Overactive Bladder- Causes, Symptoms, Risk factors, Prevention, Treatment
PACE Hospitals
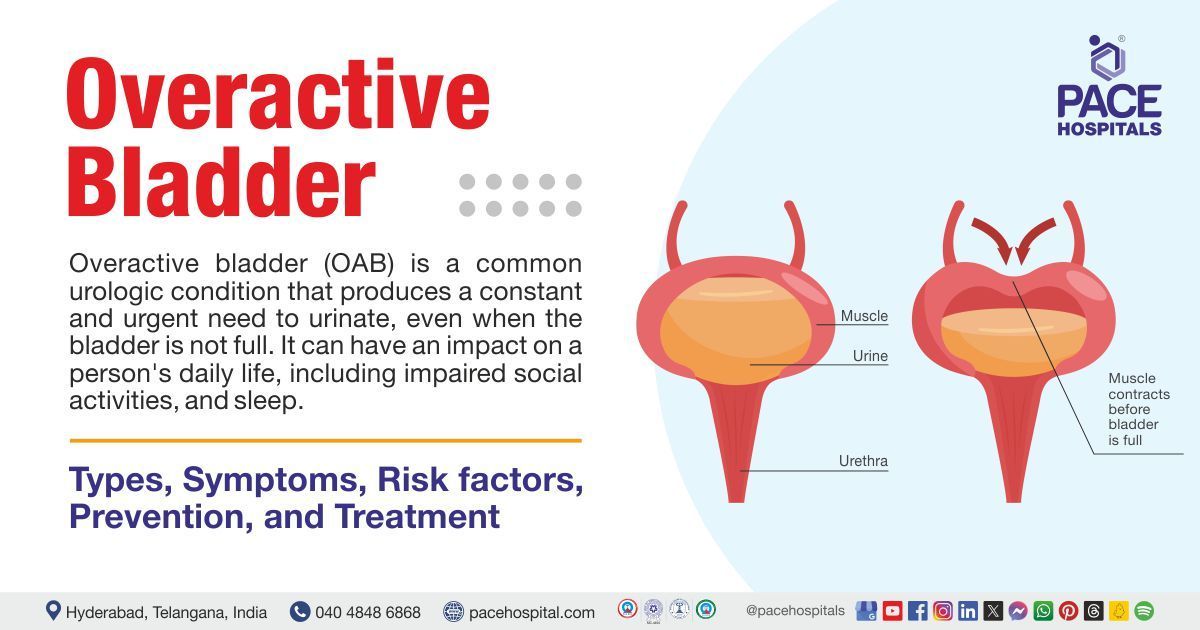
Overactive bladder (OAB) is a medical condition in which people have a strong urge to urinate several times per day and overnight, even if the bladder is not full. The condition is identified if a person urinates eight or more times during the day or at least twice overnight. There is a chance that, about one- third of people with overactive bladder may develop urinary incontinence. (unintentional urine leakage)
In other medical term overactive bladder is also called as hypertonic bladder. An overactive bladder can impose, significant negative impact on quality of life. People suffering from this condition may severely restrict their fluid intake in the hope that it may alleviate the urge to urinate. They may decline social activities if there are no bathrooms nearby, leading to social isolation.
People with overactive bladder often hesitate to consult a urologist, preventing themselves from finding a solution to the problem. Despite many treatment options are available that can improvise the symptoms and quality of life of a patient, under the careful supervision of a
urologist.
Overactive bladder definition
Overactive bladder is a medical condition characterised by a frequent and abrupt need to urinate, which frequently results in involuntary urine leakage (urge incontinence). It is caused by the involuntary contraction of detrusor muscle, that is located on the bladder wall, which can be related to a variety of circumstances such as neurological abnormalities, bladder irritation, or lifestyle.
Overactive bladder meaning
Doctors, named Paul Abrams and Alan Wein coined the phrase "overactive bladder" in 1997 to refer to a conference on lower urinary tract symptoms and treatment. One of the primary goals of the conference was to create a symptom-based definition of overactive bladder (OAB). The guiding ideas were to define this prevalent ailment in a way that would be relevant to both primary-care practitioners and experts, potentially implying immediate, non-invasive therapy without the need for sophisticated, expensive, or intrusive research.
The definition of overactive bladder, which was later formalised in 1999, was "a symptom syndrome suggestive of lower urinary tract dysfunction," specifically determined as "urgency with or without urge incontinence, usually with frequency and nocturia (frequent urination during night) without the presence of a pathological or metabolic underlying disease." This definition was formally endorsed in 2002 by the International Continence Society (ICS).
Prevalence of overactive bladder
Worldwide prevalence of overactive bladder
Overactive bladder (OAB) was estimated to affect 7-27% of men and 9-43% of women, with the condition becoming more common with age. According to several research, OAB was more common in women, particularly when combined with a lack of bladder control.
OAB impacts lakhs of people globally, regardless of ethnicity. The prevalence of OAB rises with age. However, OAB should not be seen as a natural aspect of ageing. Symptoms of OAB are reported 20% of the population aged 70 or older, and 30% of those aged 75 and older. Men typically get OAB slightly later in life than women.
Prevalence of overactive bladder in India
Research carried out in Bengal, involving the subjects from all over India had demonstrated the overall prevalence rate of 15% for overactive bladder, with males at 6.9% and females at 8.6%.
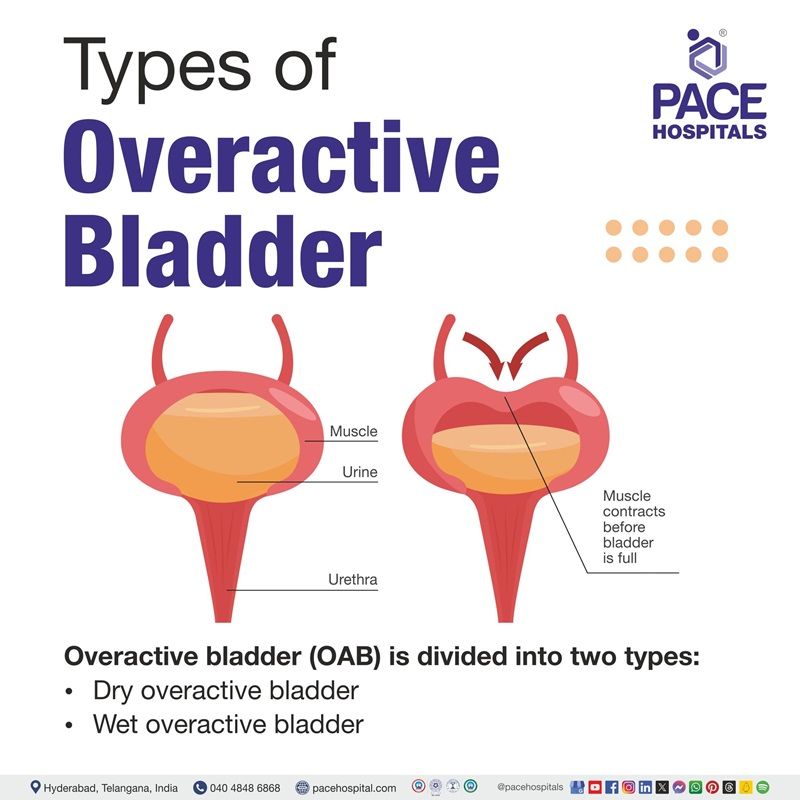
Types of overactive bladder
Overactive bladder (OAB) can be divided into two types:
- Dry overactive bladder
- Wet overactive bladder
Dry Overactive Bladder: This type is characterised by a sudden, urgent desire to urinate repeatedly during the day, with no involuntary urine leaking.
Wet Overactive Bladder: This type is characterised by a sudden need to urinate, which results in involuntary leakage before reaching the toilet. This type of overactive bladder is also known as urge incontinence.
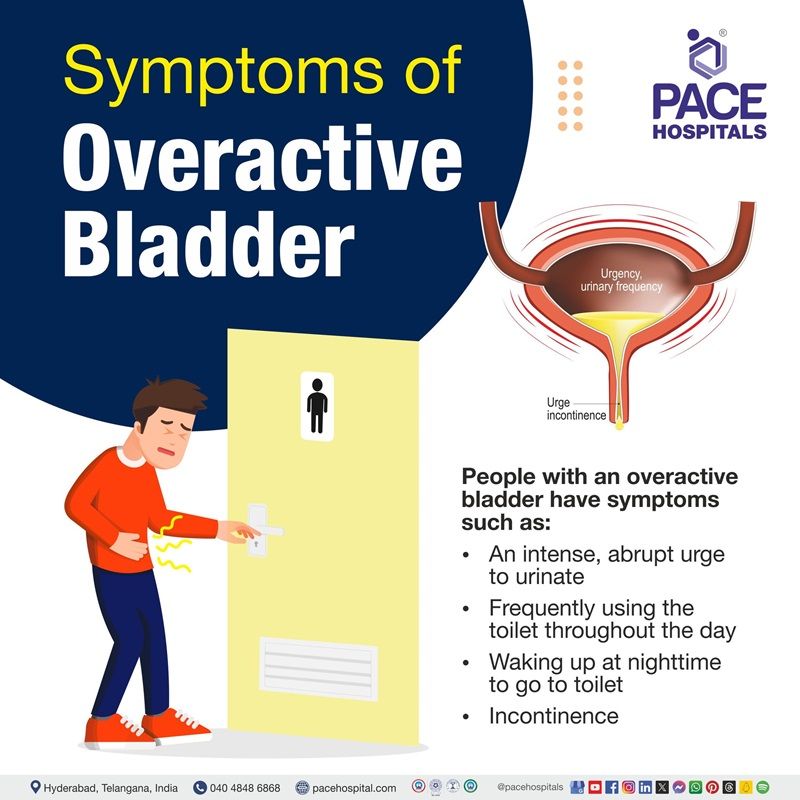
Overactive bladder symptoms
People with an overactive bladder have symptoms such as:
- An intense, abrupt urge to urinate
- Frequently using the toilet throughout the day
- Waking up at nighttime to go to toilet
- Incontinence (accidental loss or leakage of urine, in rare cases)
Overactive bladder causes
Overactive bladder is predominantly a neuromuscular condition where the detrusor muscle contracts abnormally during the storage phase of bladder filling. Regardless of the amount of urine in the bladder, these contractions happen frequently. Numerous factors, both neurogenic and nonneurogenic, can lead to overactive bladder.
Neurologic injuries that may cause overactive bladder include the following:
- Spinal cord injury
- Stroke
Neurologic diseases that may cause overactive bladder include the following:
- Multiple sclerosis (a disorder in which the immune system affects the protective coating of nerves)
- Dementia (a brain disease that can interfere with daily activities and impair cognitive functions like memory, thinking, and reasoning)
- Parkinson disease (a brain disorder that results in difficulties in moving, feeling good mentally, sleeping, having discomfort, and other health problems)
- Medullary lesions (lesion in the bone's medullary canal or in the medulla oblongata, a little but significant portion of the brain stem)
- Diabetic neuropathy (nerve damage due to diabetes)
Detrusor overactivity can arise even in the absence of a neurogenic cause. Contractions can occur spontaneously or as a result of fast bladder filling, postural shifts, walking, or coughing. Because these causes are nonneurogenic, the urgent need to urinate can be suppressed for a few minutes after it is initially detected.
Idiopathic overactive bladder occurs when there are no underlying neurologic, metabolic, or other causes of overactive bladder, as well as conditions that may mimic overactive bladder, such as urinary tract infection (UTI), bladder malignancy (cancer), bladder stones, bladder inflammation, or bladder outlet obstruction.
Certain drugs may cause symptoms of overactive bladder. Diuretics can cause urge incontinence because they increase bladder fullness, which stimulates the detrusor. Certain drugs of class muscarinic agonists can also cause urge incontinence because it stimulates bladder smooth muscle contraction.
Heart failure, as well as peripheral venous and vascular disorders, can all contribute to overactive bladder symptoms. During the day, such people accumulate surplus fluid in dependent postures (their feet and ankles). When they recline to sleep, much of this fluid is mobilised and boosts renal output, resulting in increased urine production. Many of these individuals experience increased nocturia, which presents as an overactive bladder. Only in rare circumstances is it impossible to determine a precise cause (idiopathic overactive bladder).

Risk factors of overactive bladder
Overactive bladder (OAB) can be influenced by several risk factors. Here are some key ones:
- Aging
- Menopause
- Prostate enlargement
- Neurological disorders
- Caffeine consumption
- Smoking
- Obesity and higher body mass index (BMI)
- Genetics
- Irritable bowel syndrome
- Depression and anxiety
Aging: With aging, the wall of the bladder is weakening. The bladder wall changes, the elastic tissue stiffens, and the bladder becomes less flexible. The bladder can no longer hold as much urine as it previously could.
Menopause: Hormonal changes during menopause can raise the risk of overactive bladder (OAB), a condition characterised by a sudden and persistent need to urinate. This is because oestrogen levels decline after menopause, which leads to weaker pelvic floor muscles, more sensitive bladder tissue, and less flexible bladder epithelium.
Prostate enlargement: In men, an enlarged prostate, also known as benign prostatic hyperplasia (BPH), can exert pressure on the bladder and urethra, making it difficult for urine to escape. This may cause the bladder to work harder and become hyperactive, resulting in an urgent desire to urinate.
Neurological disorders: Overactive bladder (OAB) is a risk associated with neurological conditions. These diseases can harm the brain or spinal cord, disrupting connections between the brain and bladder. Neurologic conditions that are predominant risk factors for overactive bladder include:
- Multiple sclerosis
- Parkinson’s disease
- Spinal cord injury
- Stroke
Caffeine consumption: There have been cases reported of overactive bladder due to caffeine consumption. Caffeine can irritate the bladder, causing the body to generate more urine. This can increase the bladder's sensitivity to little amounts of urine.
Smoking: Smoking can irritate the bladder, resulting in frequent urination and coughing spasms, which can lead to urine dripping.
Obesity and higher body mass index (BMI): Obesity and being overweight can raise the chance of developing an overactive bladder (OAB) because excess weight imposes pressure on the bladder.
Genetics: Research studies have demonstrated that genetics can increase the possibility of developing an overactive bladder. A 2011 study showed people may be more susceptible to develop overactive bladder if other members of their family have bladder control issues.
Irritable bowel syndrome: Some studies suggest a link between irritable bowel syndrome (IBS) and overactive bladder (OAB), which can cause people to feel an urge to urinate more frequently or urgently.
Depression and anxiety: Depression and other mental health disorders, such as anxiety, can cause overactive bladder (OAB). In fact, over 30% of individuals with overactive bladder also suffer from depression, and research has indicated that people with depression and anxiety are less likely to have remission of overactive bladder symptoms. People with overactive bladder and depression may experience more severe urine incontinence symptoms, lowering their quality of life.
Complications of overactive bladder
If not treated properly, overactive bladder (OAB) can cause a variety of complications such as:
Decreased physical activity: Physical activity promotes overall health and may avoid future problems (bladder control). However, certain activities, such as sprinting, leaping, or rapid walking, may trigger leakage in people with overactive bladder.
Emotional distress: Untreated bladder disorders might interfere with a person's daily activities. People might avoid activities they previously enjoyed. They may quit attending movies, meetings, or activities because they do not want to use a restroom while participating in an activity. These lifestyle changes can cause depression or social anxiety.
Intimacy problems: Some people may avoid intimacy as they are afraid to leak urine during intercourse.
Sleep disturbances: The presence of frequent urination during the nighttime (nocturia) may lead to consequences such as sleep disturbances
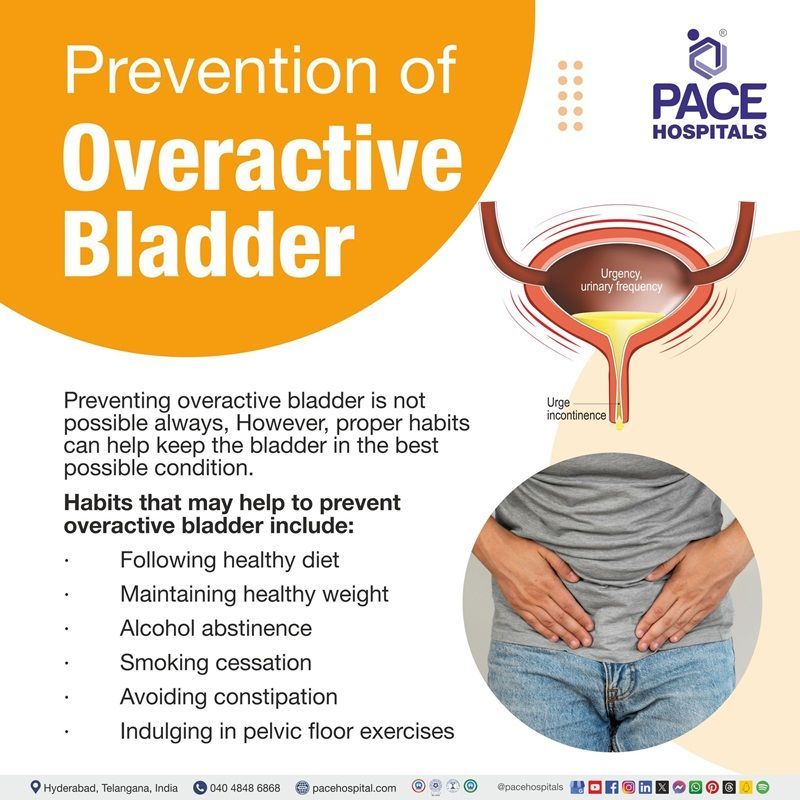
Prevention of overactive bladder
Preventing overactive bladder is not possible always, However, proper habits can help keep the bladder in the best possible condition.
Healthy habits that may help to prevent overactive bladder include:
- Following healthy diet: Healthy diet may prevent bladder problems by preventing medical conditions such as diabetes (high blood glucose) and obesity (excess body weight)
- Maintaining healthy weight: Being overweight can weaken the pelvic floor muscles and induce bladder problems owing to the pressure of fatty tissue on the bladder.
- Alcohol abstinence: Alcohol consumption can induce diuretic (removes water from the body) like effect. Cutting down alcohol may alleviate overactive bladder symptoms.
- Smoking cessation: Cigarette compounds, such as nicotine and tar, can irritate the bladder lining, causing irritation and sensitivity. Smoking cessation can improve bladder health and overall health.
- Avoiding constipation: Constipation can lead to overactive bladder (OAB) because the colon expands with faeces and strains the bladder, making it difficult to hold the urine. So, avoiding constipation may help to prevent bladder problems.
- Indulging in pelvic floor exercises: Pelvic floor muscles help the bladder to hold urine. Pelvic exercises, which are also known as Kegel exercises, can strengthen these muscles and prevent urine from spilling out when people laugh, cough, sneeze, or lift. These exercises are beneficial for both men and women.
Overactive bladder diagnosis
Diagnosing overactive bladder (OAB) often requires many measures to obtain an appropriate assessment. Patients who show urinary urgency and frequency can be assessed using:
- Standardised questionnaires
- Bladder diaries
- Complete history
- Physical examination
- Simple laboratory tests
- Urinalysis
- Postvoid residual
Patients with more complex symptoms may require urodynamic testing to confirm the diagnosis of overactive bladder or detrusor overactivity.
Urodynamic tests that may be used to diagnose overactive bladder include:
- Uroflowmetry
- Filling cystometry
- Pressure flow studies (voiding cystometry)
- Urethral pressure profilometry
- Abdominal leak point pressure
Overactive bladder treatment
Overactive bladder (OAB) can be very disturbing, but there are various effective treatments available. Here are some common approaches:
- Behavioural therapy
- Pharmacological treatment
- Combination therapy
- Surgical interventions
Behavioural therapy
It is also known as behavioural modification, is a type of treatment that seeks to enhance bladder control by changing an individual's activities or surroundings. The types of behavioural therapy include the following:
- Education
- Dietary and lifestyle modification
- Bladder training
- Pelvic floor muscle therapy (PFMT)
- Self-monitoring with bladder or voiding diaries
Pharmacological treatment
Overactive bladder medication that may be advised by the urologist include:
- Anticholinergics
- Beta 3 agonists
- Anti-depressants
- Neuromuscular blockers
- Hormones
Combination therapy
Since most patients do not attain total cure with a single type of treatment alone, hence many practitioners mix two types of treatment to manage overactive bladder.
Surgical interventions
- Augmentation cystoplasty
- Selective bladder denervation
- Urinary diversion
- Neuromodulation
- Non-invasive electrical stimulation
- Sacral neuromodulation
- Percutaneous stimulation of the tibial nerve
Investigational treatments of significant interest that can be promising to treat overactive bladder include the following:
- Neurokinin receptor antagonists
- Alpha-adrenoceptor antagonists
- Nerve growth factor inhibitors
- Stem cell–based therapies
- Novel antimuscarinic agents
- Combination therapies with beta3-adrenoceptor agonists or muscarinic agonists
- A unique vaginal delivery formulation for an antispasmodic
- Novel beta3-adrenoceptor agonists
- Gene therapy
Difference between Overactive bladder and Urge incontinence
Overactive bladder vs Urge incontinence
| Aspect | Overactive bladder | Urge incontinence |
|---|---|---|
| Definition | A condition characterized by a sudden, intense urge to urinate, often with increased frequency. | A condition where the urge to urinate leads to involuntary leakage of urine. |
| Symptoms | Frequent urination, sudden urges to urinate, nocturia (frequent urination at night). | Involuntary urine leakage following an urgent need to urinate. |
| Occurrence | Can occur without incontinence. | Often occurs as a symptom of OAB but can also occur independently. |
| Causes | Nerve signals between the bladder and brain are not coordinated properly. | Often caused by OAB but can also result from other conditions affecting bladder control. |
| Diagnosis | Based on symptoms, urination diary, pelvic examination, tests for infections, bladder scans. | Based on symptoms, urination diary, pelvic examination, tests for infections, bladder scans. |
| Treatment | Lifestyle changes, bladder training, medications, pelvic floor exercises. | Similar to overactive bladder: lifestyle changes, bladder training, medications, pelvic floor exercises. |
| Impact on daily life | Can disrupt daily activities due to frequent urination and urgency. | Can cause embarrassment and inconvenience due to involuntary leakage. |
Frequently Asked Questions (FAQs) on Overactive bladder
Is overactive bladder painful?
Yes, an overactive bladder can be painful and uncomfortable. An Overactive bladder occurs when the bladder contracts spontaneously, forcing urine out at the incorrect time. This can result in spasms, which is described as cramping pain.
Is there any over-the-counter medicine for overactive bladder?
Yes. Antispasmodic drugs are available over the counter that can ease the symptoms of overactive bladder. Nevertheless, consulting a urologist is necessary before self-assessment of the condition, because antispasmodic class of medications has potential adverse effects.
Can overactive bladder go away on its own?
No, an overactive bladder (OAB) will not go away on its own. In fact, if left untreated, symptoms can worsen, lowering the quality of life. Over time, the muscles in the bladder that control urine may weaken and the tissues in the pelvic floor can thin .
How to cure overactive bladder?
Fortunately, there are solutions to this problem. There are numerous techniques to treat overactive bladder, including medication, behavioural modifications and a combination of the two. Consulting a urologist for a thorough evaluation and carefully obeying their instructions will help to cure overactive bladder symptoms and resume the normal lifestyle.
Which vitamins help overactive bladder?
Vitamin D supplements could be beneficial to prevent or alleviate overactive bladder (OAB) symptoms. According to several studies, patients with OAB have decreased vitamin D levels, and vitamin D insufficiency increases the risk of OAB and urine incontinence.
How to control the urinary bladder naturally?
Practicing pelvic floor muscle exercises, often known as Kegel exercises, helps to keep urine in the bladder. Daily workouts can strengthen these muscles, which can assist in avoid urine from leaking when someone sneezes, coughs, lifts, laughs, or has an unexpected urge to urinate.
What is the pathophysiology of overactive bladder?
The pathophysiology of overactive bladder is multifactorial. An Increase in muscarinic receptor sensitivity may cause overactive bladder. Acetylcholine leakage from the parasympathetic nerve terminal may cause micromotion of the detrusor muscle, activating sensory afferent fibres and producing a sense of urgency. Sensory afferent nerves are also said to play a role in the development of overactive bladder.
What is the main cause of overactive bladder?
Overactive bladder can occur due to improper signals between the bladder and brain. The impulses from the brain may tell the bladder to empty even if it is not full. This condition can also occur when the muscles in the bladder are overactive. This indicates that the bladder muscles contract to pass urine before it is full.
What is overactive bladder syndrome?
Overactive bladder (OAB) syndrome is a common problem marked by urine urgency, with or without urgency incontinence, frequency, and nocturia (frequent urination at nighttime) in the absence of any underlying pathology. The clinical diagnosis is based on symptoms reported by the patient. Currently, there are numerous treatments available for the management of overactive bladder.
Can overactive bladder cause burning?
The spasm in the bladder could force urine from the bladder, resulting in leakage. When this occurs, the condition is known as urge incontinence or overactive bladder. People who have experienced such spasms describe them as cramping pains or burning sensations.
What medications cause overactive bladder?
Medications that have the potential to cause overactive bladder as an adverse effect (unintended effect) may include diuretics, muscle relaxants, and sedatives, narcotics, antihistamines, alpha-adrenergic antagonists .
Related articles
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles