows complete evaluation of the colon and rectum and is essential for colorectal cancer screening, unexplained rectal bleeding, chronic diarrhea, and assessment of inflammatory bowel disease. Flexible sigmoidoscopy examines only the lower part of the colon and may be suitable for limited evaluation but does not replace full colon cancer screening.
Capsule endoscopy is a specialized, non-invasive diagnostic treatment that visualizes the small intestine when traditional endoscopic tests fail to identify the cause of symptoms, such as unexplained bleeding. Procedures focused on the bile ducts and pancreas are recommended for conditions like suspected jaundice, gallstone disease, or pancreatic disorders. Advanced techniques that combine endoscopy with imaging provide detailed assessment of deeper tissues and are particularly valuable for cancer evaluation and staging.
Your gastroenterologist will explain the purpose, benefits, limitations, and potential risks of each procedure and guide you toward the option best suited to your individual clinical needs.
How often should I get a colonoscopy for colon cancer screening?
For average-risk individuals in India, colonoscopy screening should begin at age 45-50 or nearby age group or above and need to be repeated every 10 years if results are normal. If polyps are found during screening, follow-up intervals range from 3-5 years depending on polyp size, number, and characteristics.
High-risk individuals with family history of colorectal cancer should begin screening 10 years before the age at which their youngest affected relative was diagnosed, or at age 40, whichever comes first. Those with inflammatory bowel disease require more frequent surveillance colonoscopies beginning 8-10 years after diagnosis, typically every 1-3 years depending on disease activity and other risk factors.
Is endoscopy painful, and how should I prepare for it?
Modern endoscopic procedures are performed under conscious sedation or general anesthesia, making them painless. You'll feel drowsy and relaxed, with no memory of the procedure afterward.
Preparation varies by procedure type: for upper endoscopy, you must fast for 6-8 hours beforehand to ensure an empty stomach. Colonoscopy requires thorough bowel cleansing using prescribed laxative solutions taken the evening before and morning of the procedure, along with a clear liquid diet for 24 hours prior.
After either procedure, you'll need someone to drive you home due to sedation effects. Most patients resume normal activities the next day. Serious complications are rare (occurring in less than 0.1% of procedures), but your gastroenterologist will discuss specific risks based on your health status.
What is H. pylori infection and why is it important?
Helicobacter pylori is a gram-negative bacterium that infects the stomach lining and duodenum, affecting 50-70% of India's population. While many people carry H. pylori without having any symptoms, it's the primary cause of peptic ulcers (stomach ulcers) and significantly increases stomach cancer risk.
The infection spreads through contaminated food, water, or close contact with infected individuals. Testing for H. pylori is recommended when a person have persistent upper abdominal pain, recurrent ulcers, or family history of stomach cancer. Diagnosis involves breath tests, stool antigen tests, or biopsies during endoscopy.
Treatment involves a combination of medication using antibiotics and acid-suppressing therapy for 10-14 days, with success rates exceeding 85%. Eradicating H. pylori heals most stomach ulcers, reduces cancer risk, and often resolves chronic gastritis symptoms.
When does constipation require medical evaluation rather than just dietary changes?
Seeking medical evaluation and consultation with an experienced gastroenterologist becomes utmost necessary if constipation continues despite increasing fiber, fluids, and exercise; you experience constipation after age 45 with no prior history; you see blood in stools; you have unexplained weight loss; constipation alternates with diarrhea; you experience severe abdominal pain or bloating; you notice pencil-thin stools; or you have a family history of colon cancer or inflammatory bowel disease.
Additionally, consult a gastroenterologist if you depend on laxatives regularly to have bowel movements, have symptoms of bowel obstruction (severe cramping, inability to pass gas, vomiting), notice new onset constipation after starting medications, or experience constipation accompanied by neurological symptoms. Chronic constipation lasting months may indicate underlying conditions requiring specialized testing like colonoscopy, transit studies, or anorectal manometry.
What is the gut microbiome and how does it affect my health?
The gut microbiome is a vast community of trillions of microorganisms, mainly bacteria, living in the digestive tract, especially the colon. This internal ecosystem plays a vital role in overall health by helping digest food, producing essential vitamins, breaking down dietary fiber, supporting immune function, and also protecting against harmful microbes attacks. It also communicates with the brain through the gut–brain axis, influencing mood, stress responses, and cognitive health.
When the balance of the gut microbiome is disturbed, a state known as dysbiosis, it can contribute to digestive disorders and broader health problems, including inflammatory bowel disease, irritable bowel syndrome, metabolic conditions, allergies, and mental health issues.
A diversified, fiber-rich diet that includes fruits, vegetables, whole grains, legumes, and naturally fermented foods promotes a healthy microbiome for gut health. Doing regular physical activity, appropriate sleep, stress management, limiting processed foods and added sugars, and avoiding unneeded antibiotic use all help to maintain a healthy and strong gut flora.
What is inflammatory bowel disease and how is it different from irritable bowel syndrome?
Inflammatory bowel disease (IBD) includes Crohn's disease and ulcerative colitis, chronic autoimmune conditions causing visible inflammation and damage to the intestinal lining, identifiable through endoscopy and biopsies. IBD can cause serious complications including strictures, fistulas, perforation, and increased cancer risk, requiring long-term management.
Irritable bowel syndrome (IBS) is a functional disorder causing similar symptoms (abdominal pain, diarrhea, constipation, bloating) but without visible inflammation or structural damage on endoscopy, diagnosed based on symptom patterns and exclusion of other conditions.
IBD typically presents with bloody diarrhea, weight loss, fever, and anemia, while IBS rarely causes these warning signs. IBD treatment focuses on controlling inflammation and preventing complications through different therapeutic approaches, while IBS management emphasizes primarily on symptom relief through dietary modifications, stress management, and lifestyle changes to have better result. Despite different underlying mechanisms, both conditions significantly impact quality of life and require appropriate diagnosis and management.
How accurate are stool tests for detecting colon cancer compared to colonoscopy?
Stool-based screening tests look for hidden blood or abnormal genetic material shed into the stool by colorectal cancers or large polyps. These tests are non-invasive and convenient, making them useful screening options for some individuals. However, they are less sensitive than colonoscopy, especially for detecting precancerous polyps.
A positive stool test always requires a follow-up colonoscopy to confirm the diagnosis and identify the source of abnormal findings. Colonoscopy is considered the gold standard for colorectal cancer screening because it allows direct visualization of the entire colon and enables removal of precancerous polyps during the same procedure, thereby preventing cancer from developing.
Stool-based tests need to be repeated at regular intervals, while a normal colonoscopy offers long-term reassurance for many years. For individuals who are unable or unwilling to undergo colonoscopy, stool tests provide an alternative way to find out the reason for the issue. The choice between screening methods should be made in consultation with an experienced gastroenterologist, based on individual risk factors, preferences, and overall health.
Can liver disease be reversed if caught early?
When discovered in early condition and treated properly, many types of liver disease can be improved or even reversed. In the early stages, liver damage is often caused by inflammation, fat accumulation, or ongoing injury, and the liver has a strong capacity to heal once the underlying cause is addressed. Lifestyle changes such as weight reduction, balanced nutrition, regular physical activity, and complete avoidance of alcohol can lead to significant recovery of liver health in many individuals.
Certain liver conditions caused by infections or metabolic factors can be effectively controlled when identified early, preventing further damage and long-term complications. However, once advanced scarring of the liver, known as cirrhosis, develops, reversal becomes much more difficult, but disease development can be slowed and partial improvement may be achievable with proper treatment.
This emphasizes the importance of early detection through routine health check-ups and focused screening for high-risk persons with pre-existing health issues such as diabetes, obesity, long-term alcohol use, or any serious chronic liver disease. Regular monitoring with blood tests and imaging allows early intervention, helping prevent progression to more liver related issues such as
liver failure or
liver cancer.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles











