Slipped Disc Symptoms, Causes and Treatment | Disc Prolapse Treatment
PACE Hospitals
What is a slipped disc or disc prolapse?
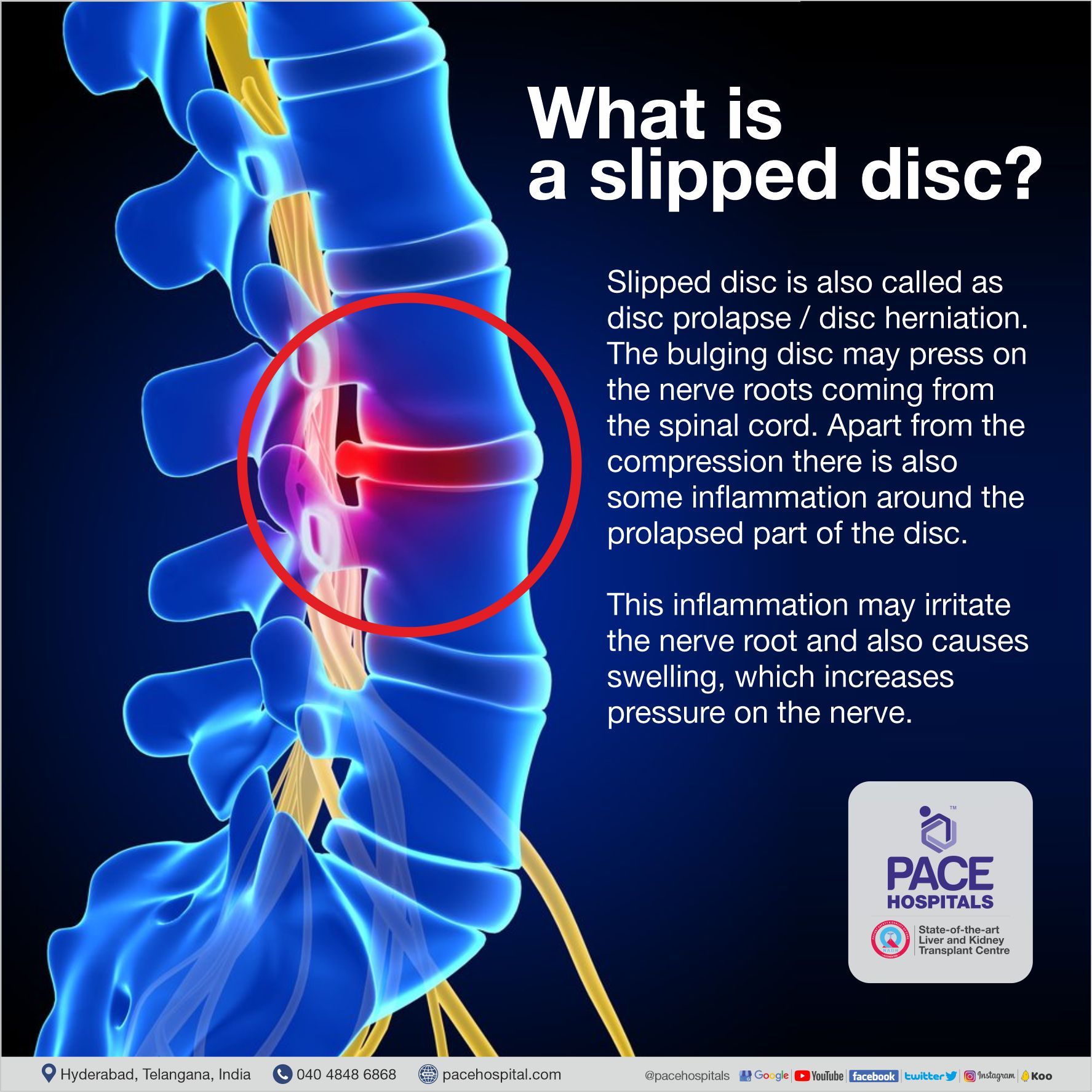
The disc does not actually slip when you have a slipped disc. The nucleus pulposus (the inner, softer portion of the disc) bulges out as a result of a weakness in the outer part of the disc. Slipped disc is also called as disc prolapse/disc herniation. The bulging disc may press on the nerve roots coming from the spinal cord. Apart from the compression, there is also some inflammation around the prolapsed part of the disc. This inflammation may irritate the nerve root and also causes swelling, which increases pressure on the nerve.
Disc prolapse can occur anywhere in your spine. However, most commonly seen in the discs of lower back (the lumbar spine) followed by the neck (Cervical region) and rarely in the thoracic spine. In the lumbar region, L4-L5 and L5-S1 levels are more commonly affected. The size of the prolapse can vary. In general, the larger the disc prolapse, the more severe the symptoms.
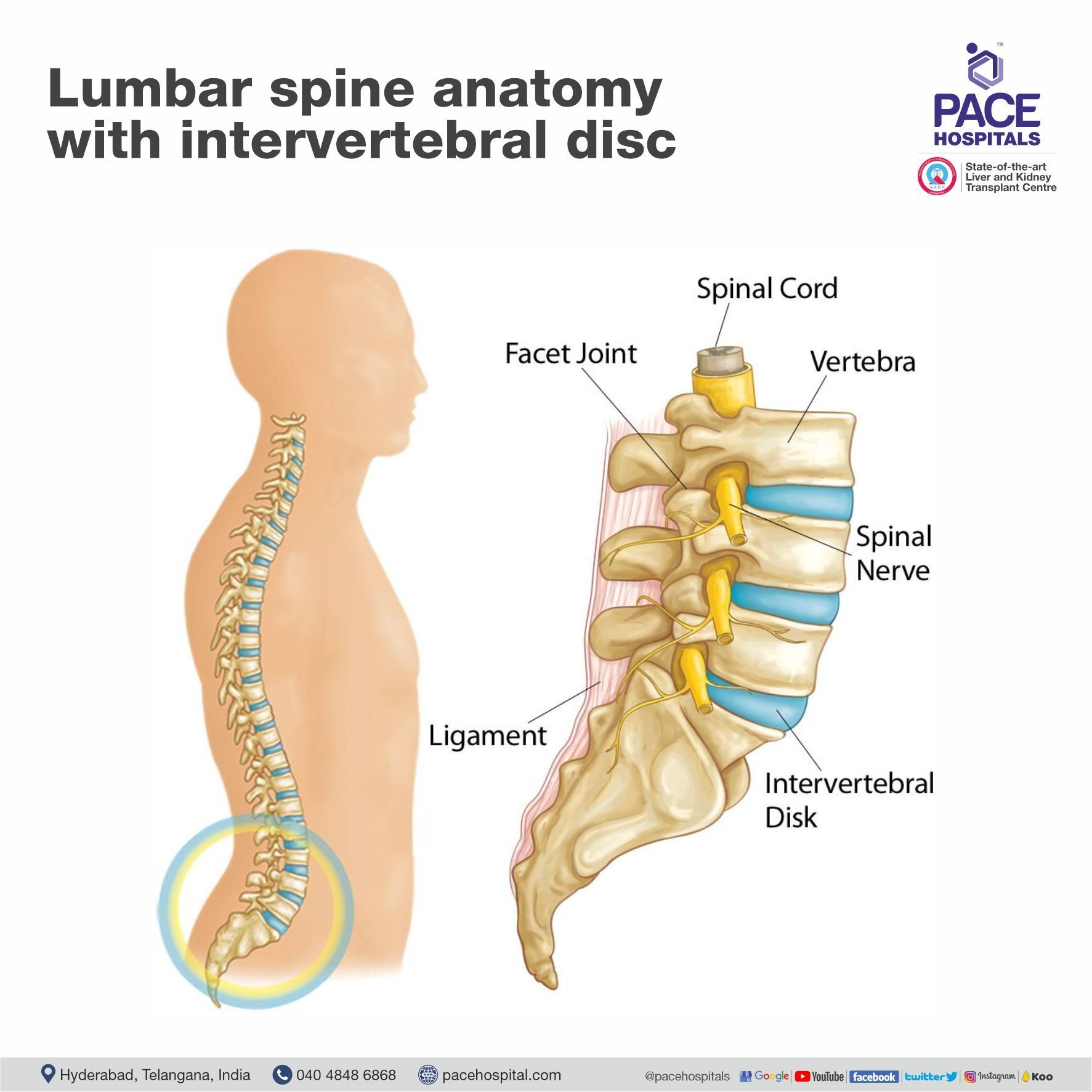
The spine is made up of many brick like bones called vertebrae that are stacked upon each other. In between each vertebra is a disc. The discs are made of strong rubber-like tissue, which allows the spine to be fairly flexible. A disc has a stronger fibrous outer part called the annulus fibrosus, and a softer jelly-like middle part called the nucleus pulposus.
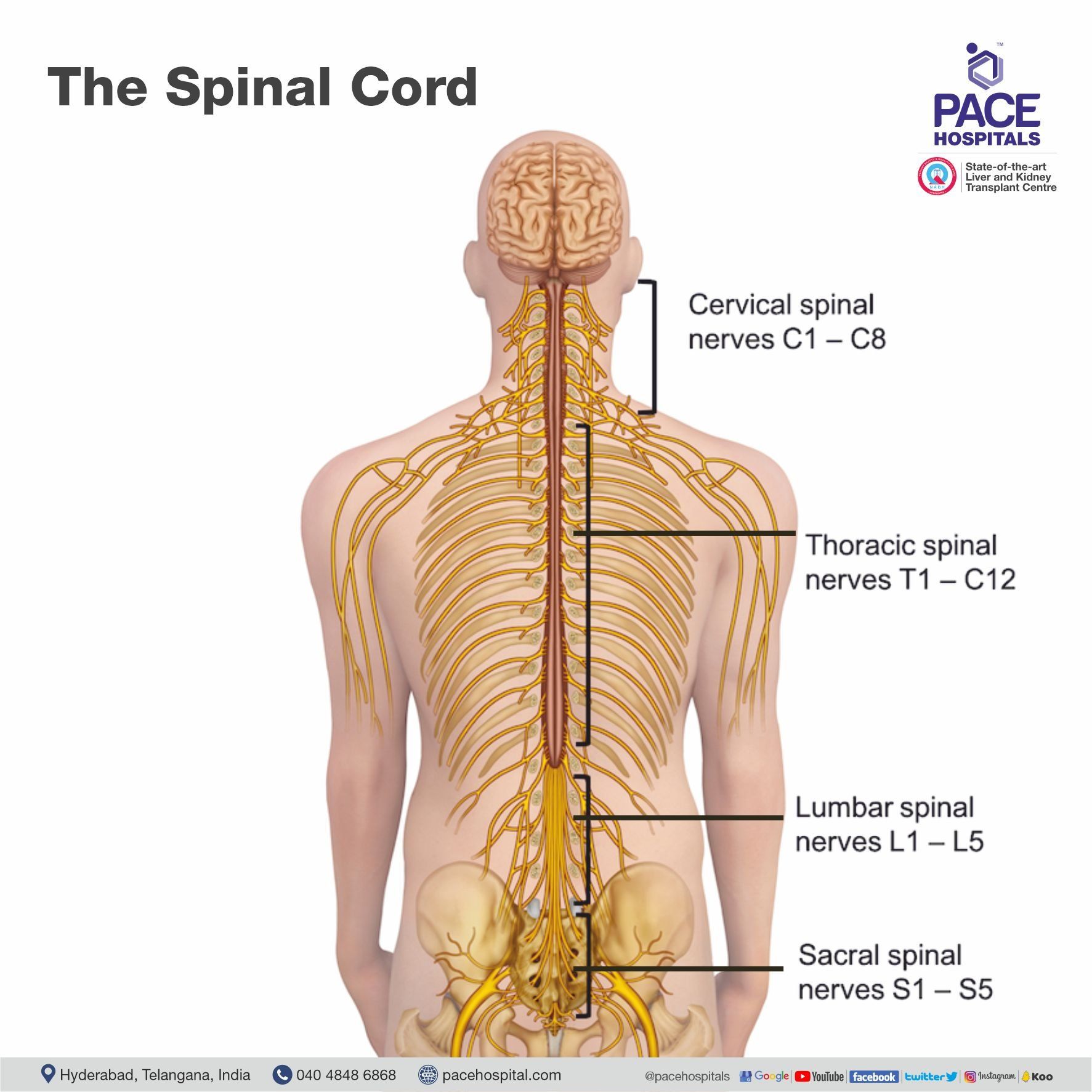
The spinal cord contains the nerves that come from the brain. It is protected by the spine. Nerves from the spinal cord come out from between the vertebrae to carry messages to and from various parts of the body. When you have a prolapsed disc, the inner softer part of the disc (the nucleus pulposus) bulges out and can press on nearby structures such as a nerve coming from the spinal cord
Who gets a a slipped disc or disc prolapse?
Acute Low back pain is very common. However, fewer than 1 in 20 cases of sudden-onset (acute) back pain are due to a slipped disc.
The most common age to develop a prolapsed disc is between 30 and 50 years. It is more common in the males than females. Disc prolapse is rare in people under 20 years of age.
What causes a slipped disc or disc prolapse?
It is not clear why some people develop disc prolapse and not others, even when they do the same job or lift the same sort of objects. Probably these people may have a weakness in the outer part of the affected disc. Activities that suddenly increase the intra-abdominal pressure such as sneezing, awkward bending, or heavy lifting in an awkward position may cause extra pressure on the disc, allowing the inner softer part of the disc to squeeze out through the weakened outer part of the disc.
Who are at risk of developing a slipped disc or disc prolapse?
Factors that may increase the risk of developing a prolapsed disc include:
- A job involving lots of lifting
- A job involving lots of sitting (especially driving)
- Weight-bearing sports (weightlifting etc)
- Smoking
- Being overweight (obesity)
- Increasing age (a disc is more likely to develop a weakness as we become older)
Symptoms of a slipped disc or disc prolapse
Back pain
The pain is often severe and usually comes on suddenly. The pain is usually eased by lying still and is often made worse if you move your back, cough or sneeze.
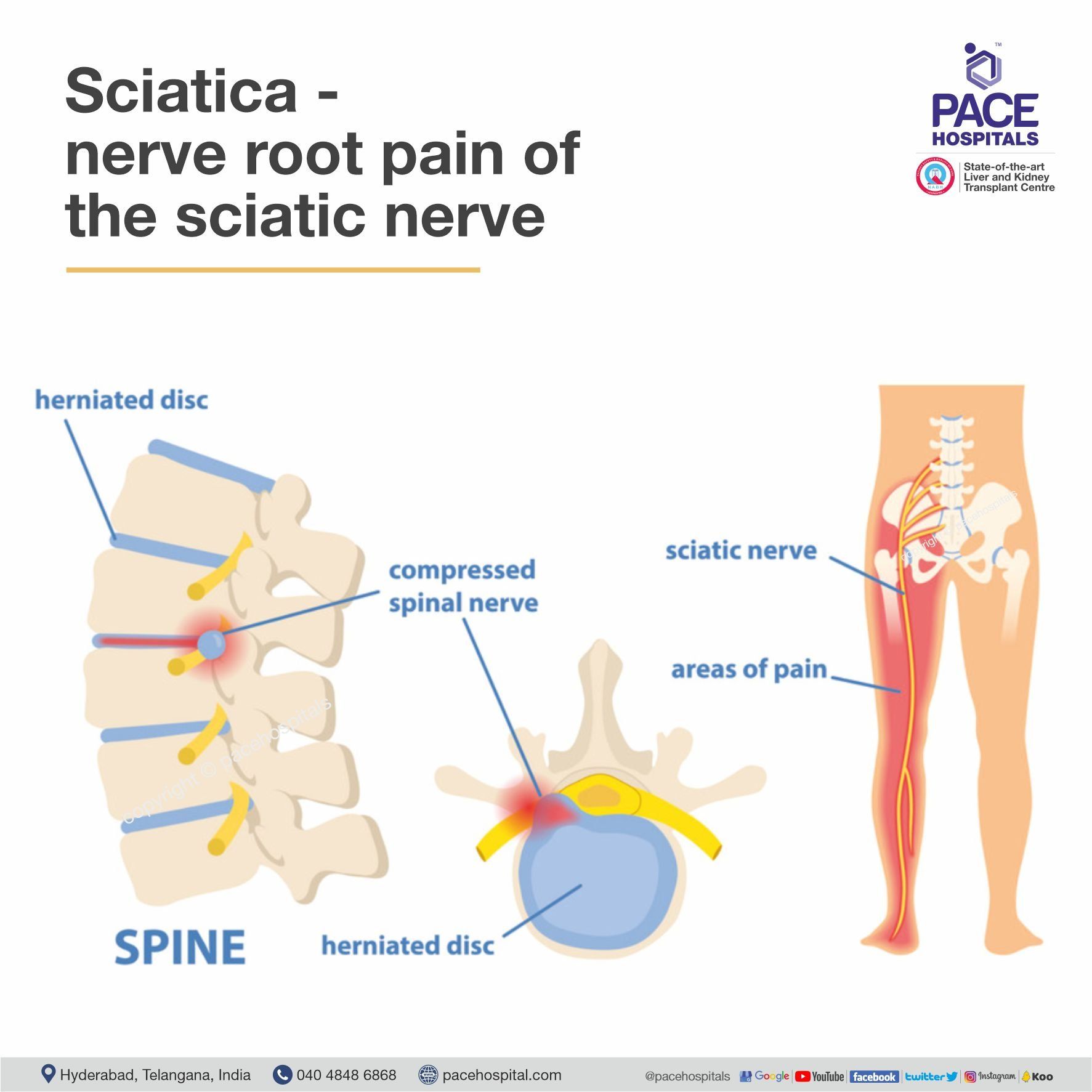
Nerve root pain (usually sciatica)
Nerve root pain is pain that occurs because a nerve coming from the spinal cord is pressed by a prolapsed disc, and is irritated by the inflammation caused by the prolapsed disc. Patients should understand that though the problem is in the back, they will feel pain anywhere along the course of the nerve in addition to back pain. Therefore, patients may feel pain below the knee as far as your calf or foot.
Nerve root pain can range from mild to severe, and it is often worse than the back pain. People often describe nerve root pain as a burning pain. With a prolapsed disc, the sciatic nerve is the most commonly affected nerve. (The term sciatica means nerve root pain of the sciatic nerve.) The sciatic nerve is a large nerve that is made up of several smaller nerves that come out of the spinal cord in the lower back. It travels deep inside the buttock and down the back of the leg.
The irritation or pressure on the nerve next to the spine may also cause pins and needles, numbness or weakness in part of a buttock, leg or foot. The exact site and type of symptoms depend on which nerve is affected.
Cauda equina syndrome - rare, but an emergency
Cauda equina syndrome is a rare serious problem caused by a prolapsed disc where the nerves below the spinal cord are compressed. This syndrome cause low back pain plus:
- Problems with bowel and bladder function (usually inability to pass urine).
- Numbness around the anal and genital region ( Saddle region)
- Weakness in one or both legs.
Do all the people develop symptoms
Research studies have shown that some people have a prolapsed disc without any symptoms. Symptoms mainly occur if the disc prolapse puts pressure or irritates a nerve. This does not happen in all. Some prolapses may be small, or occur away from the nerves and cause minor or no symptoms.
How it progress?
In most of the cases, the symptoms improve over a few weeks. Research studies have shown that the bulged portion of the disc shrink over time. The symptoms tend to ease and, in most cases, go away completely. Only 10-15 % of people will land up in having surgery
Do I need to undergo any tests?
Your doctor will be able to diagnose a prolapsed) disc from the symptoms and by examining you.
Tests such as X-rays or scans may be advised if symptoms persist. In particular, an MRI scan can show the site and size of a prolapsed disc. This information is needed if treatment with surgery is being considered.
Treatment options for a slipped disc or disc prolapse
Physiotherapy and medications:
Usually, 60-70% of prolapsed discs become better on their own by rest, analgesics and a gradual return to activities. Continue with normal activities as far as possible. Activities that cause a lot of pain are avoided. Also, sleep in the most naturally comfortable position on a comfortable surface. The use of hard beds, pillows have also been not advised. You are likely to recover more quickly and are less likely to develop persistent (chronic) back pain if you keep active when you have back pain rather than rest a lot.
Pain killers are required to ease the pain. Paracetamol, Non-steroidal anti-inflammatory drugs like diclofenac or Ibuprofen are preferred. Some people with asthma, high blood pressure, kidney failure, or heart failure may not be able to take anti-inflammatory drugs. The use of oral steroids in some patients can be considered.
Back exercises
Back exercises are very important if you have a prolapsed disc. It can help lessen the pain by strengthening the muscles that support your spine. A physiotherapist can advise you on what exercises help your situation.
Exercise not only reduces the pain of a prolapsed disc but may also reduce the chance of it happening again.
Epidural steroid injections
This is an injection given to your back. It is performed by a specialist. The injection contains local anaesthetic agent and a steroid, which is a very strong anti-inflammatory. It is essentially a long-term painkiller that can give you enough pain relief.
Selective nerve root blocks (SNRB)
This is an injection given around the nerve roots. It is performed in operation theatre under fluoroscopic guidance. The drug given contains a mixture of local anaesthetic agent and steroid.
Both Epidural steroid injection and Selective nerve root blocks are done as day care procedures.
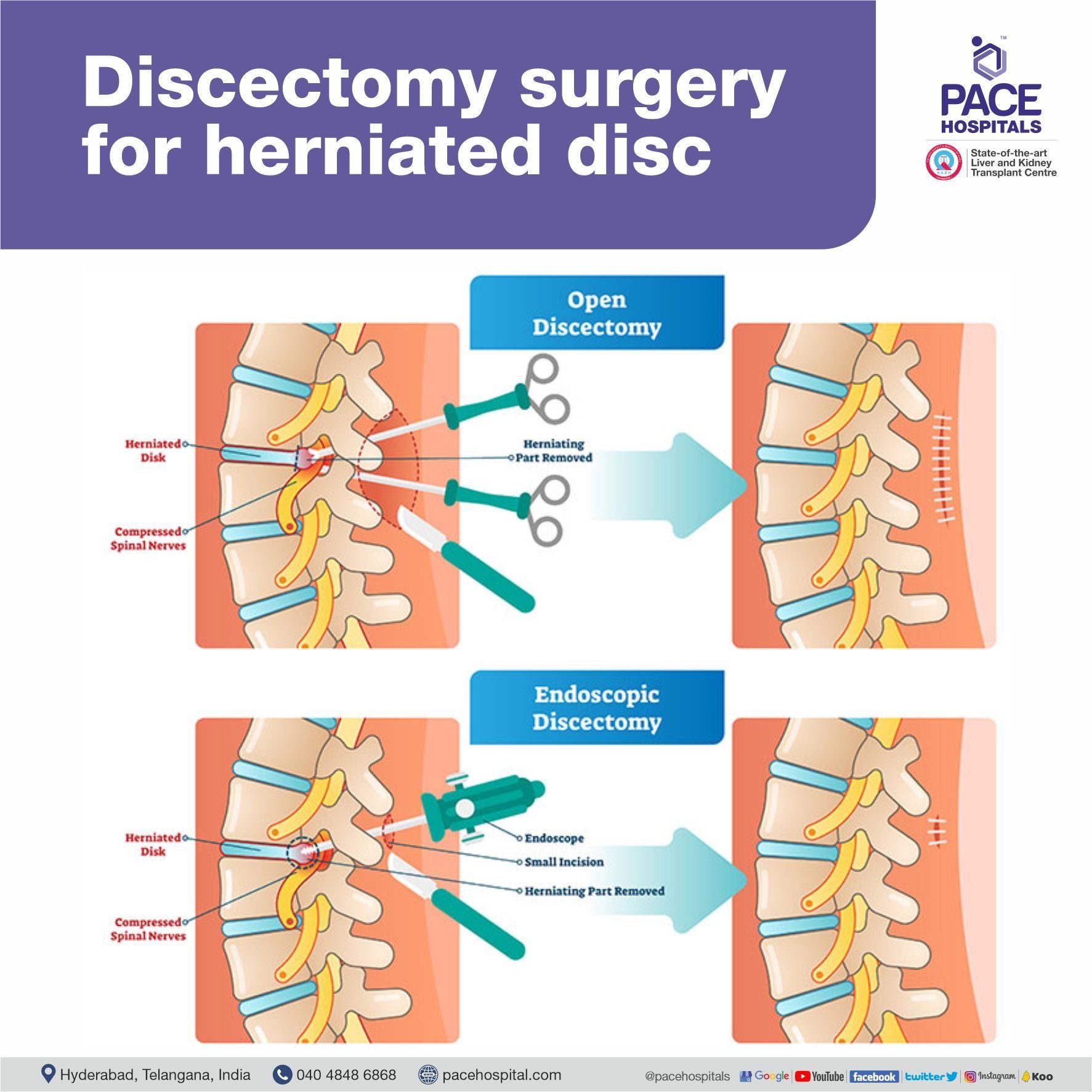
Surgery
Surgery in the form of microsurgery provides the best and immediate pain relief. As a rule, surgery may be considered if the symptoms have not settled after about four weeks. All patients must have an adequate period of conservative treatment of at least 3–6 weeks before surgery is advocated. Relief of radicular pain is the primary surgical indication in most patients. While urgent intervention is required for severe and progressive neurological deficits, there is considerable controversy regarding the relative urgency of surgery in the face of chronic and static neurological deficits. However, an absolute surgical indication is the development of cauda equina compression syndrome matched by relevant MRI findings. Relative indications for surgery include patients who express a preference for early surgery for reasons of intolerance to pain or need for an early return to work.
1. Microsurgery for Disc Prolapse
The aim of surgery is to cut out the prolapsed part of the disc and release the pressure on the nerves through a micro-incision. This often eases symptoms.
The advantages of the microsurgery are:
- Small Incision
- Safety of Nerves
- Less Muscle Injury
- Less Bone Removal
- More Physiological
- Less Scarring
- Less Blood Loss
2. Endoscopic discectomy
Endoscopic discectomy is the recent advance in the treatment of disc prolapse. The prolapsed part of the disc is removed through a small incision of size less than 1 cm. It allows early recovery. It can be done under local anaesthesia and mild sedation.
Can further episodes of disc prolapse be prevented?
Recurrent disc prolapse is seen in 1-5 % of the people. Evidence suggests that the best way to prevent slipped disc is simply to keep active and to exercise regularly. This means general fitness exercise such as walking, running, swimming, etc. Patients should be on regular back strengthening exercises. It is also sensible to be back-aware. For example, do not lift objects when you are in an awkward twisting posture. Stop smoking and taking alcohol. Strict diabetic control. More important reduce weight.
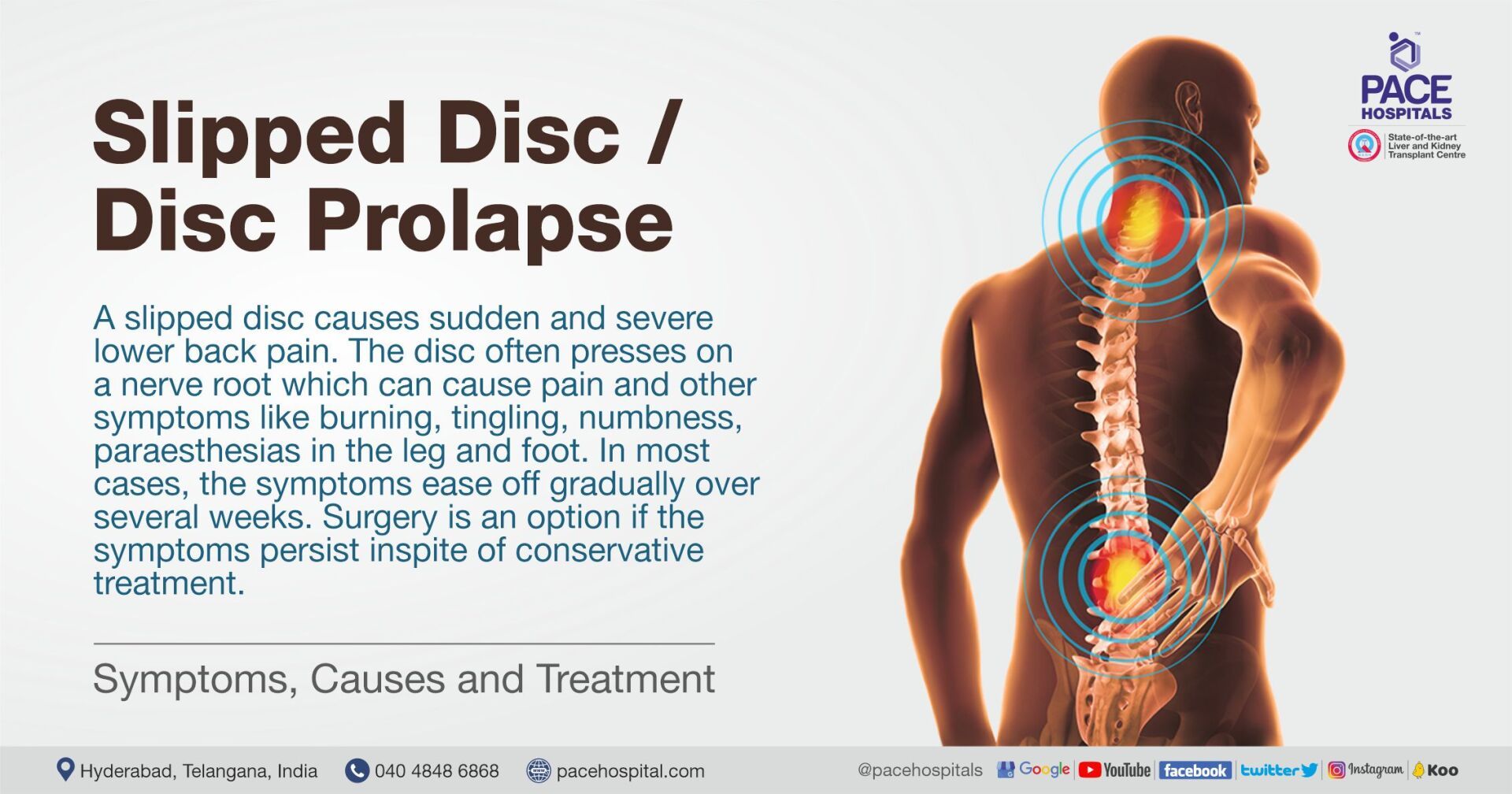
A slipped disc or disc prolapse causes sudden and severe lower back pain. The disc often presses on a nerve root which can cause pain and other symptoms like burning, tingling, numbness, paraesthesias in the leg and foot. In most cases, the symptoms ease off gradually over several weeks. Surgery is an option if the symptoms persist inspite of conservative treatment.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles