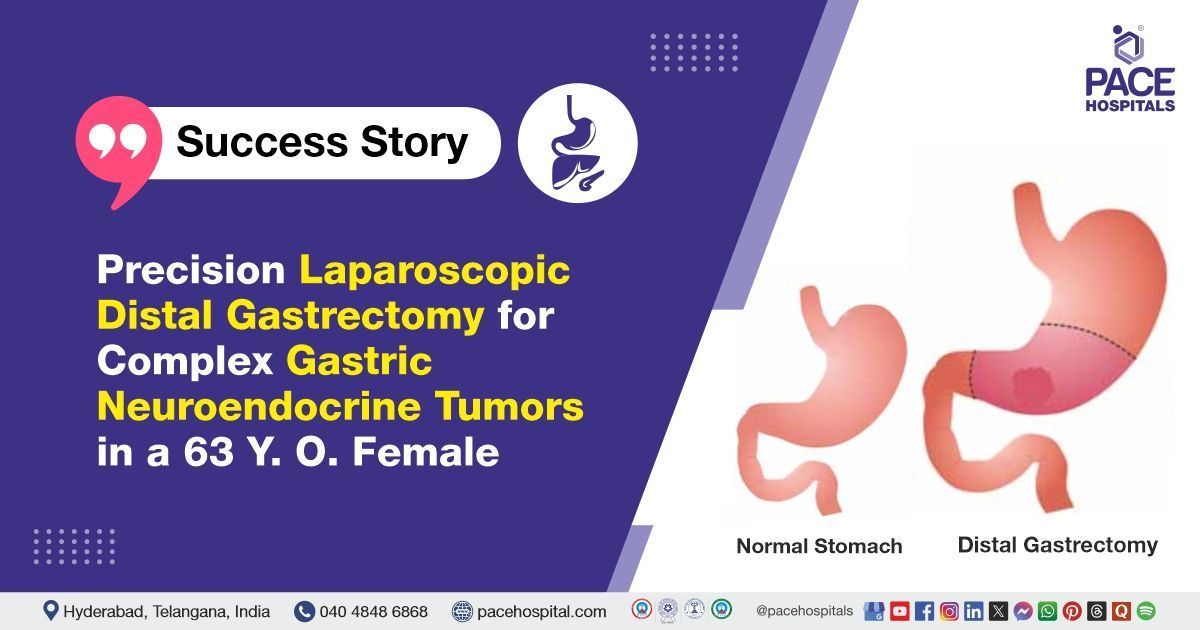
Precision Laparoscopic Distal Gastrectomy for Complex Gastric NET in a 63-Y.O. Female
PACE Hospitals
The PACE Hospitals' Surgical Gastroenterologist team successfully performed a laparoscopic distal gastrectomy on a 63-year-old female patient suffering from gastric neuroendocrine tumors (NETs), aiming to achieve complete tumor resection and disease control, thereby relieving her symptoms and preventing further progression.
Chief Complaints
A 63-year-old male patient with a
BMI of 23.4 presented to the Surgical Gastroenterology Department at
PACE Hospitals, Hitech City, Hyderabad, with chronic epigastric burning and dyspepsia. Investigations revealed grade I (early-stage) neuroendocrine tumors (a rare type of stomach tumor), along with elevated levels of chromogranin A and gastrin, indicating increased hormone activity. The DOTANOC PET scan showed two abnormal spots on the inner curve of the stomach, which were likely due to tumors. So, the patient was referred for further treatment.
Past History
The patient had previously undergone an
upper gastrointestinal endoscopy (UGIE), which revealed the presence of sessile polyps along the lesser curvature of the stomach.
Diagnosis
Upon admission to PACE Hospitals, the patient underwent a comprehensive review of his medical history, followed by a detailed clinical examination by the Surgical Gastroenterology team. Based on these findings and the patient's history, gastric neuroendocrine tumors (NETs) were strongly suspected.
Since the patient was referred to PACE Hospitals with a preliminary diagnosis of gastric neuroendocrine tumors (NETs) made at an outside facility, the Surgical Gastroenterology team began by thoroughly reviewing all prior investigations, including histopathology, imaging, and biochemical reports. However, to ensure diagnostic accuracy and guide definitive treatment, they opted to reassess the case comprehensively using a stepwise and multidisciplinary approach.
The patient’s previous upper gastrointestinal endoscopy (UGIE) had revealed sessile polyps along the lesser curvature of the stomach, raising suspicion for gastric NETs. To confirm this, a biopsy with histopathological examination had already been performed externally, providing initial evidence of neuroendocrine tumor features. However, since treatment decisions require precise tumor grading and assessment of biological behavior, further confirmation was essential.
At PACE Hospitals, serum biomarkers—particularly gastrin and chromogranin A-levels—were reviewed. Both were significantly elevated, a finding consistent with Type I gastric NETs, which are often associated with chronic atrophic gastritis and hypergastrinemia. Elevated chromogranin A-levels further supported the neuroendocrine origin of the tumor and provided a baseline for monitoring disease progression and response to treatment.
To obtain a more detailed characterization of the tumor, the team utilized immunohistochemistry (IHC). IHC staining for markers like chromogranin A, synaptophysin, and Ki-67 helped in confirming the neuroendocrine nature of the tumor and determining its proliferative index and grade, which are critical for planning treatment and predicting prognosis.
Additionally, advanced imaging was deemed necessary. A DOTANOC PET scan was performed, which identified two tracer-avid foci along the lesser curvature of the stomach, indicating the presence of somatostatin receptor-positive NET lesions. To further evaluate the depth and local spread of the tumors, endoscopic ultrasound (EUS) was considered, which provides high-resolution imaging of the stomach wall and adjacent structures, crucial for accurate staging.
This comprehensive re-evaluation ultimately confirmed the diagnosis of grade I gastric neuroendocrine tumors, localized to the lesser curvature, and guided the decision to proceed with laparoscopic distal gastrectomy.
Based on the confirmed diagnosis, the patient was advised to undergo Gastric Tumor Treatment in Hyderabad, India, under the expert care of the Surgical Gastroenterology Department to address the tumor burden, alleviate symptoms, and prevent potential complications or progression of the disease.
Medical Decision Making (MDM)
Following a detailed consultation with Consultant Surgical Gastroenterologist Dr. Suresh Kumar S and input from other specialists, a thorough multidisciplinary evaluation was conducted to determine the most appropriate treatment strategy for the patient. The team carefully analyzed the patient’s medical history, clinical symptoms, and all prior diagnostic results—including upper gastrointestinal endoscopy, histopathology, imaging studies, and biochemical markers. This systematic and collaborative approach ensured a clear understanding of the patient’s condition, leading to the development of a personalized treatment plan tailored to his confirmed diagnosis of gastric neuroendocrine tumors and overall health status.
Based on their expert assessment, it was concluded that a Laparoscopic Distal Gastrectomy would be the most effective surgical procedure to address the patient’s condition. This decision was made after evaluating the extent and location of the gastric neuroendocrine tumors, particularly along the lesser curvature, as well as the patient’s overall health status and previous clinical findings.
Surgical Procedure
Following the decision, the patient was scheduled for a Laparoscopic Gastrectomy Surgery in Hyderabad at PACE Hospitals, under the expert supervision of the Surgical Gastroenterology Department.
Laparoscopic distal gastrectomy is a minimally invasive surgical procedure used to remove the lower stomach portion, often used to treat conditions including gastric cancer, peptic ulcer disease, or multiple gastric neuroendocrine tumors. The procedure uses small incisions and a camera-guided laparoscope to precisely remove the affected stomach while preserving surrounding structures. It offers advantages such as reduced postoperative pain, shorter hospital stays, faster recovery, and smaller scars.
Under general anaesthesia, the patient underwent a laparoscopic distal gastrectomy. During the procedure, the distal portion of the stomach was carefully mobilized, and both the greater and lesser curvatures were meticulously skeletonized to facilitate safe and complete resection. For effective vascular control, the right gastroepiploic artery (RGEA), right gastric artery (RGA), and left gastric artery (LGA) were double ligated and subsequently divided.
To safely separate the duodenum, a surgical stapler was fired at the D1 level. Following intraoperative endoscopic confirmation of the neuroendocrine tumors (NETs) located along the lesser curvature, the proximal stomach was divided using a stapling device, thereby completing the resection of the diseased portion.
To restore gastrointestinal continuity, an antecolic gastrojejunostomy (GJ) was constructed, enabling smooth passage of food from the stomach remnant to the small intestine.
Postoperative Care
The patient’s postoperative recovery was smooth and uneventful. He was gradually initiated on a liquid diet, which he tolerated well without any complications. Postoperative ultrasound screening revealed no abnormal fluid collections, and his clinical condition remained stable throughout the recovery period. Overall, the patient showed satisfactory progress following the laparoscopic distal gastrectomy.
Discharge Notes
As the patient showed good postoperative progress with stable vital signs and no complications, the medical team decided to proceed with discharge. He was discharged in a hemodynamically stable condition, with comprehensive instructions for continued care. These included dietary modifications suited to his postoperative status, strict adherence to prescribed medications, proper wound care, and scheduled follow-up appointments to closely monitor his recovery and ensure optimal long-term outcomes.
Discharge Medications
Upon discharge, the patient was prescribed a proton pump inhibitor (PPI) to reduce gastric acid secretion and promote healing, opioids for pain management during the early postoperative period, prokinetic agents to support gastric motility, mineral supplements to address potential deficiencies, and laxatives to prevent constipation, a common side effect of opioid use.
Dietary Advice
The patient was advised to follow a liquid diet for one week to aid in the healing process and allow for gradual adjustment of the digestive system after a laparoscopic distal gastrectomy. This dietary approach helps prevent strain on the stomach, promotes faster recovery, and reduces the risk of complications by easing the transition to solid foods while the digestive tract heals.
Emergency Care
The patient was informed to contact the Emergency ward at PACE Hospitals in case of any emergency or development of symptoms like fever, abdominal pain, or vomiting.
Review and Follow-up Notes
The patient was advised to return for a follow-up appointment with the Surgical Gastroenterologist at PACE Hospitals, Hyderabad, after five days, bringing the histopathologic examination (HPE) report for further evaluation and management. This follow-up visit is crucial to assess the tumor’s characteristics, ensure proper healing, and guide any necessary adjustments in treatment, such as dietary modifications or medication changes, based on the histopathological findings.
Conclusion
This case highlights the effectiveness of minimally invasive laparoscopic techniques (specifically laparoscopic distal gastrectomy) in performing Gastric Neuroendocrine Tumors Treatment in Hyderabad, India, enabling successful tumor removal while preserving the surrounding healthy liver tissue, promoting quicker recovery, and preserving the integrity of the stomach and nearby structures.
Enhancing Laparoscopic Distal Gastrectomy for Gastric Neuroendocrine Tumours with DOTANOC PET Imaging
DOTANOC PET imaging plays a vital role in enhancing the accuracy and precision of laparoscopic distal gastrectomy for patients with gastric neuroendocrine tumors (NETs). This advanced imaging technique allows for the precise localisation of tumors, even in challenging cases where they may be small or difficult to detect using traditional methods. By assessing the metabolic activity of the tumors, DOTANOC PET provides valuable insights that guide surgeons in selecting the most effective surgical approach. Integrating this imaging technology with minimally invasive surgery not only improves tumor removal but also helps preserve healthy tissue, reducing the risk of recurrence. Ultimately, DOTANOC PET imaging aids the surgical gastroenterologist/surgical gastroenterology doctors in achieving better surgical outcomes and faster recovery for patients undergoing laparoscopic gastrectomy for gastric NETs.
Share on
Request an appointment
Fill in the appointment form or call us instantly to book a confirmed appointment with our super specialist at 04048486868
Appointment request - health articles
Recent Articles